West Coast Retina
Case of the Month
June, 2013
Presented by Sara Haug, MD, PhD
A 33 year-old white woman with decreased vision in her left eye, referred for evaluation of possible mass

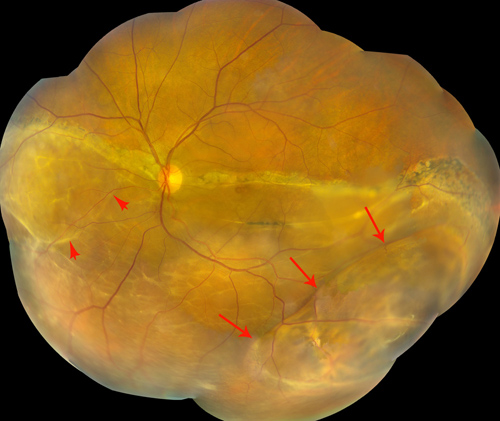
Figure 1: Color fundus photograph montage of the left eye. There is a prominent pigmented demarcation line with an inferior retinal detachment. A mass-like effect is noted inferotemporally (large arrows) and a retinal macrocyst nasally (small arrows).
Case History
A 33 year-old woman presented with decreased vision in her left eye discovered during a vision test required for renewal of her driver’s license. The patient was in good health.
Visual acuity was 20/25 in the right eye and 20/200 in the left eye. Intraocular pressures were 12mm Hg and 10mm Hg in the right and left eye, respectively. Anterior segment examination was normal bilaterally. Posterior segment examination in the right eye was normal. In the left eye, there was a prominent demarcation line through the macula and nasal to the disc with an inferior retinal detachment (Figure 1). In the inferotemporal quadrant, a mass-like effect was noted with a peculiar branching orange-pigmented appearance. The pigment appeared to be present on the inner layer of the elevated retina (Figure 1, large arrows and Figure 2). A macrocyst was also apparent nasally (Figure 1, small arrows) and areas of subretinal fibrosis.
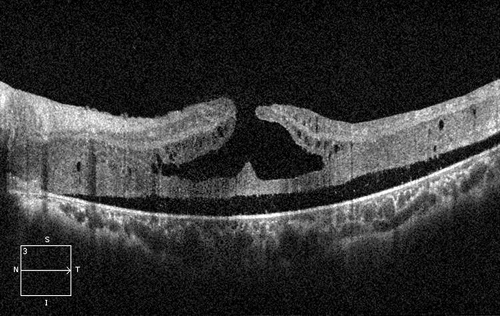
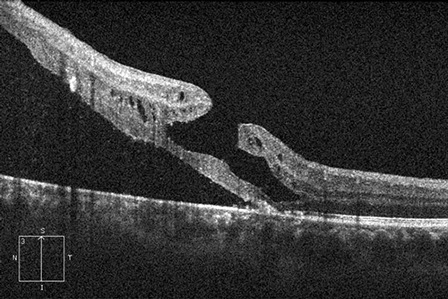
Spectral Domain optical coherence tomography (SD-OCT) performed through the fovea showed a lamellar hole and macula-off inferior retinal detachment (Figure 3). Fluorescein angiography showed areas of hyper- and hypofluorescent changes consistent with chronic retinal detachment. Inferotemporally there were areas of non-perfusion and one small area of expanding hyperfluorescence, concerning for neovascularization. No evidence of intrinsic vascularity was observed within the area suspicious for a mass (Figures 4 and 5).
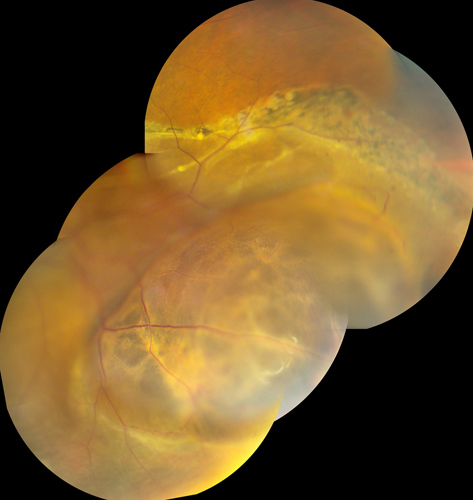
Figure 2: Color fundus montage of the inferotemporal lesion of the left eye. There is a branching orange pigment pattern in the area of more highly detached retina.
A
B
Figures 3A and B: Optical coherence tomography (OCT) images through the fovea of the left eye. Figure 3A, a horizontal scan through the shows detachment of the sensory retina and a lamellar hole. The vertical scan through the fovea, fig 3B, shows the retinal detachment extending just through the fovea with the overlying lamellar hole.
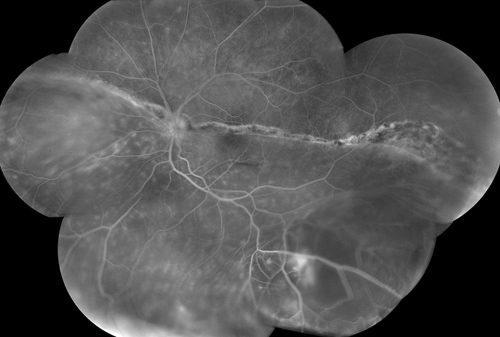
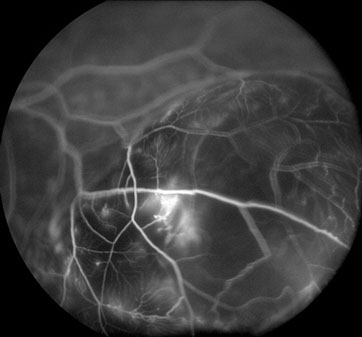
Figure 4: Fluorescein angiogram montage of the left fundus. Mutliple areas of hyperfluorescence and hypofluorescence are seen in the area of retinal detachment. Inferotemporally there is evidence of nonperfusion as well as a small area of expanding hyperfluorescence, likely representing an area of neovascularization.
Figure 5: Fluorescein angiogram, mid-phase, of the inferotemporal fundus of the left eye. There is a bright area of hyperfluorescence within the mass-like area of detachment as well as areas of nonperfusion. No intrinsic vascularity is seen within the apparent mass.
What is your Diagnosis?
Differential Diagnosis
The patient had a chronic macula-off inferior retinal detachment. A possible mass was noted with a pigmentation pattern mimicking orange lipofuscin pigment overlying a choroidal melanoma. Other conditions in the differential include other choroidal masses, such as metastasis or hemangioma, a vasoproliferative tumor, retinal schisis, or pigmentary and cystic changes associated with a chronic retinal detachment.
B-scan ultrasonography was performed through both the inferotemporal (Figure 6) and nasal (Figure 7) lesions showed cystic cavities within the retina, but no evidence of a mass – consistent with the diagnosis of multiple retinal macrocysts in the setting of chronic retinal detachment. The patient was scheduled for retinal detachment repair, including scleral buckle and pars plana vitrectomy.
A noteworthy finding in this patient was the peculiar orange branching pigment that appeared to be present within the inferotemporal cystic space. Clinically, the pigment appeared to be present on the underside of the inner cyst, rather than present under the retina. It is uncertain how this pigment migrated to this area. If a break were present within the retinal layers to allow for pigment migration, one would think that the retinal cyst would simply collapse or have not formed.
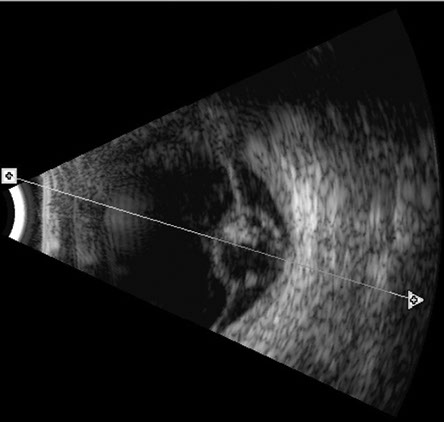
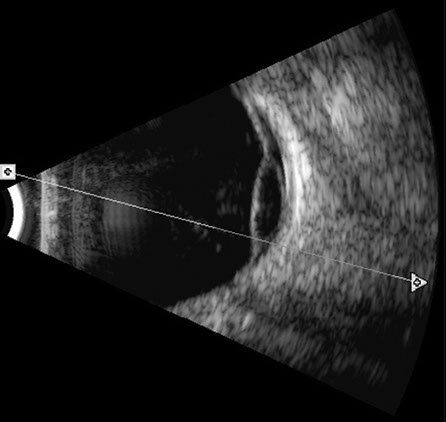
Figure 6: B-scan ultrasonography of the inferotemporal retinal mass-like lesion. The retinal is detached and a hypoechoic cavity representing a large cystic space is observed. No masses are detected.
Figure 7: B-scan ultrasonography of the nasal lesion of the left eye. The retina is detached with a hypoechoic cavity, representing a retinal macrocyst.
Discussion
Long-standing, chronic retinal detachment can cause changes in retinal anatomy such as retinal pigmentary atrophy, demarcation lines, retinal macrocyst formation, and neovascularization.1-6 Retinal macrocysts were first described in depth by Hagler and North in 1967, who emphasized their occurrence in the setting of chronic retinal detachment.1 These authors reviewed 1,112 eyes and found a 3% incidence of macrocysts. The macrocysts were specifically associated with retinal detachments of more than six months duration, and tended to be both well-circumscribed and located at the equator.1 Subsequent reports described retinal macrocysts associated with retinal dialysis and extending to the ora serrata.2-4 One series of 196 patients with retinal dialysis found that 11% developed macrocysts, and only patients with detachments of one year or more had macrocysts.4
Retinal macrocysts occur in the outer plexiform layer of the retina, hypothesized to be due to the loose synaptic connections and watershed area of retinal circulation in this layer.7 Macrocysts are usually well-demarcated and have a smooth surface. Furthermore, retinal macrocysts typically do not require any particular attention during surgical repair of the detachment and spontaneously resolve with retinal reattachment. However, when the macrocyst is localized at or near a retinal break it can prevent retinal reattachment. Therefore, surgical drainage of the cyst in these cases is advocated.2 As an alternative to surgical drainage, particularly when placing a scleral buckle, a recent case report advocated using an Nd:YAG laser to drain the cyst prior to surgery to aid in reattachment with good results.7
Take Home Points
- Retinal macrocysts are commonly associated with long-standing retinal detachments from retinal dialysis
- Macrocysts typically do not require any particular treatment and tend to resolve with retinal reattachment.
- If a retinal macrocyst is located near a retinal break or dialysis, surgical drainage is indicated. Nd:YAG laser disrupt the cyst is a possible alternative to surgical drainage.
Want to Subscribe to Case of the Month?
References
- Hagler WS, North AW. Intraretinal macrocysts and retinal detachment Trans Am Acad Ophthalmol Otolargyngol 1967;71:422-454.
- Marcus DF, Aaberg TM. Intraretinal macrocysts in retinal detachment. Arch Ophthalmol 1979;97:1273-1275.
- Hagler WS. Retinal dialysis: a statistical and genetic study to determine pathogenic factors. Trans Am Ophthalmol Soc 1980;78:686-733.
- Zion VM, Burton TC. Retinal dialysis. Arch Ophthalmol 1980;98:1971-74.
- Labriola LT, Brant AM, Eller AW. Chronic retinal detachment with secondary retinal macrocyst and peripheral neovascularization. Semin Ophthlamol 2009;24:2-4.
- Verdaguer P, Nadal J. Intraretinal cyst secondary to longstanding retinal detachment. Eur J Ophthalmol 2012;22:506-8.
- Mendis KR, Hewick SA. Internal drainage of a retinal macrocyst with an Nd:YAG laser to aid primary retinal reattachment. Arch Ophthalmol 2009;127:791-2.