March, 2023
Presented by Georgia Kamboj, MD, PhD


Presented by Georgia Kamboj, MD, PhD

A 63-year-old woman presents with new floaters in the right eye.
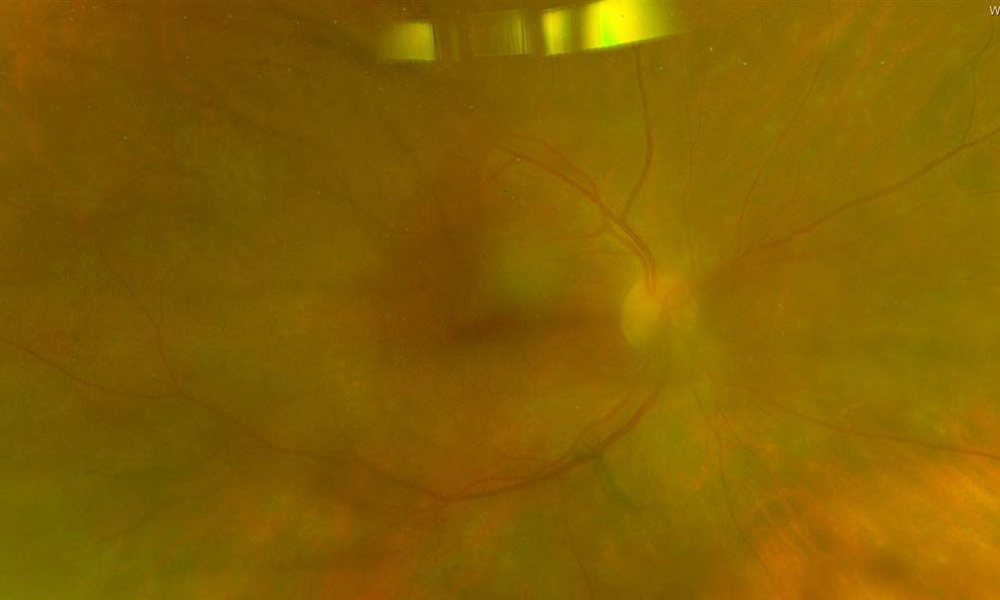
Figure 1A: Wide-field color photo of the right eye. Note the hazy media. Subtle creamy infiltration of the retina is present.

Figure 1B: Wide-field color photo of the left eye is unremarkable.
The patient presented with increasing floaters and mildly blurred vision in the right eye over a 10 day period. She denied flashes, metamorphopsia, and photophobia. On examination, the patient’s best corrected Snellen visual acuity measured 20/32 in the right eye (OD) and 20/20 in the left eye (OS). Intraocular pressure was normal in both eyes. Anterior segment exam of the right and left eyes revealed nuclear sclerotic cataracts. Moderate anterior vitreous cell was present in the right eye. Posterior segment exam of the right eye was significant for mild haze and subtle creamy subretinal lesions in the macular and midperiphery (Figure 1A). The left fundus was unremarkable (Figure 1B). Fluorescein angiography (FA) of the right eye (Figure 2A) showed diffuse patchy hyperfluorescence without leakage from the retinal vessels or optic disc. The FA of the left eye was normal (Figure 2B). Hyperfluorescent spots were seen on fundus autofluorescence of the right eye (Figure 3A), but the left eye was unremarkable (Figure 3B). Optical coherence tomography (OCT) of the right eye showed in the macula showed a normal study but with overlying vitreous cells (Figure 4A). The left macula was unremarkable (Figure 4B). Temporal to the right macula, lumpy-bumpy sub-RPE deposits and intraretinal hyperreflectivity was noted (Figure 4C).
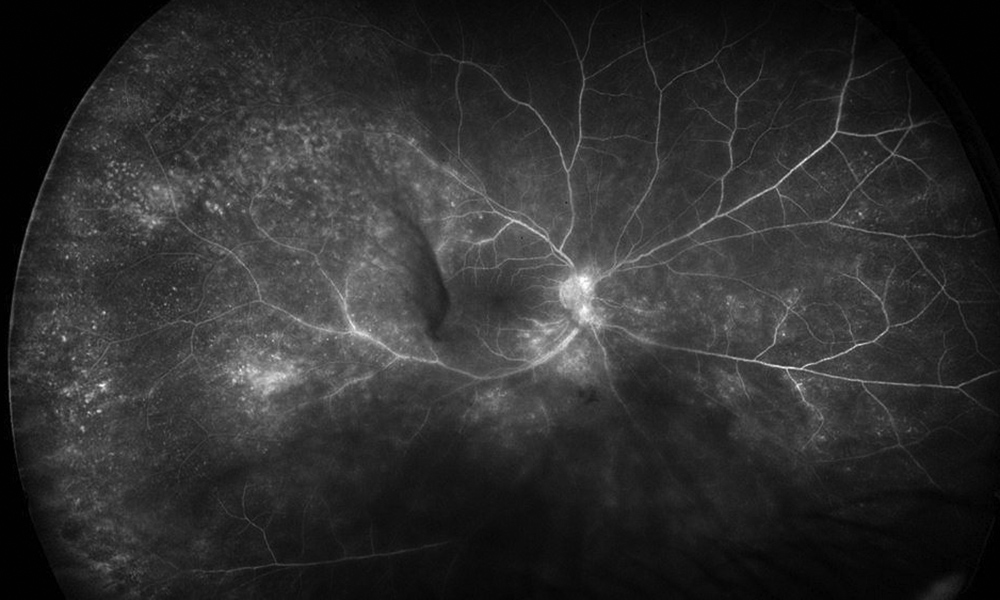
Figure 2A: Wide-field fluorescein angiogram of the right eye. Note the areas of mottled hyperfluorescence and some areas of vascular leakage.
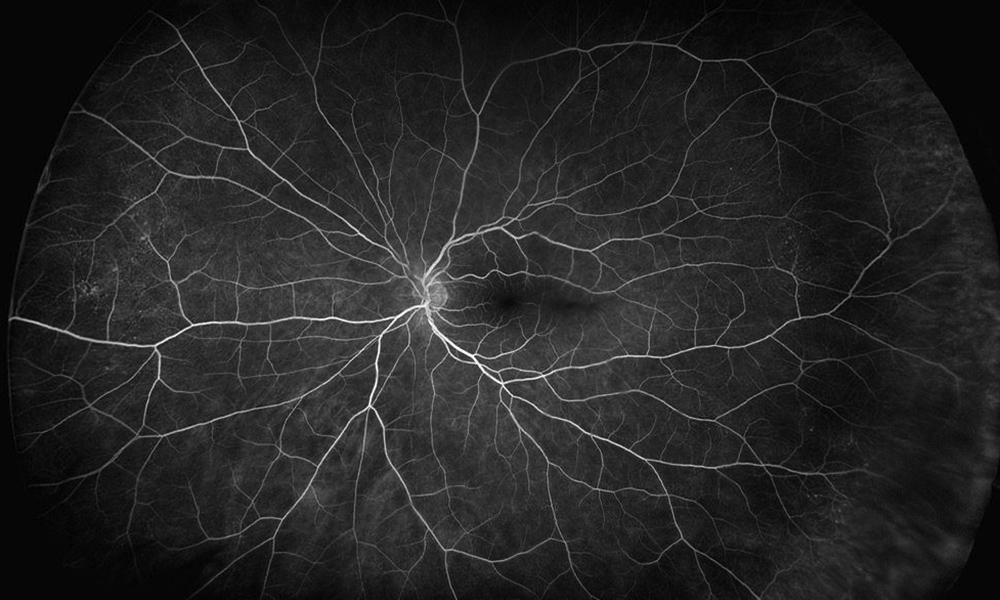
Figure 2B: Wide-field fluorescein angiogram of the left eye is unremarkable.
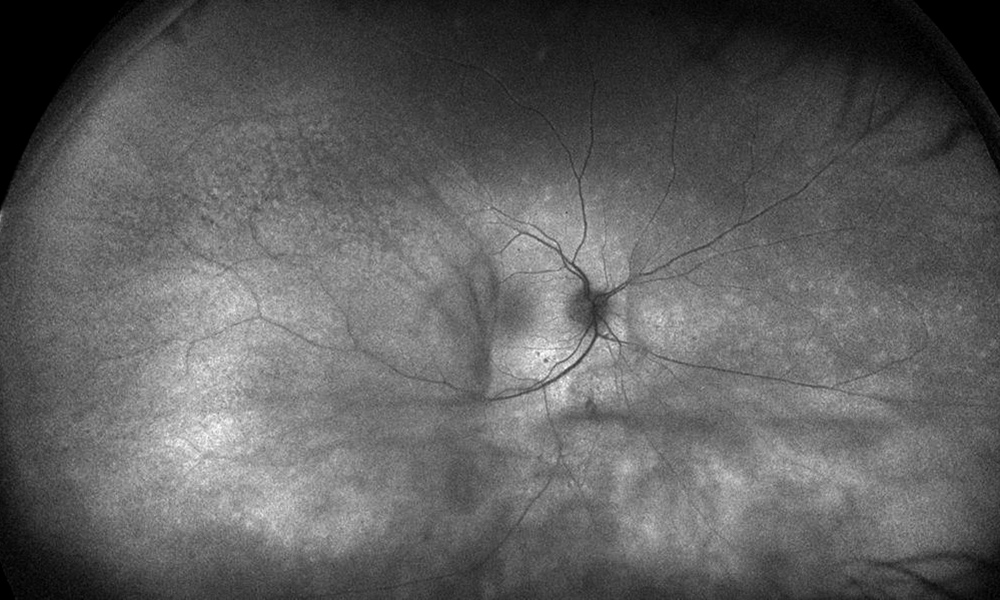
Figure 3A: Wide-field fundus autofluorescence of the right eye. Irregular areas of irregular hyperautofluorescence are present.
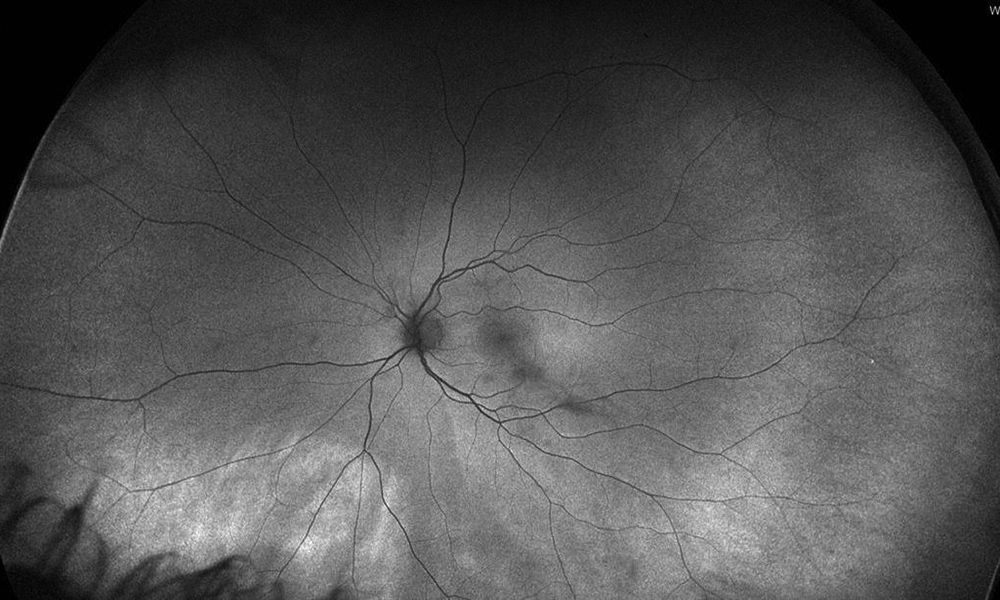
Figure 3B: Wide-field fundus autofluorescence of the left eye is unremarkable.
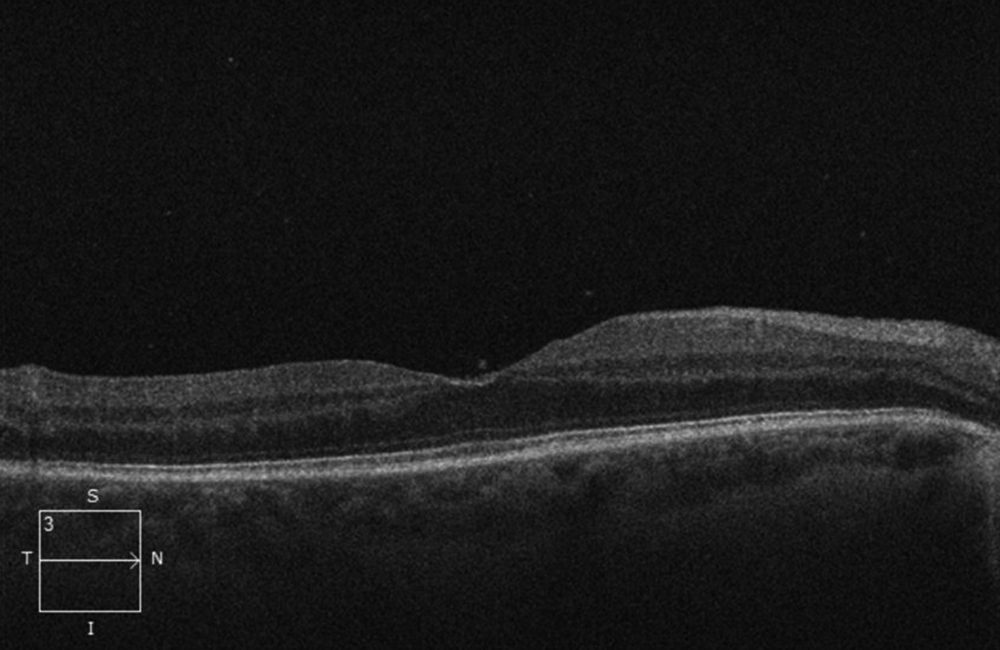
Figure 4A: SD-OCT scan of the right macula. The retina is normal, but note vitreous cells.
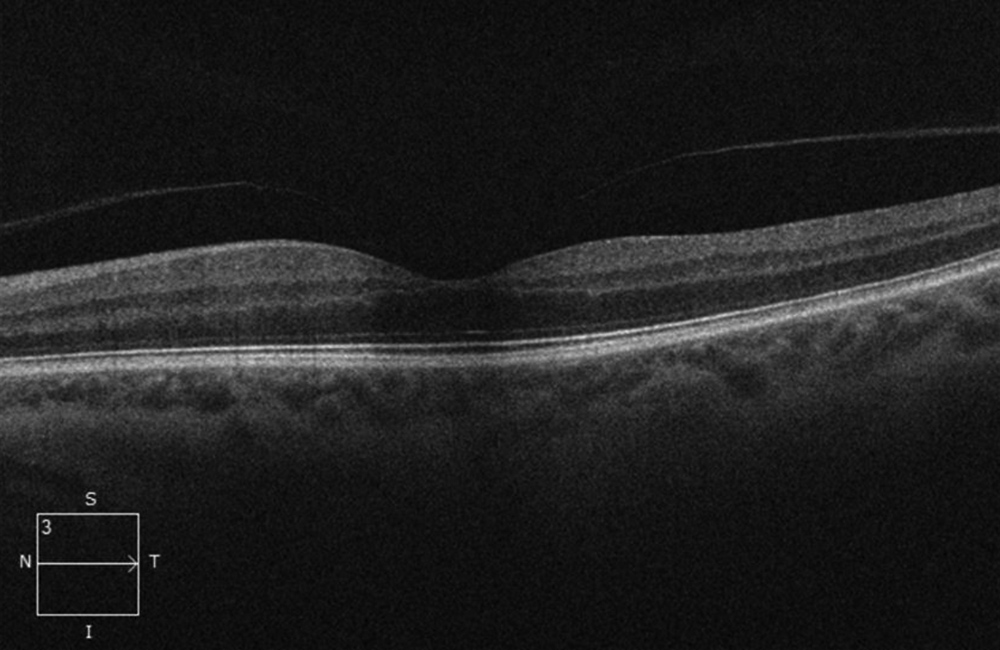
Figure 4B: SD-OCT of the left macula is unremarkable.
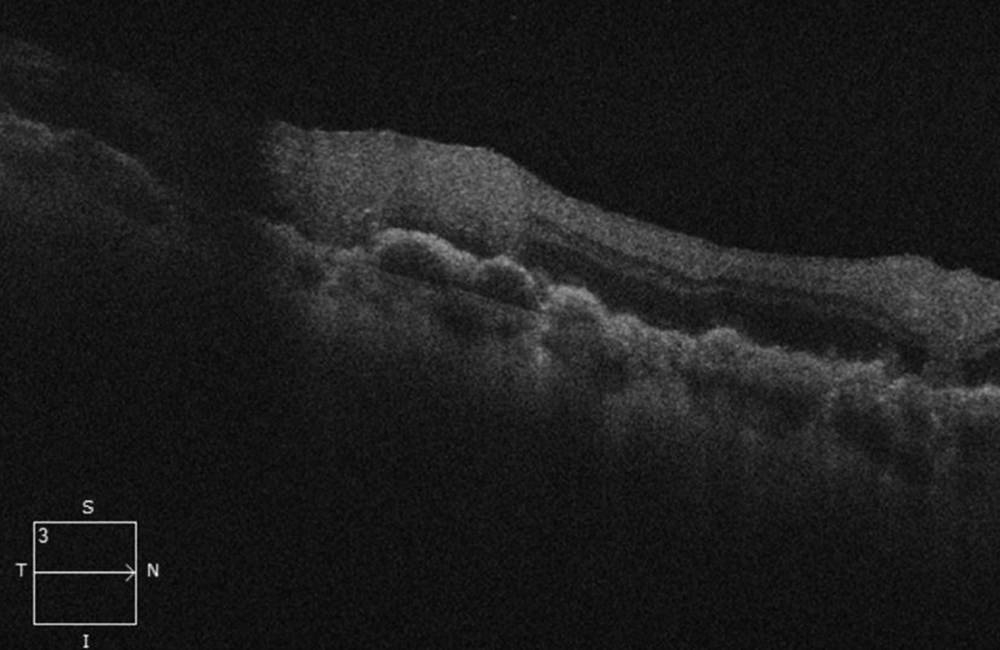
Figure 4C: SD-OCT of the right eye inferotemporal to the macula. Note the lumpy-bumpy RPE elevation and overlying intraretinal infiltration/hyperreflectivity.
Additional History
Her past ocular history was unremarkable. Ten months earlier, the patient was diagnosed with diffuse large B cell lymphoma (DLBCL) confined to the retroperitoneum, and had completed treatment with R-EPOCH. At the time of diagnosis of DLBCL, she was found to have MRI findings concerning for leptomeningeal involvement but she had no focal symptoms and CSF examination did not show evidence of NHL. She was prophylactically treated with intrathecal methotrexate. Following completion of treatment and three months prior to presentation she had a negative PET/CT scan and was currently considered to be in remission.
Differential Diagnosis
Diagnosis and Patient Course
The clinical suspicion for vitreoretinal lymphoma was high given the patient’s recent diagnosis and treatment of DLBCL. The appearance of large anterior vitreous cells, lumpy-bumpy appearance on OCT and fluorescein angiography findings are also consistent with this diagnosis. Repeat staging was performed by the patient’s primary oncologist and no other organ involvement was identified. In a patient with unilateral vitreoretinal lymphoma with no evidence of systemic activity, treatment options include intravitreal methotrexate, external beam radiotherapy and high dose systemic chemotherapy. The patient has opted to proceed with several cycles of systemic chemotherapy including intravenous methotrexate.
Discussion
Intraocular lymphomas can be categorized by the region of involvement (vitreoretinal lymphoma (VRL), choroidal lymphoma, and iridial lymphoma). VRL may be either primary or secondary. Primary VRL is considered a subset of CNS lymphoma where as secondary VRL is associated with systemic lymphoma elsewhere in the body.1 Approximately 20% of patients diagnosed with primary CNS lymphoma go on to develop vitreoretinal involvement.2 Of those with primary vitreoretinal lymphoma, up to 90% will subsequently develop CNS involvement.3 Secondary ocular involvement of systemic lymphoma most commonly involves the choroid but can present with vitreoretinal involvement alone in 5% of cases.1
Cytological examination of vitreous or chorioretinal biopsies is the gold standard for diagnosis. Positive biopsies show large atypical lymphoid cells with pleomorphic nuclei, scant basophilic cytoplasm and prominent nucleoli.4 Unfortunately only 50 % of VRL cases yield a positive diagnosis on cytology from vitreous or chorioretinal biopsy.4 PCR for mutation in the MYD88 gene can also be performed on biopsy specimens and aid in a positive diagnosis.5
Treatment of VRL depends on the extent of disease. Management options have been reviewed by Pulido et al. (2018), and the following summarizes their recommendations.6 When disease is unilateral and there is no evidence of CNS or systemic involvement, local therapy can be considered. Local intravitreal therapies include intravitreal methotrexate and/or intravitreal rituximab. Monitoring of treatment efficacy and recurrence while on intravitreal treatment can be performed via aqueous sampling and quantitative testing of interleukin-10. Local treatment with external beam radiotherapy is another alternative for unilateral disease, however the risk of radiation retinopathy needs to be considered. In patients with bilateral VRL, or associated CNS or systemic involvement, systemic treatment with methotrexate or rituximab is often used in conjunction with intravitreal therapy. When there is recurrence of disease, stem cell transplant can also be considered.