West Coast Retina
Case of the Month
August, 2010
Presented by Christian Hester, MD
A 71-year-old Vietnamese man presented with a one-month history of blurred vision and floaters in his left eye
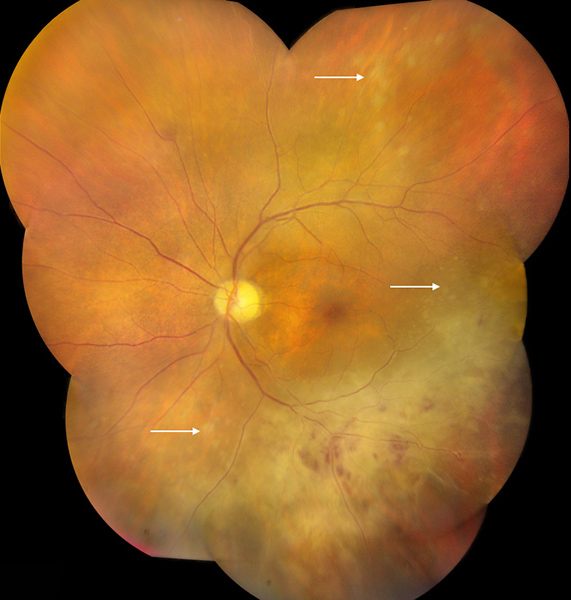
Figure 1A Color photograph montage of the left eye. Note the large area of retinal whitening inferiorly with some intraretinal hemorrhage. Satellite lesions are present more peripherally as well as superotemporally (arrows). The disc appears normal.
Case History
A 71-year-old Vietnamese man presented with a one-month history of blurred vision and floaters in his left eye. He had undergone uncomplicated vitrectomy for symptomatic floaters in the left eye at an outside facility four months prior to presentation. A comprehensive review of systems was unrevealing. His past medical history was notable for recurrent oral herpes, systemic hypertension, a positive Purified Protein Derivative (PPD) test with normal chest x-ray, and hepatitis C that was treated with interferon. Social and family histories were non-contributory.
On examination, best-corrected visual acuity was 20/25 on the right and 20/40 on the left. Intraocular pressure was 13 mm Hg on the right and 15 mm Hg on the left. Examination of the right eye was otherwise unremarkable. Examination of the left anterior segment showed a single granulomatous keratic precipitate and 1+ anterior chamber cellular reaction. Posterior segment examination on the left revealed moderate vitritis, a normal optic disc, and a large area of retinal whitening associated with intraretinal hemorrhages and multiple, small, creamy-yellow satellite lesions at and anterior to the inferior arcade vessels (Figure 1A). Fluorescein angiography (FA) showed staining in the area of retinal whitening and satellite lesions (Figure 1B and 1C). Vascular leakage was not prominent.
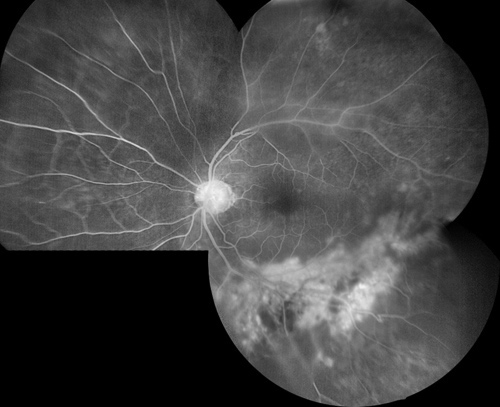
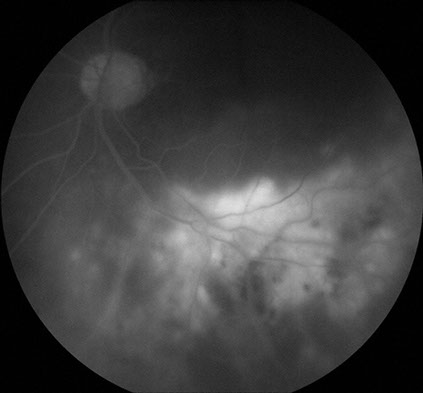
Figure 1B: Fundus angiogram montage of the left eye. The area of retinal whitening shows increased hyperfluorescence, but vascular leakage is not prominent
Figure 1C: Late phase fluorescein angiogram of left eye. The area of retinal whitening show marked hyperfluorescence due to staining, but retinal vascular leakage is minimal and the optic disc shows minimal increased fluorescence.
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis in this patient is broad and includes those entities listed in Table 1. Polymerase chain reaction (PCR) analysis of the aqueous was performed for the detection of herpes simplex virus (HSV), varicella zoster virus (VZV), cytomegalovirus (CMV), Toxoplasma gondii, and Mycobacterium tuberculosis (TB). Additional work-up included serum rapid plasma reagin (RPR), fluorescent treponemal antibody (FTA-ABS), angiotensin converting enzyme (ACE), lysozyme, and human immunodeficiency virus (HIV) antibodies. QuantiFERON Gold testing and chest x-ray were also obtained because of the history of a positive PPD.
Table 1
Infectious
Inflammatory
Infiltrative
Viral
- HSV
- VZV
- CMV
Bacterial
- Syphillis
- Tuberculosis
Parasitic
- Toxoplasmsis
Fungal
- Candida
Sarcoidosis
Behcet's Disease
Vogt-Koyanagi-Harada Syndrome
Primary Intraocular Lymphoma
Clinical Course
The clinical suspicion for acute retinal necrosis (ARN) was high in this patient with recurrent herpetic oral ulcers. An intravitreal injection of foscarnet was administered and treatment with valganciclovir 900 mg PO BID was initiated. One week following the initial presentation, the area of retinal whitening had enlarged slightly. Serum testing for syphilis, sarcoidosis, and HIV as well as PCR analysis of the aqueous for HSV, VZV, CMV, and Toxoplasma Gondii were all unrevealing. The chest x-ray was within normal limits. QuantiFERON Gold testing for TB was positive. Valganciclovir was discontinued and empiric quadruple therapy for TB was initiated. Four weeks following the initial presentation, the best-corrected visual acuity in the left eye had decreased from 20/50 to hand motion. The view to the posterior segment was hazier and the area of retinal whitening enlarged significantly despite treatment (Figure 2). There were several areas of irregularly shaped, creamy-yellow subretinal infiltrates (arrows). At this time, PCR testing of the aqueous for TB returned and was noted to be negative. Magnetic resonance imaging of the brain with and without contrast as well as a lumbar puncture did not show evidence of central nervous system (CNS) lymphoma. A diagnostic vitrectomy was performed and the vitreous biopsy revealed numerous atypical lymphoid cells. A retinal biopsy showed extensive infiltration and necrosis of the retina with lymphoid cells with prominent nuclei and multiple nucleoli, which are features typical of large cell lymphoma (Figures 3A and B). Immunohistochemical staining using an antibody directed against the B-cell antigen, CD20, demonstrated that these cells were neoplastic B-lymphocytes (Figure 3C). The patient was diagnosed with primary intraocular lymphoma (PIOL) and systemic treatment with methotrexate was started.
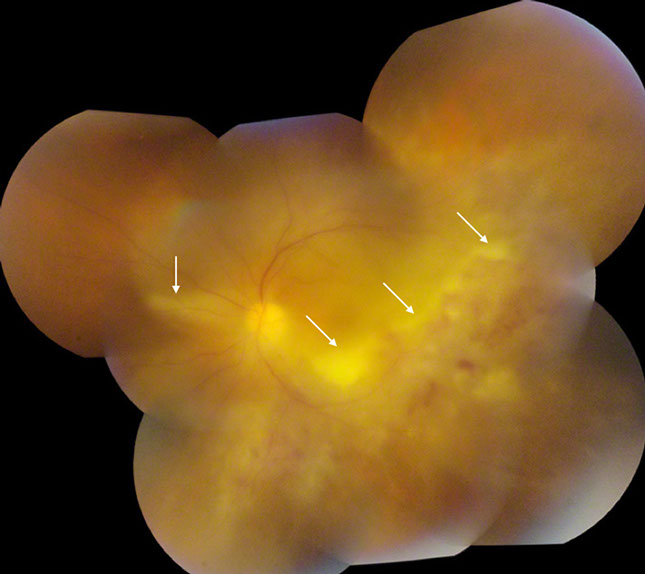
Figure 2: Color photograph montage of the left eye. Four weeks after initial presentation, the extent of retinal whitening is significantly larger. Note the areas of irregularly shaped creamy-yellow subretinal infiltrates (arrows).
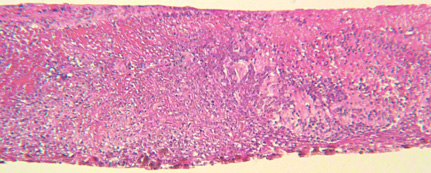
Fig 3A
Figure 3. (A): The retinal biopsy revealed extensive infiltration and necrosis of the retina with atypical lymphoid cells. (B): These cells showed minimal cytoplasm, prominent nuclei, and discrete nucleoli, features typical of large cell lymphoma. (C): Immunohistochemical staining for CD20, an antibody for B-cell, demonstrated these are neoplastic B-lymphocytes. Courtesy of Dr. Narsing Rao, Department of Ophthalmology, USC School of Medicine.
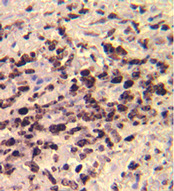
Fig 3C
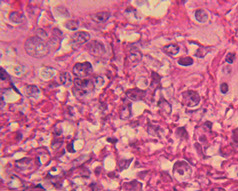
Fig 3B
Discussion
Primary intraocular lymphoma is a subset of primary CNS lymphoma that initially presents with ocular manifestations but without simultaneous CNS involvement. Approximately 60-80% of patients eventually develop CNS lymphoma. It is a rare disease, with an estimated incidence of 30 cases per year in the United States.1 Primary intraocular lymphoma commonly masquerades as uveitis and typical symptoms include blurred vision and floaters. Anterior chamber inflammation is present in 50 to 75% of patients; however, the most common finding is vitritis.2 Lymphoma cells may be seen as sheets and clumps of cells in the vitreous or as multifocal creamy-yellow subretinal infiltrates.3 Fluorescein angiographic abnormalities, which occur due to disturbances of the retinal pigment epithelium, include granularity, small foci of blockage, and late staining.4 Equally important are the lack of signs of inflammation such as vascular leakage and macular edema.4
The diagnosis of PIOL is challenging and requires a high degree of clinical suspicion. The time to diagnosis is often delayed, with a mean of 6 months. The gold standard of diagnosis is based on cytology of an intraocular sample. Diagnostic vitrectomy is the preferred sampling method, as malignant cells are usually found in the vitreous on first clinical presentation. Diagnosis can also be made by lumbar puncture if the CNS is involved. The National Eye Institute recommends that lumbar puncture be performed prior to aqueous or vitreous aspiration or diagnostic vitrectomy, because it is less invasive.5 Primary intraocular lymphoma is usually of monoclonal B-cell origin and stains for B-cell markers are typically positive. Primary intraocular lymphoma can be treated locally, with intravitreal injection of methotrexate, or systemically. A recent study showed no statistical difference in the median survival between patients treated with local versus systemic therapy.1 The prognosis for patients with PIOL is guarded, as the median survival is 58 months.
Take Home Points
- Primary intraocular lymphoma commonly masquerades as uveitis.
- Typical fluorescein angiographic findings include late staining, small foci of blockage and the absence of vascular leakage or macular edema.
- The gold standard for diagnosis is based on cytology of a tissue sample obtained from lumbar puncture, diagnostic vitrectomy, or aqueous or vitreous aspiration.
- The median survival following diagnosis is approximately 5 years.
Want to Subscribe to Case of the Month?
References
- Grimm SA, Pulido JS, Jahnke K, et al. Primary intraocular lymphoma: an International Primary Central Nervous System Lymphoma Collaborative Group Report. Ann Oncol 2007;18:1851-5.
- Rothova A, Ooijman F, Kerkhoff F, Van Der Lelij A, Lokhorst HM. Uveitis masquerade syndromes. Ophthalmology 2001;108:386-99.
- Chan CC, Wallace DJ. Intraocular lymphoma: update on diagnosis and management. Cancer Control 2004;11:285-95.
- Velez G, Chan CC, Csaky KG. Fluorescein angiographic findings in primary intraocular lymphoma. Retina 2002;22:37-43.
- Faia LJ, Chan CC. Primary intraocular lymphoma. Arch Pathol Lab Med 2009;133:1228-32.