West Coast Retina
Case of the Month
April, 2012
A 50-year-old man with decreased vision in his right eye.
Presented by Sandeep Randhawa, MD

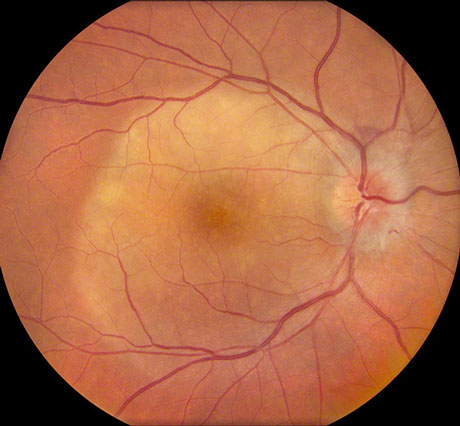
A
B
Figures 1A and B: Color photographs of the right and left eye. In the right eye, note the yellowish placoid lesion in the macula and the optic disc edema. There is a small subretinal hemorrhage superior to the disc. In the left eye, there is a small yellowish subretinal lesion superotemporal to the macula.
Case History
A 50-year-old man presented with decreased vision in his right eye for two weeks. His past medical history, family history and review of symptoms was unremarkable.
On examination his best corrected visual acuity was hand motion in the right eye and 20/20 in the left. He had a positive relative afferent pupillary defect in the right eye. His anterior segment exam and intraocular pressure was normal in both eyes.
Dilated fundus exam of the right eye showed optic disc edema and a yellow circular subretinal lesion in the macula that was lighter centrally and inferiorly (Figure 1A). A small subretinal hemorrhage superior to the disc was present as well. The left eye has a small yellow subretinal lesion superotemporal to the macula (Figure 1B).
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis includes acute posterior multifocal placoid pigment epitheliopathy, persistent placoid maculopathy, acute syphilitic posterior placoid chorioretinitis, viral retinitis, and lymphoma.
Additional Investigations
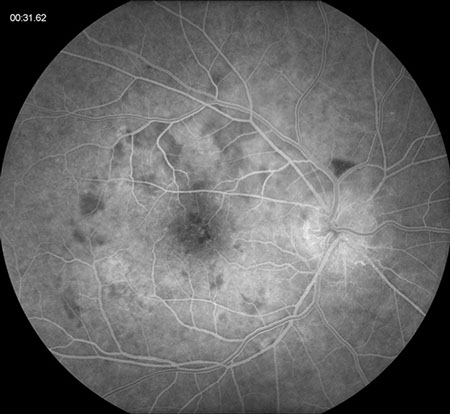
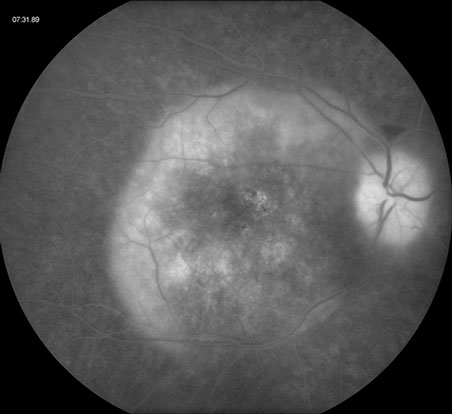
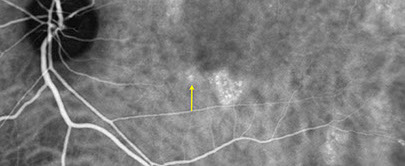
Fluorescein angiography (FA) revealed early patchy hypofluorescence with late staining along the outer rim of the lesion in the right eye and also disc leakage (Figure 2A and B). The left eye showed late staining of the superotemporal lesion and small points of hyperfluorescence in the inferior parafoveal area and inferotemporal to the macula on fluorescein angiography (Figure 3). Indocyanine green (ICG) angiography revealed hypofluorescence of the large posterior placoid lesion in the right eye and the small superotemporal lesion in the left eye (Figure 4A and B). In addition, multiple hyperfluorescent patches were seen in the posterior pole and along the superotemporal arcade in the left eye (most of these spots corresponded to the point areas of hyperfluorescence on FA but were much more prominent on ICG (Figure 4B). Autofluorescence imaging showed hyperautofluorescence of the placoid lesion in the right eye and small areas of hypoautofluorescence corresponding to the hyperfluorescent patches on ICG angiography in the left eye (Figure 5A and B).
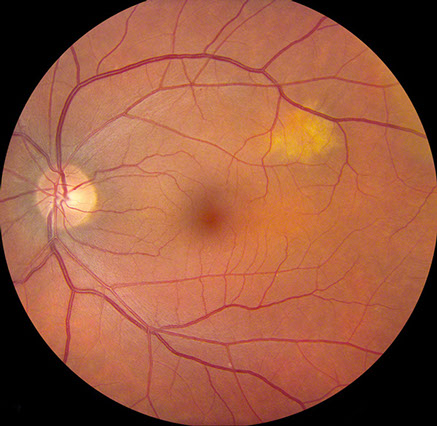
A
B
Figures 2A and B: Fluorescein angiography of the right eye. Note the early patchy hypofluorescence around the macula and late staining along the outer rim of the placoid lesion. Disc leakage is present.
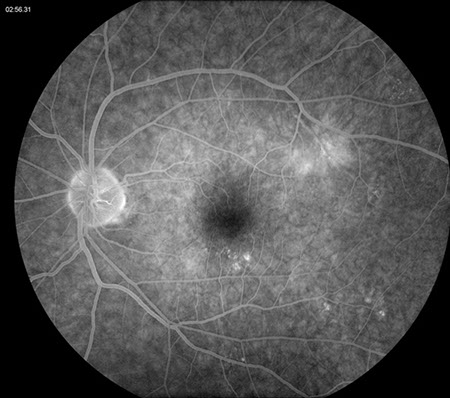
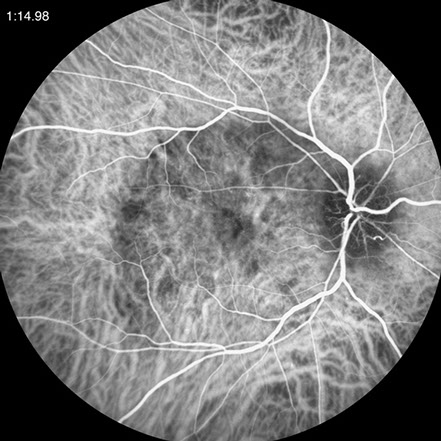
Figure 3: Late phase fluorescein angiogram of the left eye. Note the staining of the superotemporal lesion as well as some other areas of staining inferiorly. Also note, a semi-circular area of increased hyperfluorescence on the nasal side of the macula.
A
B
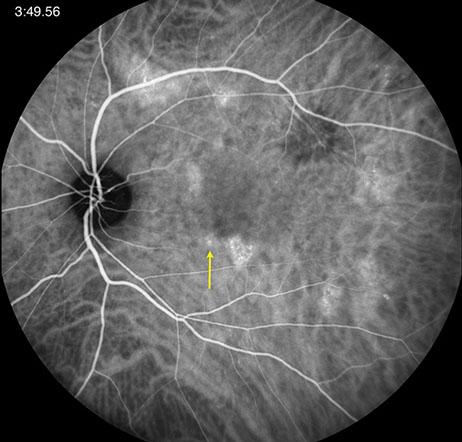
Figures 4A and B: ICG angiography of the right eye and left eye. In the right eye, there is hypofluorescence of the large posterior placoid lesion. Note in the left eye the hypofluorescence of the superotemporal lesion and the multiple hyperfluorescent patches in the posterior pole and along the superotemporal arcade. The yellow arrow corresponds to the lesion imaged on the SD-OCT scan below (FIg. 6D)

A
B
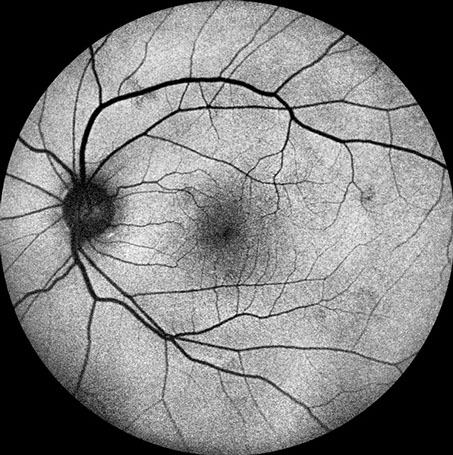
Figures 5A and B: Fundus autofluorescence photos of the right and left eye. Note the increased autofluorescence corresponding to the placoid lesion in the right eye. In the left eye, there are small areas of reduced autofluorescence corresponding to the multiple hyperfluorescent patches on the ICG angiograms (Fig 4B).
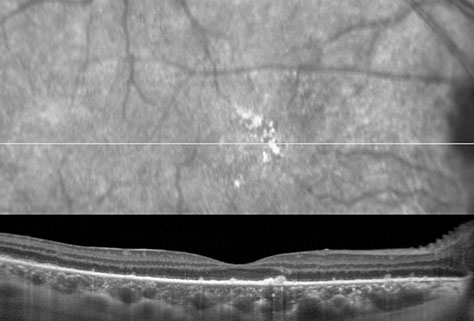
A
B
Figures 6A and B: Spectral domain optical coherence tomography of the right eye. On the left is a scan through the fovea showing choroidal infiltration, loss of the photoreceptor IS/OS junction, and hyperreflective clumps above an abnormal mottled RPE. On the right side, the scan is through the superior macula. Widespread pigment migration into the retina, diffuse IS/OS junction loss, and a focal discontinuity of the external limiting membrane is present.
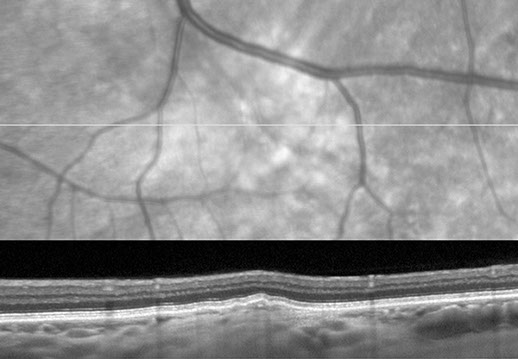
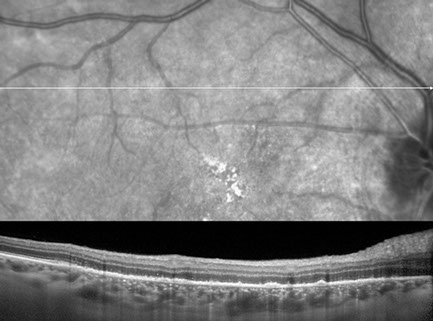
C
D
E
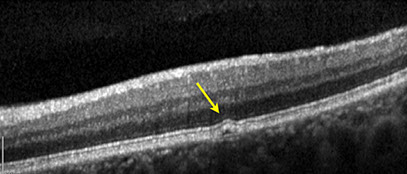
Figures 6C-E: Spectral domain optical coherence tomography of the left eye. Fig 6C shows the scan through the choroidal lesion superotemporal to the macula. Note the choroidal infiltration and elevation of the RPE. Fig 6E is the scan through the hyperfluorescent lesions on the ICG (Fig 6D, yellow arrow) in the left eye revealing small detachment of the RPE.
Additional Investigations
Spectral domain optical coherence tomography (SD-OCT) through the fovea in the right eye showed choroidal thickening and infiltration with extensive loss of the photoreceptor inner segment-outer segment (IS/OS) junction (Figure 6A and B). Also, hyperreflective clumps were noted above an abnormal retinal pigment epithelium (RPE) which was mottled and allowed increased choroidal reflectivity. Additionally, a scan through the superior macula revealed widespread pigmentary migration into the retina, diffuse IS/OS junction loss, and a focal discontinuity of the external limiting membrane (Figure 6B).
SD-OCT of the left eye in the region of the superotemporal choroidal lesion showed apparent choroidal infiltration with elevation of the RPE (Figure 6C). Fig 6E, a scan through the hyperfluorescent lesions on ICG in the left eye (yellow arrow, Fig 4B and Fig 6D) revealed tiny RPE detachments.
The imaging clearly revealed that the patient had a bilateral chorioretinitis with concomitant optic nerve involvement in the right eye.
Clinical Course
The clinical presentation and findings on the imaging studies suggested that the most likely diagnosis was acute syphilitic posterior placoid chorioretinitis. This was confirmed with a positive rapid plasma reagin (RPR, titer 1:128) and treponema pallidum antibody (TP-PA). In consultation with his primary care physician, the patient was initiated on procaine penicillin-G, in a dosage of 2.4 million units administered intramuscularly once daily, plus probenecid in a dosage of 500 mg orally four times daily, for two weeks.
Discussion
There has been an increase in the incidence of syphilis in the United States in recent years and it remains an important cause of uveitis.1
While the majority of findings in ocular syphilis are fairly nonspecific, the finding of acute posterior placoid chorioretinitis in syphilis described by Gass is highly suggestive of the diagnosis.2 Gass et al postulated that, in secondary syphilis, the widely disseminated spirochaetes may also be present in the inflammation around the RPE in the placoid lesions of acute syphilitic posterior placoid chorioretinitis.2 Another explanation was that the clinical appearance was due to deposition of soluble immune complexes.3
The findings show a large, placoid, yellowish lesion with central fading at the level of the RPE in the macular and juxtapapillary areas, which shows a fluorescein angiographic pattern of early hypofluorescence and late staining. The placoid lesion is hypofluorescent on ICG angiography4 and hyperautofluorescent.5 It can be accompanied by variable amount of vitreous inflammation and may be associated with superficial hemorrhages, retinal vasculitis, disc edema and subretinal fluid.6
The SD-OCT findings through acute syphilitic posterior placoid chorioretinitis have previously been reported7 and our patient had similar findings of choroidal infiltration with loss of the photoreceptor IS/OS junction and external limiting membrane. In addition, hyperreflective clumps above an abnormal mottled RPE were noted in our patient.
There have been two reports8,9 of multiple hyperfluorescent spots seen on the ICG angiography in syphilis as were seen in the left eye of our patient. SD-OCT through these spots has not been previously described. In our case, there was presence of mild RPE detachments corresponding to these spots (which were much more hyperfluorescent on the ICG than on the FA and were hypoautofluorescent).
It is now well-known that acute syphilitic posterior placoid chorioretinitis can occur independently of the immune status of the patient. Even though the exact pathogenesis of this entity still remains unknown, the angiographic and SD-OCT findings in our patient clearly point to a pathogenic process at the level of the choroid-retinal pigment epithelium complex with secondary insult to the photoreceptor IS/OS junction layer.
Take Home Points
- Acute syphilitic posterior placoid chorioretinitis can be the presenting sign of syphilis, and this gives the ophthalmologist an important role in the detection and treatment of this disease.
- Syphilitic chorioretinitis is often a bilateral disease and ICG angiography and spectral domain OCT are helpful in identifying chorioretinitis which may not be apparent on exam
Want to Subscribe to Case of the Month?
References
- Heffelfinger JD, Swint EB, Berman SM, Weinstock HS: Trends in primary and secondary syphilis among men who have sex with men in the United States. Am J Public Health. 2007;97:1076-83.
- Gass JDM, Braunstein RA, Chenoweth RG: Acute syphilitic posterior placoid chorioretinitis. Ophthalmology 1990;97:1288-1297.
- de Souza EC, Jalkh AE, Trempe CL, Cunha S, Schepens CL: Unusual central chorioretinitis as the first manifestation of early secondary syphilis. Am J Ophthalmol 1988;105:271–276.
- Meira-Freitas D, Farah ME, Höfling-Lima AL, Aggio FB: Optical coherence tomography and indocyanine green angiography findings in acute syphilitic posterior placoid choroidopathy: case report Arq Bras Oftalmol. 2009;72(6):832-5.
- Bellmann C, Holz FG, Breitbart A, Völcker HE: Bilaterale akute syphilitische posteriore plakoide chorioretinopathie (ASPPC) Angiographie- und Autofluoreszenz-Merkmale. Ophthalmologe 1999; 96:522-528.
- Aldave AJ, King JA, Cunningham Jnr, ET: 2001. Ocular syphilis. Curr Opin Ophthalmol, 12:433–441.
- Brito P, Penas S, Carneiro A, Palmares J, Falcão Reis, F: Spectral-Domain Optical Coherence Tomography Features of Acute Syphilitic Posterior Placoid Chorioretinitis: The Role of Autoimmune Response in Pathogenesis. Case Rep Ophthalmol 2011;2:39-44.
- Mora P, Borruat F, Guex-Crosier Y: Indocyanine Green Angiography Anomalies In Ocular Syphilis. Retina 2005;25:171–181.
- Joseph A, Rogers S, Browning A, Hall N, Barber C, Lotery A, Foley E, Amoaku WM: Syphilitic acute posterior placoid chorioretinitis in nonimmunocompromised patients. Eye 2007;21:1114–1119.