May, 2023
Presented by Georgia Kamboj, MD, PhD


Presented by Georgia Kamboj, MD, PhD

A 38-year-old white woman was referred with a hypopigmented lesion in the right eye.
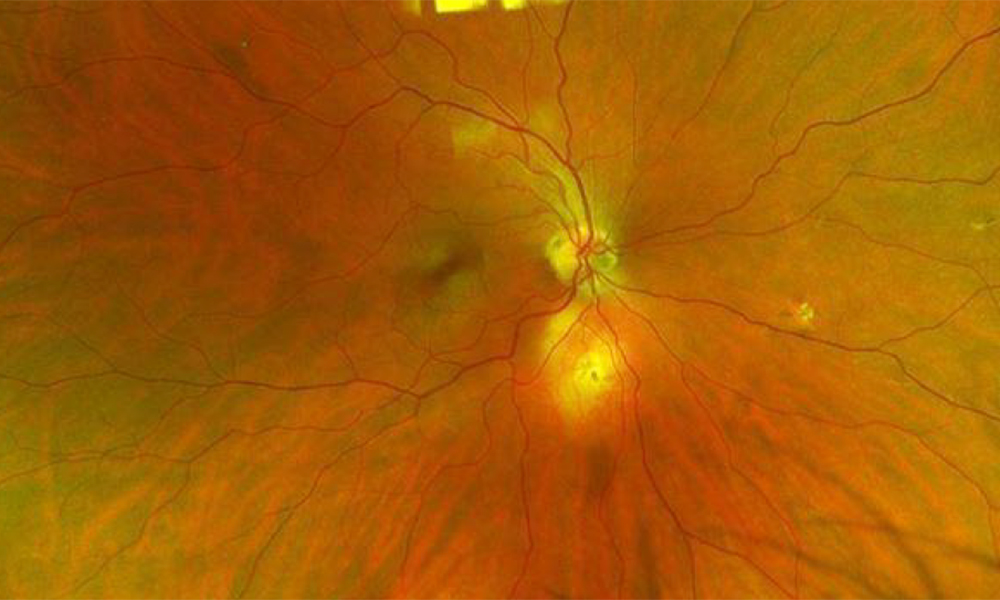
Figure 1A: Wide-field color photo of the right eye. Note the amelanotic lesion just inferior to the nerve

Figure 1B: Wide-field color photo of the left eye is unremarkable.
The patient was referred by her local eye doctor after a routine examination. She denied changes to her vision, flashes/floaters, metamorphopsia, and photophobia. Her past ocular history and past medical history were negative. Review of systems was negative. She was born and raised in Missouri and moved to California at age 21.
The patient’s best corrected Snellen visual acuity measured 20/20 in each eye. Intraocular pressure was normal in both eyes. Anterior segment exam was unremarkable, without evidence of inflammation. There was no vitritis. Posterior segment exam of the right eye was remarkable for a small nasal chorioretinal scar as well as an elevated, yellowish lesion inferior to the optic nerve, approximately 2.5mm x 3.5mm in size, with a central focal area of chorioretinal scaring and a surrounding orange halo (Figure 1A). The vasculature appeared normal and there was no subretinal fluid. The left fundus showed no abnormalities (Figure 1B). Macular optical coherence tomography (OCT) of both eyes was unremarkable (Figure 2A-B). OCT taken through the inferior yellow lesions in the right eye showed a dome shaped scleral lesion with severe choroidal thinning and normal overlying retinal layers (Figure 2). Hyperautofluorescence was noted on fundus autofluorescence (Figure 3A). Fluorescein angiography demonstrated late staining (Figure 3B). There was hypocyanescence on indocyanine green angiography (Figure 3C).
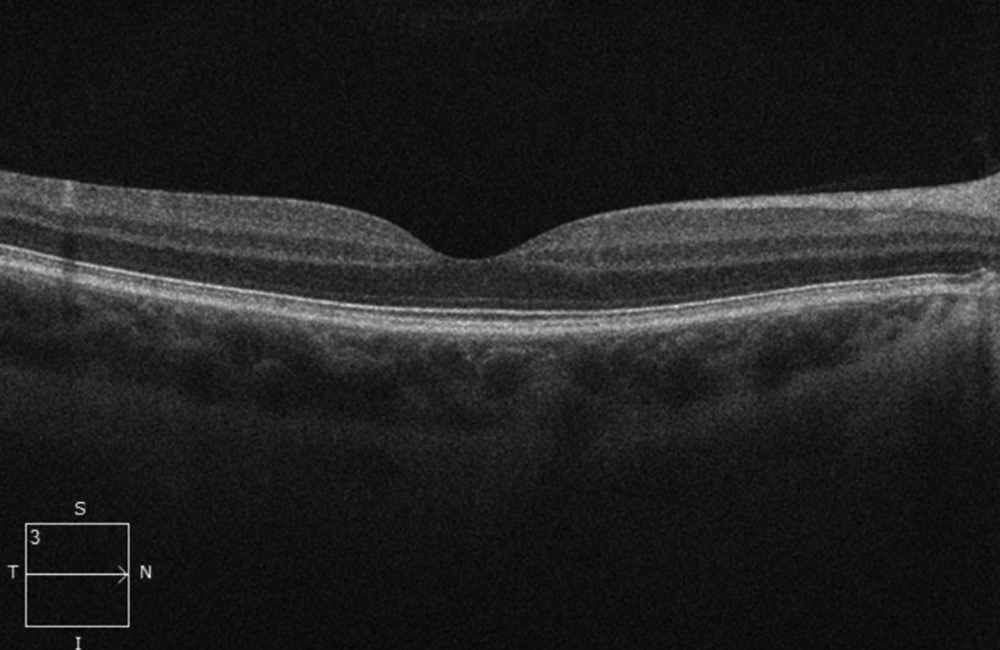
Figure 2A: SD-OCT scan of the right macula. The scan is unremarkable.
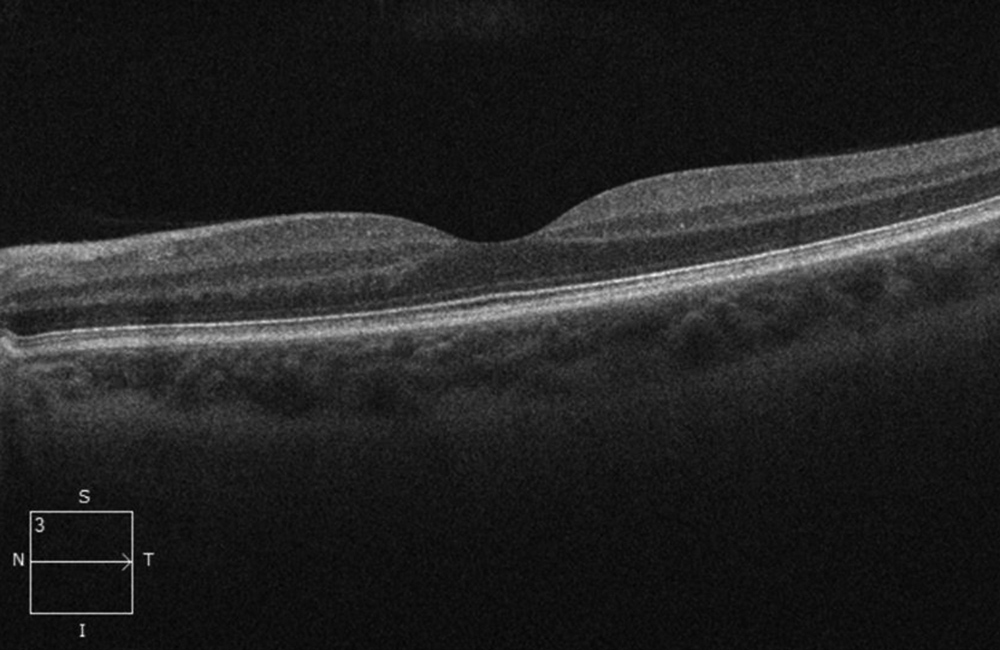
Figure 2B: SD-OCT of the left macula is unremarkable.
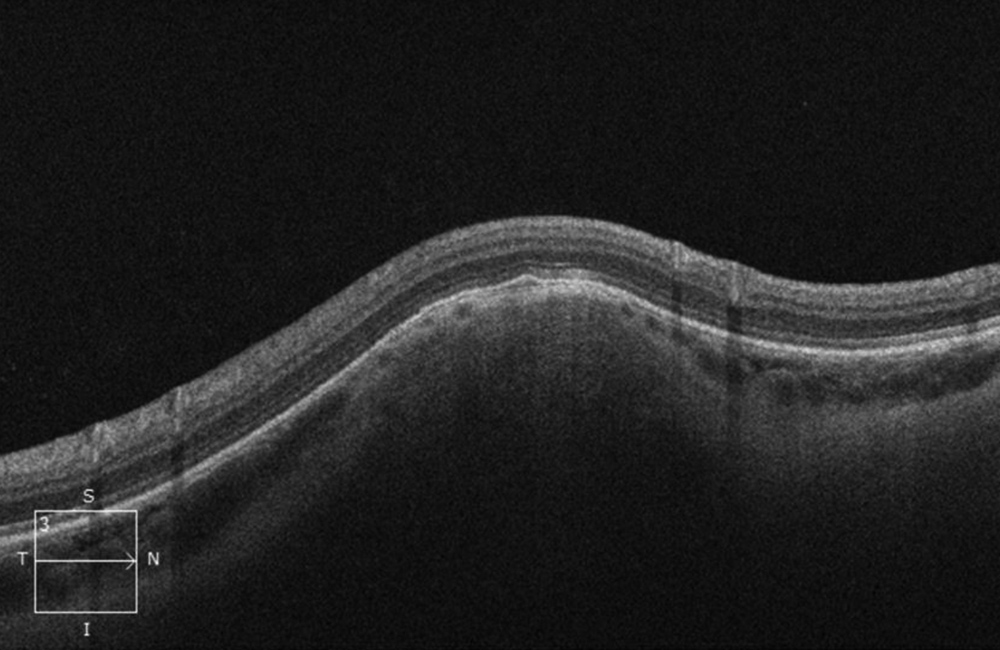
Figure 2C: OCT-SD scan through the yellowish lesion inferior to the nerve. The lesion is in the sclera and is dome shaped with choroidal thinning and normal overlying retinal layers .
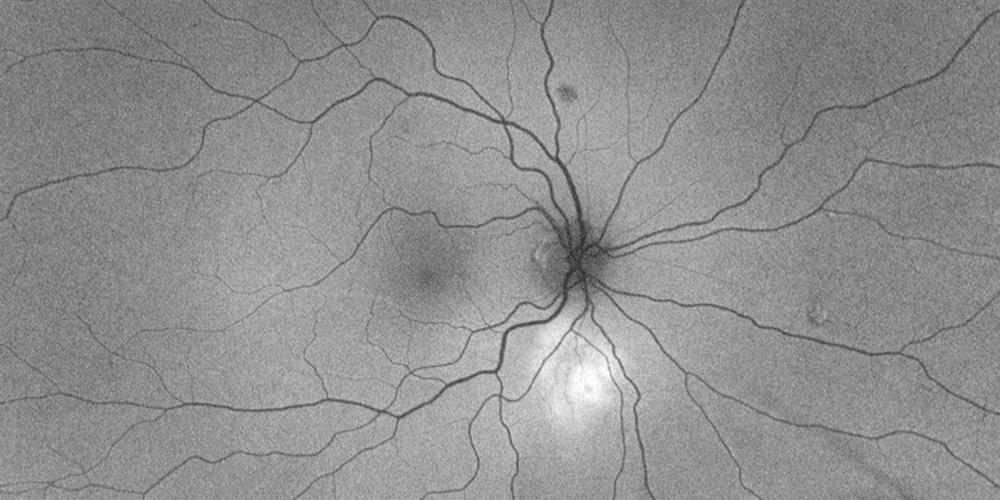
Figure 3: Wide-field autofluorescence right eye. Note the increased autofluorescence in the area of the lesion
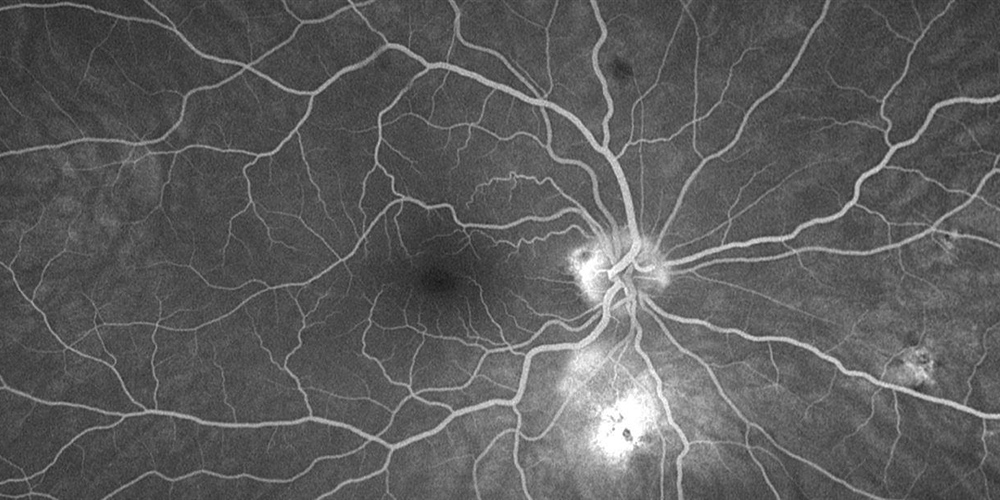
Figure 4: Wide-field fluorescein angiogram of the right eye. Note the increased fluorescence, but no leakge was present on later studies, or evidence of vasculitis or inflammation.
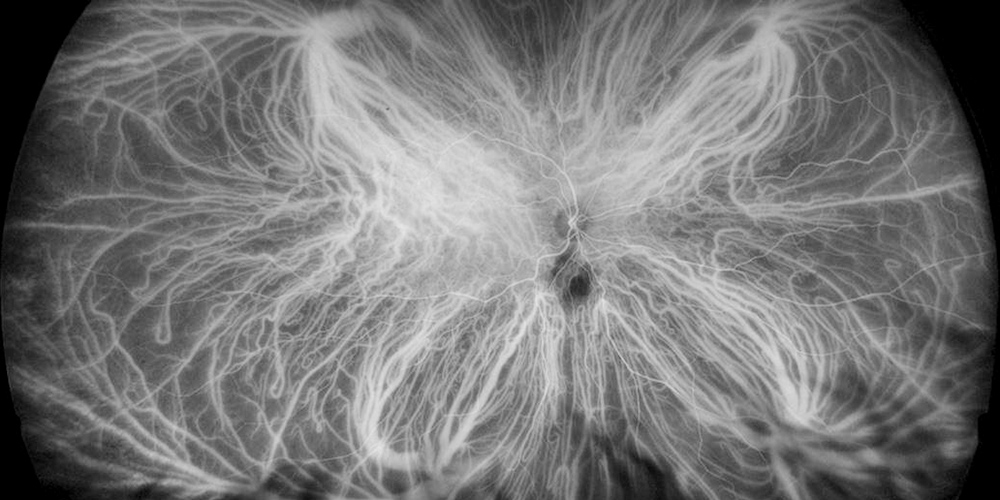
Figure 5: Wide-field indocyanine angiogram of the right eye. Note the decreased cyanescence in the area of the lesion.
Differential Diagnosis
Diagnosis and Patient Course
A diagnosis of focal scleral nodule (FSN) was made based on the dome-shaped scleral lesion on OCT, which is characteristic of this condition. Observation of the lesions without further workup was recommended.
Discussion
Focal scleral nodules (FSN) were first named unifocal helioid choroiditis1 and later re-named as solitary idiopathic choroiditis2. They are thought to be congenital in origin and are most commonly found in White Females.2 The characteristic appearance is a unilateral, yellow/white mass near the optic nerve, with an orange halo. Legions are asymptomatic and are often found incidentally.
The differential diagnosis includes inflammatory conditions (choroidal granuloma), malignant lesions (choroidal metastasis) and other benign lesions of the sclera (sclerochoroidal calcification) and choroid (choroidal osteoma). Multimodal imaging including the use of OCT and b-scan are key in differentiating between these diagnoses. Enhanced depth imaging (EDI) OCT demonstrates that FSN lesions arise from the scleral and/or outer choroid with thinning of the overlying choroidal vasculature.3 They can appear dome shaped or nodular on OCT and are rarely associated with subretinal fluid. The lesions are acoustically dense on ultrasound (unlike sclerochoroidal calcifications and choroidal osteomas which are hyper-echoic on ultrasound).4 Hyperautofluoresence is typically seen on autofluorescence with late staining on fluorescein angiography and hypocyanescence on indocyanine green angiography.4 Sclerochoroidal calcifications are generally seen more peripherally compared with FSN, have a more irregular surface and are associated with disease causing disfunction in calcium-phosphorous metabolism.4
The majority of FSN lesions remain stable on long-term follow-up and require no treatment. Very occasionally, lesions can grow or regress over time.4 Regressed lesions can lead to focal choroidal excavations.4