West Coast Retina
Case of the Month
April, 2016
Presented by Kevin Patel, MD

A 44 year-old Caucasian man presenting with blurred vision in the right eye.
A
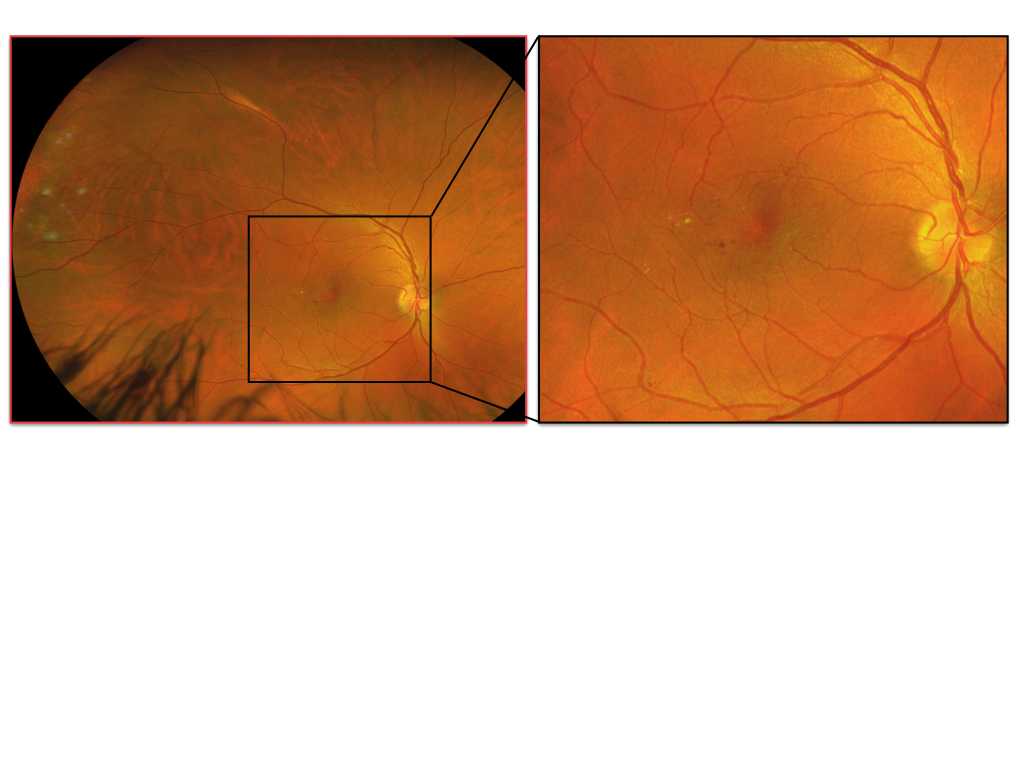
Figures 1A – B: Color fundus photographs of the right (A and inset) and left (B) eyes. The macula of the right eye has several microaneurysms and exudates temporal to the fovea with associated cystoid macular edema (A, inset). The periphery of the right eye shows retinal vascular changes. The posterior segment of the eye is unremarkable (B).
B
Case History:
A 44 year-old Caucasian man presented with a 6-month history of blurred vision of the right eye. It began gradually and remained stable over the past several months. There was no associated pain or other ocular symptoms. The patient denied any changes in vision in his left eye. There was no significant past ocular history. Past medical history was significant for diabetes insipidus. Family and social history were noncontributory.
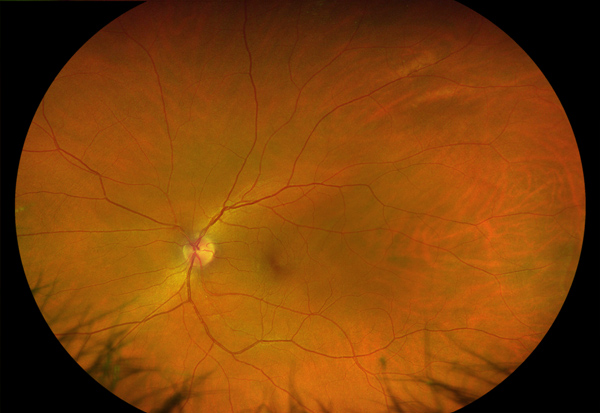
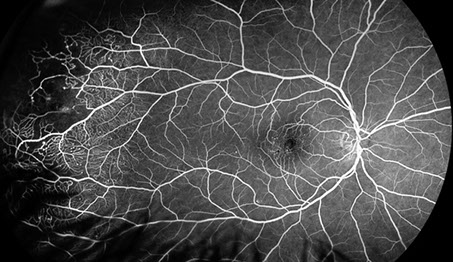
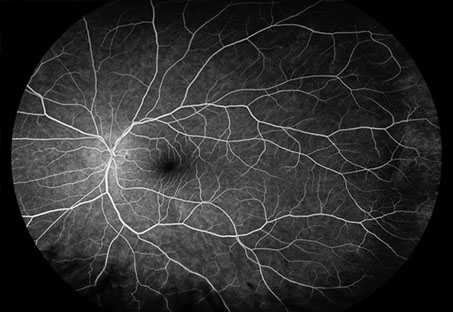
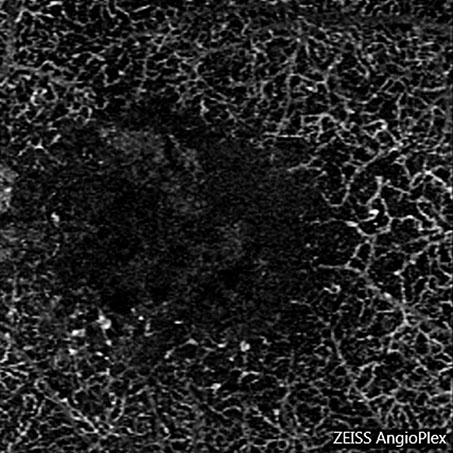
On examination, best-corrected visual acuity was 20/40 in the right eye and 20/20 in the left eye. Intraocular pressure and anterior segment examination were normal in both eyes. Posterior segment examination of the right eye was significant for several microaneurysms and exudates in the temporal macula with associated cystoid macular edema (Figure 1A). The left eye appeared normal (Figure 1B). Wide-field fluorescein angiography of the right eye in early frames revealed microaneurysms in the macula and telangiectatic vascular changes with associated microaneurysms and peripheral nonperfusion temporally (Figure 2A). Late frames displayed leakage in the macula secondary to cystoid macular edema and persistent nonperfusion with microaneurysms in the far temporal periphery (Figure 2B). The left eye was unremarkable (Figure 2C). Optical coherence tomography (OCT) of the right eye demonstrated cystoid macular edema with associated exudates temporally (Figure 3A). OCT of the left eye was normal (Figure 3B). OCT angiography of the right eye was significant for ischemia and telangiectatic changes in the deep capillary plexus (Figures 4A and B). The deep capillary plexus of the left eye was normal (Figures 4C and D).
A
C

B
Figures 2A – C: Wide-field fluorescein angiography of the right (A and B) and left (C) eyes. In early frames of the right eye, there are microaneurysms in the macula and telangiectasis with associated microaneurysms and peripheral nonperfusion temporally (A). Late frames show leakage in the macula consistent with cystoid macular edema and persistent nonperfusion with microaneurysms in the far temporal periphery (B). The left eye appears unremarkable (C).
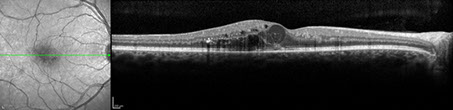
A
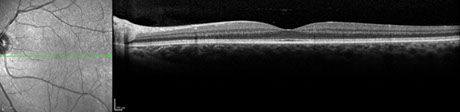
B
Figures 3A – B: Optical coherence tomography of the right (A) and left (B) eyes. The right macula has cystoid macular edema with associated exudates temporally (A). The left macula is normal (B).
B
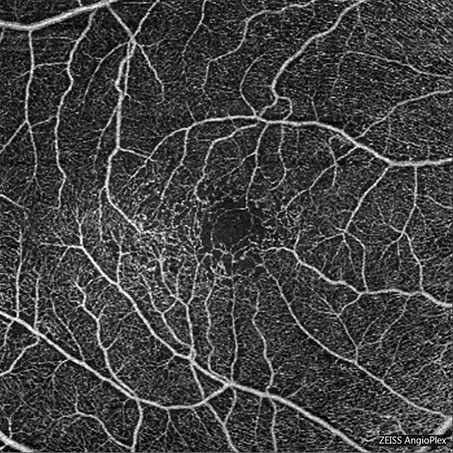
A
Figures 4A – C: Optical coherence tomography angiography of the right (A and B) and left (C) eyes. Fig 4A shows a 6mm x 6mm scan of the superficial capillary plexus. Note the microaneurysms and telangiectasis. Fig 4B is a 3mm x 3mm block segmented at the level of the deep capillary plexus. Note the ischemia and telangiectatic changes in the. Fig 4C shows a 3mm x 3mm scan of the deep capillary plexus in the left eye is normal.

C
What is your Diagnosis?
Differential Diagnosis:
The differential diagnosis for macular telangiectatic changes and exudation is broad. It includes the common vascular conditions of diabetic retinopathy and retinal vein occlusion, and other diseases such as radiation retinopathy, sickle-cell retinopathy, Coats’ disease, and idiopathic macular telangiectasia.
Idiopathic macular telangiectasia can be subdivided into several groups, according to Gass and Blodi: group 1A – unilateral congenital macular telangiectasia; group 1B – unilateral, idiopathic, focal macular telangiectasis; group 2A – bilateral, idiopathic, acquired macular (juxtafoveolar) telangiectasia; group 2B – juvenile occult familial idiopathic juxtafoveolar retinal telangiectasis; group 3A – occlusive idiopathic juxtafoveolar retinal telangectasis; and group 3B – occlusive idiopathic juxtafoveolar retinal telangiectasis associated with central nervous system vasculopathy.1,2 Yannuzzi et al later reclassified idiopathic macular telangiectasia into three types based on new clinical and imaging observations. Groups 1A and B were merged into type 1: aneurysmal telangiectasia; groups 2A and B into type 2: perifoveal telangiectasia; and groups 3A and B into type 3: occlusive telangiectasia.3
Our patient did not have a history of diabetes mellitus, sickle cell disease, or radiation treatment. There was also no evidence of a retinal vein occlusion on fundus examination and ancillary testing. Our patient’s findings of unilateral retinal telangiectasis with exudation in the temporal macula and focal telangiectasias and nonperfusion in the far temporal periphery fall within the spectrum of Coats’ disease. His disease is consistent with type 1 (or group 1A) idiopathic macular telangiectasia, which is considered by many to be a variant of Coats’ disease. Other clinical characteristics of our patient which support this diagnosis are unilateral findings, male gender, having no other vascular systemic disease, and onset of symptoms in early-to-mid adulthood secondary to cystoid macular edema and exudation.2,3
Additional Case History:
After discussion with the patient on possible treatment versus observation of his macular edema and the unknown benefit of treating his condition, it was decided to try a course of anti-VEGF therapy. An intravitreal injection of bevacizumab was given to the patient on his initial visit. He was then scheduled to follow up in one month for continuation of intravitreal bevacizumab treatment.
Discussion:
Idiopathic macular telangiectasia consists of several subgroups of diseases which all develop ectatic and incompetent retinal capillaries in the foveal and perifoveal region which may lead to loss of vision from ischemia and exudation. According to Gass and Blodi, there are groups 1A – 3B.1 Our patient’s presentation most resembled group 1A: unilateral congenital macular telangiectasia, which can be considered a variant of Coats’ disease. Yannuzzi et al would classify this as type 1 idiopathic macular telangiectasia.3 Patients tend to be males with congenital and unilateral retinal telangiectasis in the temporal macula without an underlying systemic disease. There is also multiple capillary, venular, and arteriolar aneurysms in the superficial and deep capillary plexuses. One-third of patients have focal telangiectasis outside of the macula, usually temporally. Mild vision loss can occur secondary to exudation and cystoid macular edema with an onset of symptoms in young adulthood.2,3 Group 1B is called unilateral idiopathic focal macular telangiectasis. In this subgroup, middle-aged men have a very small, focal area of telangiectasis with or without exudation at the edge of the foveal avascular zone. Visual acuity tends to remain very good without the need for treatment.2 In Yannuzzi’s classification, group 1B was grouped into type 1, as it was felt that having a smaller focal area of telangiectasia was just a less severe variant in the spectrum of type 1 idiopathic macular telangiectasia.3
Group 2A, bilateral idiopathic acquired macular (juxtafoveolar) telangiectasia, is the most common subgroup. Patients have bilateral, symmetric area of capillary telangiectasis that is mainly located temporal to the fovea. Mildly blurred vision usually occurs in the fifth or sixth decade of life secondary to minimal intraretinal serous exudation. Right-angle venules, crystalline deposits, and intraretinal pigmented plaques can be seen on examination. Fluorescein angiography demonstrates the parafoveal telangiectasia with associated leakage. OCT shows 'cysts' or hyporeflective spaces in the inner and/or outer retina without associated retinal thickening. In some patients, choroidal neovascularization can develop.2 Group 2B is called juvenile occult familial idiopathic juxtafoveolar retinal telangiectasis. It is similar to group 2A but develops in childhood and does not have right-angle venules, retinal refractile deposits, or stellate pigmented plaques. It was also only described in a pair of two young brothers.2 Because group 2B had only been reported in these pair of siblings, Yannuzzi et al felt that this was a rare familial variant and eliminated the subcategory from their definition of type 2 idiopathic macular telangiectasia.3
Group 3A is known as occlusive idiopathic juxtafoveolar retinal telangiectasis and is very rare. There is bilateral juxtafoveolar retinal telangiectasis with progressive loss of the perifoveolar capillary network. Patients have an associated systemic vascular occlusive or inflammatory disease. Vision loss can be associated with ischemic retinal whitening and occlusion of the perifoveolar retinal capillaries.2 In Group 3B, occlusive idiopathic juxtafoveolar retinal telangiectasis is associated with central nervous system involvement.2 Yannuzzi’s et al omitted these two subgroups from their idiopathic macular telangiectasia classification system. They felt that these conditions only consisted of perifoveal capillary nonperfusion with compensatory dilated capillaries as ocular manifestations of systemic or cerebral familial disease.3
In type 1, or group 1A, idiopathic macular telangiectasia, vision loss is typically secondary to macular edema and exudation. Several treatment options have been suggested for this condition in case reports, however, no treatment has been shown to have consistent visual outcomes. Laser photocoagulation in combination with anti-VEGF therapy was shown to be effective in treating macular edema in a patient with type 1 idiopathic macular telangiectasia. Resolution of edema and stable visual acuity were maintained for three years.4 Anti-VEGF injections alone were found to help eliminate leakage in several other patients, however, visual acuity did not significantly improve.5 In other case series of five eyes, intravitreal anti-VEGF therapy did not improve macular edema, visual acuity, or leakage on FA in the majority of patients.6 Intravitreal corticosteroid treatment with dexamethasone implants was shown to improve anatomical outcomes and reduce macular edema in a patient who did not respond to treatment with anti-VEGF injections. However, similar to the other forms of treatment used in type 1 idiopathic macular telangiectasia, visual acuity failed to improve.7
Take Home Points:
- Idiopathic retinal telangiectasia is a group of diseases that demonstrate telangiectatic changes in the foveal and perifoveal region, often accompanied by macular edema and exudation.
- Group 1A or type 1 idiopathic macular telangiectasia is a rare subgroup that typically presents unilaterally in males during young adulthood.
- While several forms of treatment have been utilized for type 1 idiopathic macular telangiectasia, an option with consistent visual outcomes has yet to be identified
Want to Subscribe to Case of the Month?
References:
- Gass JD, Blodi BA. Idiopathic juxtafoveolar retinal telangiectasis: update on classification and follow-up study. Ophthalmology. 1993;100:1536-46.
- Agarwal A. Gass’ Atlas of Macula Disease, 5th ed. Elsevier; 2012. Pg 522-534.
- Yannuzzi LA, Bardal AM, Freund KB, et al. Idiopathic macular telangiectasia. Arch Ophthalmol. 2006;124:450-60.
- Ciarnella A, Verrilli S, Fenicia V, et al. Intravitreal ranibizumab and laser photocoagulation in the management of idiopathic juxtafoveolar retinal telangiectasia type 1: a case report. Case Rep Ophthalmol. 2012;3:298-303.
- Rouvas A, Malamos P, Douvali M, et al. Twelve months of follow-up after intravitreal injection of ranibizumab for the treatment of idiopathic parafoveal telangiectasia. Clin Ophthalmol. 2013;7:1357-62.
- Takayama K, Ooto S, Tamura H, et al. Intravitreal bevacizumab for type 1 idiopathic macular telangiectasia. Eye. 2010;24:1492-7.
- Loutfi M, Papathomas T, Kamal A. Macular oedema related to idiopathic macular telangiectasia type 1 treated with dexamethasone intravitreal implant (ozurdex). Case Rep Ophthalmol Med. 2014;2014:231913.