West Coast Retina
Case of the Month
April, 2014
Presented by Steven Williams, MD
A 39 year-old man with acute vision loss of the right eye


A
B

C
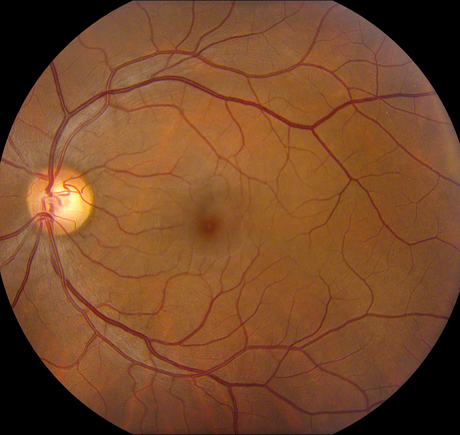
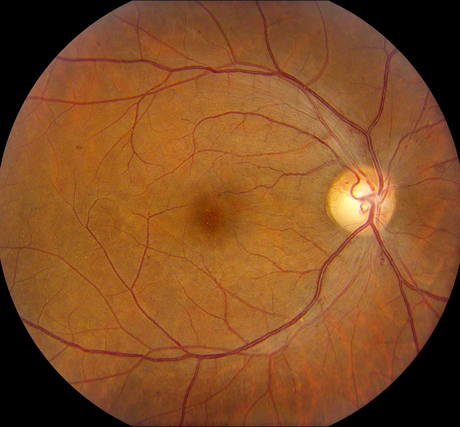
Figures 1A-C: Photos of the right eyes reveals patchy retinal whitening (A and C), with associated hemorrhage, venous dilation and mild disc swelling. The left eye has a normal appearance (B). Wide angle photography of the periphery highlights the perivenular and macula distribution of the retinal whitening (C)
Case History
A 39 year-old, Latino man presented with acute onset of painless, central vision loss of the right eye. He reported having an acute viral illness that preceded the vision loss by several days, with associated headache, dry cough, arthralgias, and chills. Past ocular and medical histories were otherwise unremarkable. He denied any history of sexually transmitted diseases and had no smoking history. He had chickenpox at age 20.
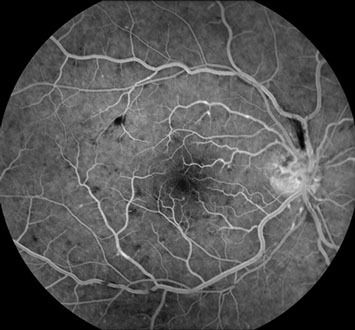
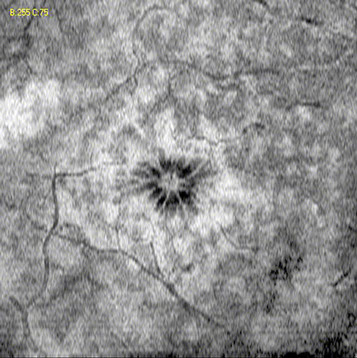
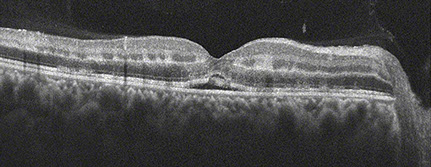
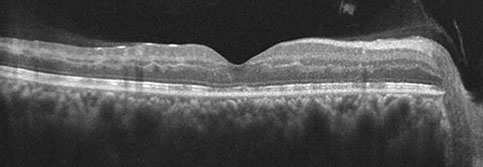
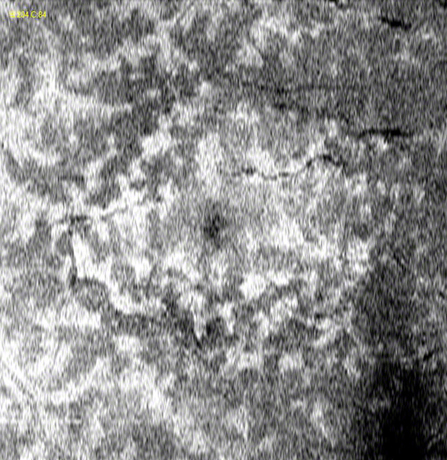
Vision was 5/200 in the right eye and 20/20 in the left eye. Anterior segment examination was unremarkable bilaterally. There was no vitreous cell in either eye. Posterior segment examination of the right eye revealed mild swelling of the superior optic disc with Drance hemorrhage (Figure 1A). There was mild venous dilation and tortuousity in the posterior pole, and scattered dot-blot and flame hemorrhages throughout the fundus (Figure 1C). There was patchy ischemic retinal whitening in the posterior pole that was most prominent along retinal veins. A cotton wool spot was noted inferior to the optic disc. Fluorescein angiography of the right eye revealed mild hyperfluorescence of the disc and multiple foci of late vascular staining and mild leakage, most prominently along the retinal veins (Figure 2A, B). There was blockage of choroidal fluorescence from scattered intraretinal hemorrhages and the cotton wool spot. There were no areas of capillary nonperfusion or delayed retinal filling that corresponded with the areas of patchy ischemic retinal whitening. Mild hypo-autofluorescence was noted within the macula and along the retinal veins (Figure 2C). Spectral domain OCT (SD-OCT) of the right eye demonstrated segmental areas of hyperreflectivity and thickening of the inner nuclear layer (Figure 3A). Intraretinal and subretinal fluid was also present. En face SD-OCT imaging of the inner retina demonstrated patchy hyperreflectivity of the inner nuclear layer, with petalloid hyporeflectivity consistent with cystoid edema of the central macula (Figure 3B). The left eye did not demonstrate any abnormalities.
A

C

B
Figures 2A-C: Fluorescein angiography (A,B) reveals normal antero-venous transit with focal areas of perivenular staining. There was no evidence of macula edema or non-perfusion within the macula. Fundus autofluorescence (C) reveals a fern-like pattern of hypo-autofluorescence along the retinal veins and within the macula.
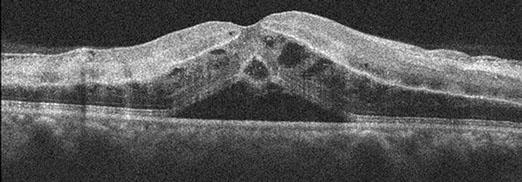
Figures 3A and B: Spectral domain OCT (SD-OCT) of the right eye demonstrated segmental areas of hyperreflectivity and thickening of the inner nuclear layer (3A). Intraretinal and a peculiar pattern of subretinal fluid was also present. En face OCTimaging of the inner retina demonstrated patchy hyperreflectivity, and petalloid hyporeflectivity consistent with cystoid macula edema of the central macula (Figure 3B).
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis for retinal whitening associated with hemorrhage and vasculitis is lengthy and includes; infectious diseases such as herpes simplex virus 1 and 2, varicella zoster virus, cytomegalovirus, syphilis, Mycobacterium tuberculosis; ischemic causes such as retinal vein occlusion, with or without retinal artery occlusion; inflammatory conditions such as sarcoidosis, Behcet’s disease, systemic lupus erythematous and granulomatosis with polyangitis (formerly known as Wegener’s granulomatosis); various blood dyscrasias and trauma (Berlin’s edema).
Our patient received an extensive work up for hypercoagulative, vasculitic, and infectious disorders. This work-up was unrevealing. A clinical diagnosis of non-ischemic central retinal vein occlusion (CRVO) with deep capillary ischemia and paracentral acute middle maculopathy was made.
Discussion
Retinal whitening in CRVO is typically a feature of superficial capillary ischemia resulting in focal cotton wool spots or larger cotton wool spots associated with cilioretinal artery occlusion. Late staining along the retinal veins can also be seen, although usually with moderate to severe degrees of venous occlusion. The deep retinal whitening seen in this case is an uncommon feature of CRVO and differs from the more dense, superficial retinal whitening typical of cotton wool spots. Browning reported 11 cases (4.7%) of CRVO associated with patchy ischemic retinal whitening (PIRW) that is distinct from cotton wool spot formation. These patients were more likely to be young women, and had better final visual acuity. All patients had non-ischemic CRVO (< 10 disc areas of capillary nonperfusion). Cilioretinal artery insufficiency was seen in 5 of 11 patients. Laboratory investigation was generally negative and systemic prednisone was used in eight patients, seven of whom showed visual improvement. PIRW was the earliest clinical sign of CRVO in some cases and typically resolved in 2-4 weeks. Fluorescein angiogram was normal in mild cases, but occasionally demonstrated patches of capillary nonperfusion in more severe cases. Macula edema was occasionally present and typically followed the appearance of PIRW. PIRW was predominantly located along the retinal veins and was postulated to occur because of the relative lower oxygen saturation of the perivenular retinal tissue, especially in the posterior pole, which has higher oxygen demand.
More recently Pichi et al described a case of CRVO with perivenular whitening that corresponded to hyperreflectivity of the inner nuclear and inner plexiform layers, as well as a perivenular, fern-like pattern of blockage on autofluoresence. Similar OCT findings were reported by Sarda et al The hyperreflectivity on OCT is thought to represent deep capillary ischemia within the retina and this finding has been noted in several conditions. Sarraf et al, described 9 patients (11 eyes) with acute macular neuroretinopathy (AMN) who demonstrated either hyperreflectivity above the outer plexiform layer (type -1 lesion) or below the outer plexiform layer (type-2 lesions). They proposed that ischemia of the deep capillary plexus may lead to the development of both type-1 and type-2 lesions. Although these patients all presented with paracentral scotomas and shared many demographic risk factors, patients with type-1 lesions tended to be older males with vascular risk factors, while patients with type-2 lesions tended to be younger, healthy females. However, Tsui et al has reported a single case of AMN with a type-1 lesion in a young, healthy female without known vasculopathy. Yu et al also reported 4 patients (5 eyes) with deep capillary ischemia and OCT lesions nearly identical to those seen in type-1 AMN. These patients usually presented with good central vision, paracentral scotoma and tended to have vasculopathic risk factors. There was no sex predilection. Although none of their cases presented with CRVO, they acknowledge that precapillary arteriolar occlusion can occur from a variety of vascular insults, including, embolization, vasculitis, and vascular endothelial damage, which can be seen in many systemic diseases. Precapillary occlusion can result in superficial capillary ischemia (cotton wool spot) or deep capillary ischemia (paracentral acute middle maculopathy). They proposed that in the acute phase, deep capillary ischemia could be differentiated from superficial capillary ischemia by the presence of mild deep retinal whitening on fundus photography with a relatively normal appearance on fluorescein angiography, mild thickening and hyperreflectivity of the middle retinal layers on SD-OCT, slightly light appearance on red free imaging and slight dark appearance on near infra-red imaging. In the chronic phase, thinning of the middle retinal layers may be the only indication of previous damage.
Clinical Course
Our patient was treated with an 8 week taper of oral prednisone. His OCT at 1 week and 1 month week follow up showed resolution of intraretinal and subretinal fluid and progressive outerplexiform/inner nuclear layer thinning, with (Figure 4A-F). At 2 month follow up his vision improved to the 20/50, although he reported persistent paracentral scotomas.

A
B
C
D
E
F
Figures 4A-F: Fundus photo, SD-OCT and en face OCT imaging through the inner nuclear layer at 1 week (A, C, E) and 1 month (B, D, F) follow up revealed progressive resolution of retinal whitening, intraretinal and subretinal fluid, and outerplexiform/inner nuclear layer thinning, respectively.
Want to Subscribe to Case of the Month?
References
- Browning DJ. Patchy ischemic retinal whitening in acute central retinal vein occlusion. Ophthalmology 2002;109:2154-9.
- Pichi F, Morara M, Veronese C, et al: Perivenular whitening in central vein occlusion described by fundus autofluorescence and spectral domain optical coherence tomography. Retina. 2012;32(7):1438-9.
- Sarda V, Nakashima K, Wolff B, et al: Topography of patchy retinal whitening during acute perfused retinal vein occlusion by optical coherence tomography and adaptive optics fundus imaging. Eur J Ophthalmol 2011;21:653-6.
- Sarraf D, Rahimy E, Fawzi AA, et al: Paracentral acute middle maculopathy: a new variant of acute macular neuroretinopathy associated with retinal capillary ischemia. JAMA Ophthalmol 2013;131:1275-1287.
- Fawzi AA, Pappuru RR, Sarraf D, et al: Acute macular neuroretinopathy: long-term insights revealed by multimodal imaging. Retina 2012;32:1500-1513.
- Tsui I, Sarraf D: Paracentral acute middle maculopathy and acute macular neuroretinopathy. Ophthalmic Surg Lasers Imaging Retina 2013;44:S33-35.
- Yu S, Wang F, Pang CE, et al: Multimodal imaging findings in retinal deep capillary ischemia. Retina 2013:Nov 14. [Epub ahead of print].