West Coast Retina
Case of the Month
April, 2010
Presented by Jon Wender, MD
A 32 year-old man was found to have an asymptomatic scar on routine exam.
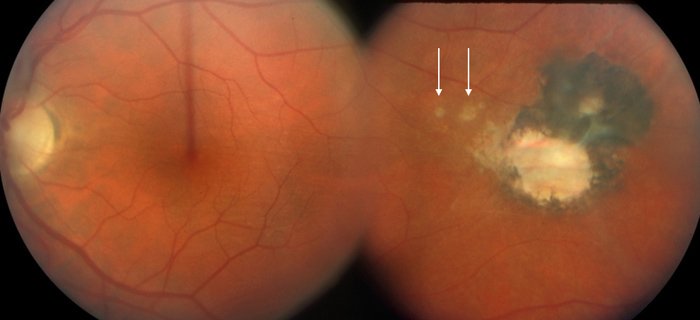
Figure 1: Note the pigmented chorioretinal scar temporally. A couple of smaller scars are seen on the foveal side of the scar (arrows)
Case History
An asymptomatic 32-year-old Caucasian man was noted on routine exam to have a chorioretinal scar in the temporal mid-periphery of the left fundus (Fig. 1). His past medical, surgical, family, and social history were non-contributory. His visual acuity was 20/13 in the right eye and 20/16 in the left eye. Eight years later, during an annual exam, the patient was still asymptomatic but the chorioretinal scar in his left eye was closer to the macula (Fig 2).
Two and a half years later, the patient began to notice blurred vision and floaters in his left eye. His left visual acuity decreased to 20/50. Anterior segment examination was within normal limits in each eye. Fundus examination of the left eye revealed moderate vitritis as well as an area of active retinitis in close proximity to the fovea and bordering on the chorioretinal scar (Fig. 3A). Fluorescein angiography revealed late leakage in the region of active retinitis and late staining of the chorioretinal scar (Figs. 3B and C). Empiric therapy with oral trimethoprim / sulfamethoxazole (Bactrim), 400/80 mg (double strength, DS), twice daily in addition to a 2-week taper of oral prednisone, starting at 80 mg per day, was initiated. Serum levels of anti-Toxoplasma gondii IgG were found to be significantly elevated to 244 IU/mL (normal < 7.5 IU/mL). Two weeks later, the visual acuity in his left eye improved to 20/25 and the area of active retinitis had largely resolved. The patient completed a one-month course of Bactrim DS, twice daily.
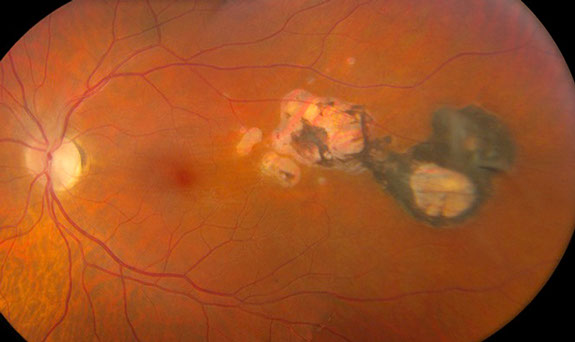
Figure 2: Eight years after presentation, the chorioretinal scars have enlarged and extended closer to the fovea.

Figure 3A:
Note the active chorioretinitis at the temporal edge of the fovea (arrows). Also, the entire area of old scarring has enlarged since photos 2 1/2 years earlier (Fig 2).
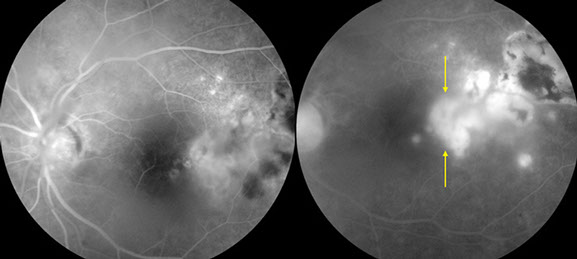
Figures 3B and C:
Note the area of intense hyperfluorescence temporal to the fovea due to the active inflammation (arrows).
Case History (Continued)
Four and a half months later, the patient again noted an increase in the number of floaters in his left eye. Visual acuity at that time was 20/25 in the left eye. Posterior segment examination of the left eye revealed vitritis and active retinitis within one disc diameter of the foveal center. (Fig. 4A) Fluorescein angiography revealed early hypofluorescence with progressive leakage in the region of active retinitis and late staining of the chorioretinal scar (Figs. 4B & C). “Quadruple therapy”, including pyrimethamine, 100 mg, every 12 hours for one day, followed by 25 mg daily; folinic acid, 10 mg, every other day; sulfadiazine, 2 gm for one dose followed by 1 gm, four times per day; as well as prednisone, 60 mg daily, was initiated. An intravitreal injection of 1.0 mg in 0.1 mL of clindamycin was also administered. One week later, the vitritis and retinitis began to resolve. Pyrimethamine, folinic acid, and sulfadiazine were then discontinued; prednisone was tapered; and Bactrim DS, PO, twice daily, was reinstituted. Over the following month, the visual acuity in the left eye remained stable at 20/25, the active retinitis resolved and long-term maintenance therapy with Bactrim DS, one pill every third day, was initiated.

Figure 4A:
Note the area of active chorioretinitis inferiorly (arrow).
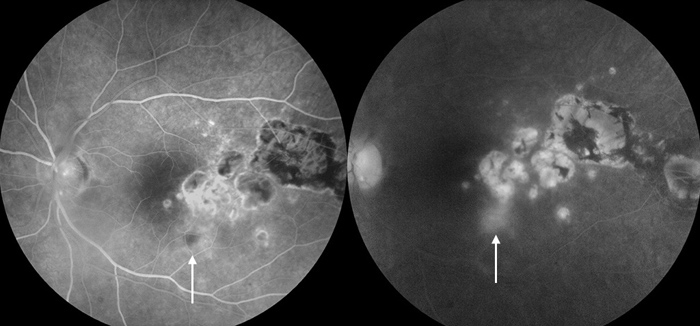
Figures 4B & C:
The fluorescein angiogram shows the old inactive areas of inflammation and scarring and the new active lesion (arrows)
Discussion
Toxoplasmosis is one of the most common causes of posterior uveitis in immunocompetent individuals.1 The typical clinical manifestations include significant vitritis and a focal area of retinochoroiditis with or without an adjacent retinochoroidal scar. Because the infection is often self-limited, toxoplasmic retinochoroiditis may, in some cases, be observed without therapy. In many cases, however, treatment may be indicated in order to address a decrease in visual acuity, a moderate to severe level of vitritis, an area of retinochoroiditis that is larger than one disc diameter in size, or a lesion that is significantly close to the fovea or optic nerve.2,3
Classic quadruple therapy for toxoplasmosis includes a combination of pyrimethamine, folinic acid, sulfadiazine, and prednisone. Because this treatment modality is associated with significant side effects and difficulty in maintaining patient compliance, however, many uveitis specialists employ alternative therapeutic regimens.2 These strategies most commonly involve therapy with a single antibiotic agent such as pyramethamine, sulfadiazine, Bactrim, or clindamycin with or without the addition of systemic corticosteroids.2 A prospective randomized trial comparing Bactrim with classic multi-agent therapy demonstrated that outcomes, in terms of improvement in visual acuity and reduction in lesion size, were similar between the two groups.4 For these reasons, the patient described herein was treated briefly with quadruple therapy but primarily with Bactrim and a prednisone taper.
In some cases, however, systemic therapy is either ineffective, prohibitively expensive, or associated with unacceptable adverse effects.5 In such patients, an intravitreal injection of clindamycin may facilitate prompt resolution of toxoplasmic retinochoroiditis.6,7 In the present case, intravitreal clindamycin was administered because of steady progression of the lesion into the fovea. In conjunction with systemic antibiotic and corticosteroid therapy, intravitreal clindamycin yielded a rapid improvement of the vitritis and retinitis along with preservation of favorable visual acuity.
Long-term intermittent therapy with Bactrim has been demonstrated to decrease the rate of recurrences of toxoplasmic retinochoroiditis.8 Given the proximity of the lesion to the foveal center as well as the frequency of relapses of inflammation in the present case, maintenance therapy with Bactrim was employed.
Take Home Points
- Toxoplasmosis is a very common cause of posterior uveitis
- Treatment may be indicated if there is a significant decline in vision, moderate to severe vitritis, or retinochoroiditis that is close to the fovea or optic nerve
- Classic multi-agent therapy may not be warranted; alternatively, mono-therapy with an agent such as Bactrim, pyrimethamine or sulfadiazine may be employed
- Intravitreal clindamycin may yield rapid improvement in toxoplasmic retinochoroiditis when systemic therapy is ineffective or poorly tolerated
- Intermittent, maintenance therapy with Bactrim may be effective in preventing recurrences of toxoplasmic retinochoroiditis in patients with frequent bouts of inflammation or lesions that threaten the fovea or optic nerve
Want to Subscribe to Case of the Month?
References
- Bonfioli AA, Orefice F. Toxoplasmosis. Semin Ophthalmol 2005;20(3):129-41.
- Holland GN, Lewis KG. An update on current practices in the management of ocular toxoplasmosis. Am J Ophthalmol 2002;134(1):102-14.
- Lum F, Jones JL, Holland GN, Liesegang TJ. Survey of ophthalmologists about ocular toxoplasmosis. Am J Ophthalmol 2005;140(4):724-6.
- Soheilian M, Sadoughi MM, Ghajarnia M, et al. Prospective randomized trial of trimethoprim/sulfamethoxazole versus pyrimethamine and sulfadiazine in the treatment of ocular toxoplasmosis. Ophthalmology 2005;112(11):1876-82.
- Bosch-Driessen LH, Verbraak FD, Suttorp-Schulten MS, et al. A prospective, randomized trial of pyrimethamine and azithromycin vs pyrimethamine and sulfadiazine for the treatment of ocular toxoplasmosis. Am J Ophthalmol 2002;134(1):34-40.
- Kishore K, Conway MD, Peyman GA. Intravitreal clindamycin and dexamethasone for toxoplasmic retinochoroiditis. Ophthalmic Surg Lasers 2001;32(3):183-92.
- Sobrin L, Kump LI, Foster CS. Intravitreal clindamycin for toxoplasmic retinochoroiditis. Retina 2007;27(7):952-7.
- Silveira C, Belfort R, Jr., Muccioli C, et al. The effect of long-term intermittent trimethoprim/sulfamethoxazole treatment on recurrences of toxoplasmic retinochoroiditis. Am J Ophthalmol 2002;134(1):41-6.