West Coast Retina
Case of the Month
Aug, 2015
Presented by Kevin Patel, MD
A 47 year-old Argentinian man presenting with distorted vision in both eyes.

B

A
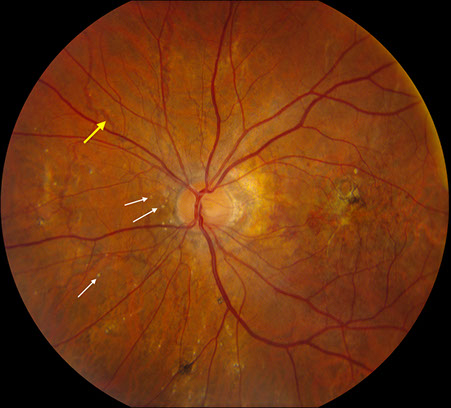
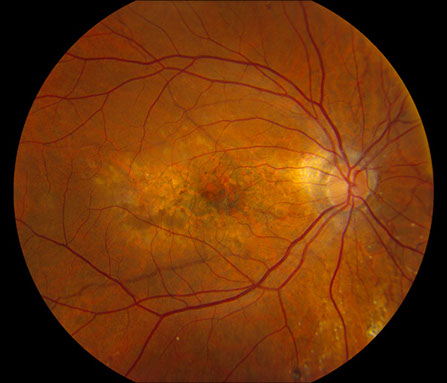
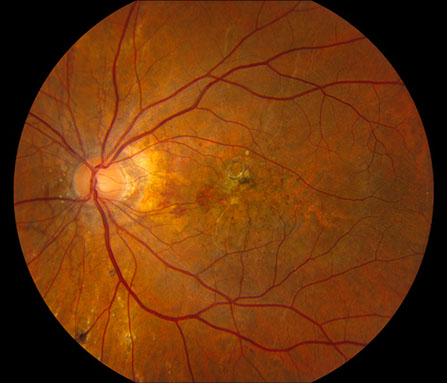
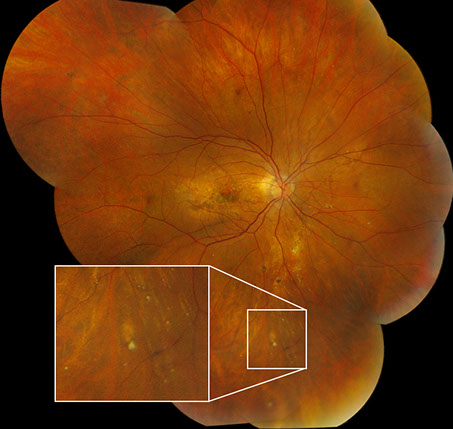
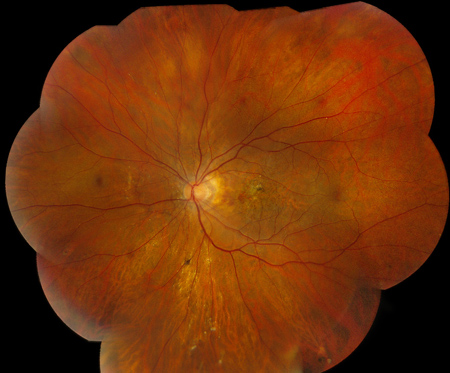
Figures 1A – F: Color fundus photographs of the right (A, C, and E) and left (B, D, and F) eyes. The peripapillary retina of both eyes displayed myopic-appearing optic nerves and angioid streaks (A and B, Yellow arrows). Note the yellow crystalline bodies most readily visible in the posterior pole (white arrows), but also present in the periphery. The macula had areas of RPE atrophy and clumping and subretinal fibrosis bilaterally (C and D). Note the leading edge of atrophy associated with a crystalline body in the periphery of the right eye producing a 'comet' shape (Fig 1E inset).
C
D
E
F
Case History:
A 47 year-old Argentinian man presented with distorted vision in both eyes, but more severe in the left eye, for about 1 week. The patient denied any pain or other ocular symptoms. He had several episodes of this distortion in both eyes starting in 2007. His family and social history were noncontributory, and he took no medications regularly.
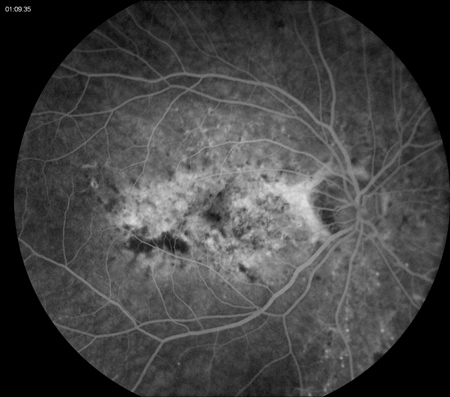
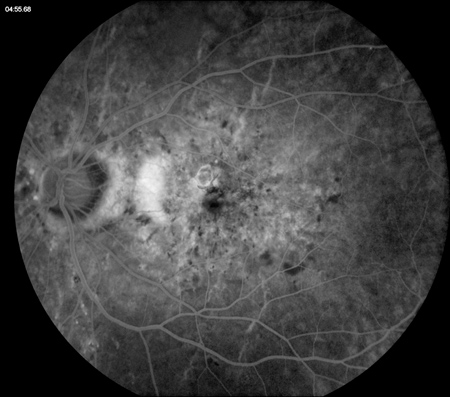
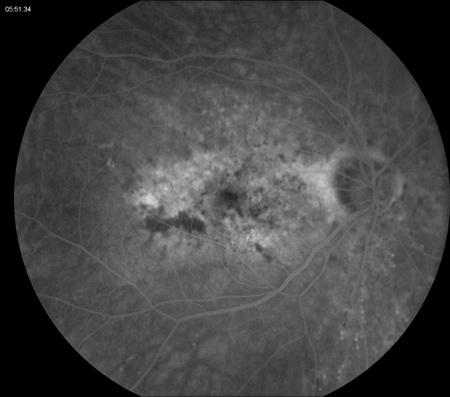
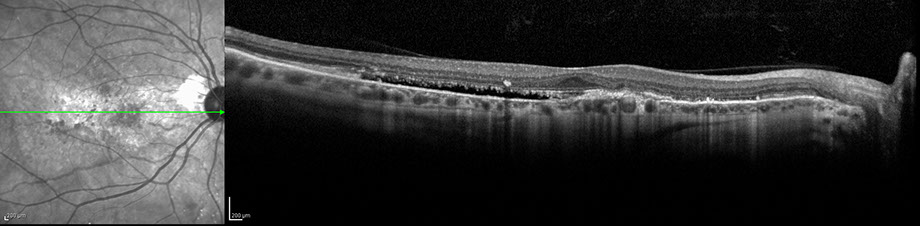
On examination, best-corrected visual acuity was 20/25 bilaterally. Intraocular pressure and anterior segment examination were normal in both eyes. Posterior segment examination was significant for myopic-appearing optic nerves and peripapillary angioid streaks bilaterally (Figures 1A and B). There were retinal pigment epithelial (RPE) changes with hyperpigmentation and subretinal fibrosis in each macula (Figures 1C and D). Multiple yellow crystalline bodies were present in both eyes (Figures 1A, B, E and F). Fluorescein angiography (FA) was remarkable for stippled hyperfluorescence in early and late frames in both eyes consistent with occult choroidal neovascularization (Figures 2A – D). Fundus autofluorescence (FAF) displayed foveal hypoautofluorescence with surrounding hyperautofluorescence in the macula bilaterally (Figures 3A and B). Optical coherence tomography (OCT) was significant for disruption of the outer retina, subretinal fibrosis, and temporal subretinal fluid bilaterally (Figures 4A and B). On external examination, it was noted that the patient had patches of small, yellow papular lesions on both sides of his neck (Figures 5A and B).

A
B
C
D
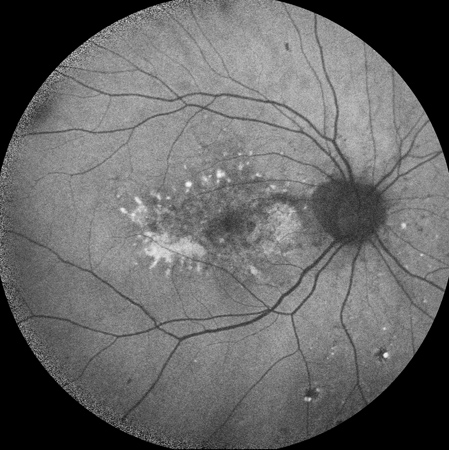
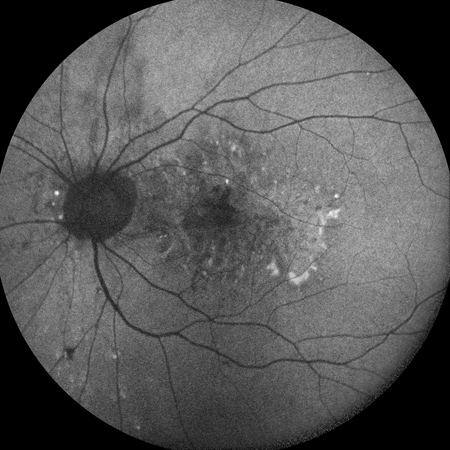
Figures 2A – D: Fluorescein angiogram of the left (A and C) and right (B and D) eyes. Early (A and B) and late (C and D) frames of both eyes revealed stippled hyperfluorescence consistent with occult choroidal neovascularization.
A
B
Figures 3A – B: Fundus autofluorescence of the right (A) and left (B) eyes. There is foveal hypoautofluorescence with surrounding hyperautofluorescence in the macula bilaterally.
A
B
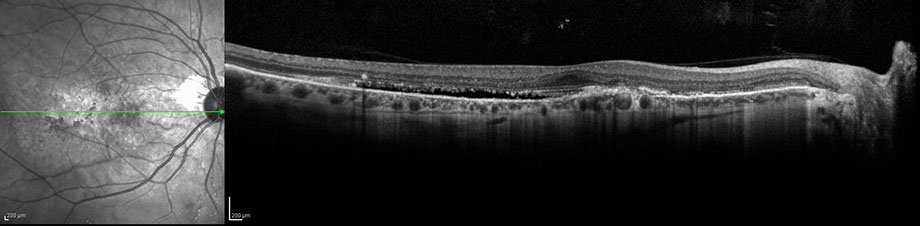
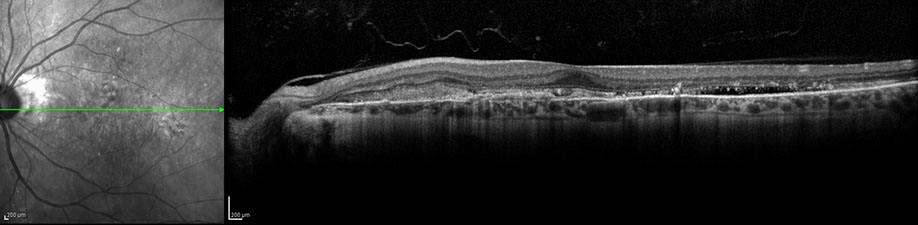
Figures 4A – B: Optical coherence tomography of the right (A) and left (B) eyes at the initial visit. There is disruption of the outer retina, subretinal fibrosis, and temporal subretinal fluid in the right (A) and left (B) macula

A

B
Figures 5A – B: Color external photographs of the right (A) and left (B) sides of the back of the neck. There are symmetric patches of small, yellow papular lesions.
A
B
What is your Diagnosis?
Differential Diagnosis:
Angioid streaks are either idiopathic or caused by a number of systemic conditions, including pseudoxanthoma elasticum (PXE), Ehlers-Danlos syndrome, Paget’s disease, sickle-cell disease, and beta thalassemia. Choroidal neovascularization can arise in areas of angioid streaks in all of these diseases. However, papular skin changes, as seen on the neck of our patient, are commonly seen in patients with PXE.
Additional Case History:
Our patient had a well-documented history of pseudoxanthoma elasticum with angioid streaks complicated by several recurrences of choroidal neovascularization in both eyes previously treated with intravitreal bevacizumab.
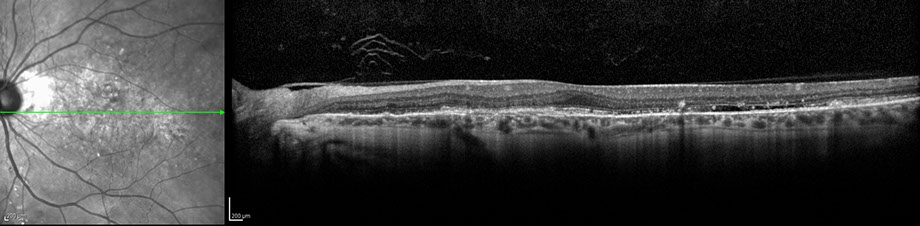
Our patient was initially treated with intravitreal bevacizumab bilaterally and returned to clinic for follow up in one month. On examination, best-corrected visual acuity was 20/20 bilaterally, but the patient still complained of distorted vision in both eyes. The OCT on his follow-up visit displayed persistent temporal subretinal fluid in both macula (Figures 6A and B). After discussion with the patient about possible treatment options, intravitreal ranibizumab was given bilaterally with plans for follow up in one month. In addition, because of concern for potential systemic complications from PXE, it was recommended to our patient that he see an internist to facilitate appropriate cardiac and gastrointestinal testing.
Discussion:
Pseudoxanthoma elasticum is a hereditary systemic disease caused by a mutation in the ABCC6 gene, which encodes for a protein in the C-family of adenosine triphosphate-binding cassette proteins. PXE predominantly affects the eyes, skin, and cardiovascular system. Histologically, the changes seen in PXE are caused by degeneration and calcification of the elastic tissue of the dermis, which can lead to premature calcification of large arteries. Such changes in the cardiovascular system may cause intermittent claudication and coronary artery disease. Gastrointestinal bleeding is another systemic complication of PXE. The earliest manifestation of PXE occurs in the skin, where confluent, yellowish papules develop on the flexural surfaces in the neck, antecubital fossa, and periumbilical area. This gives the skin a “plucked chicken” appearance.1
Characteristic ophthalmic findings in PXE predominantly involve the retina. Angioid streaks are common. These irregular, radiating, jagged lines extend from the peripapillary area into the peripheral retina. They are caused by discrete linear breaks in Bruch’s membrane. A frequent complication of angioid streaks is the development of choroidal neovascularization (CNV) that grows into the sub-RPE or subretinal space. Serous and hemorrhagic detachments of the RPE adjacent to these neovascular membranes are the predominant cause of vision loss.2 An additional retinal finding in PXE is the “peau d’orange” pigmentary change caused by multiple, indistinct, yellowish lesions of the RPE. This widespread mottling of the fundus, which is usually most apparent in the mid-peripheral fundus especially temporally, is likened to that of an orange skin (peau d’orange). Patients with PXE have also been reported to have optic nerve head drusen, focal atrophic RPE lesions, and crystalline bodies as was seen in our patient.1 These crystalline bodies frequently have a leading area of RPE atrophy producing a streaking comet appearance.
McDonald et al described reticular-like pigmentary patterns in the fundus of 9 patients with PXE.3 More recently, Agarwal et al reported that PXE can display a wider spectrum of pattern dystrophies. These include fundus pulverulentus, butterfly-shaped dystrophy, fundus flavimaculatus, reticular dystrophy, and vitelliform pattern dystrophy.4
Intravitreal injections of anti-vascular endothelial growth factor (VEGF) medications have been proven to be highly effective for treatment of CNV secondary to age-related macular degeneration. These studies did not evaluate the efficacy of anti-VEGF medications in treating CNV in PXE. However, case series have described successful treatment of CNV secondary to angioid streaks in PXE.5
Take Home Points:
- Pseudoxanthoma elasticum is a hereditary systemic disease that can affect the eyes, skin, and cardiovascular system.
- There are many ophthalmic manifestations of PXE, the most common being angioid streaks.
- Vision loss in PXE is most often caused by the development of choroidal neovascularization as a complication of angioid streaks.
- Intravitreal bevacizumab has been shown to be effective in treating CNV in PXE.
Want to Subscribe to Case of the Month?
References:
- Agarwal A. Gass’ Atlas of Macula Diseases, 5th ed. Elsevier; 2012. Pg. 146-50.
- Agarwal A. Gass’ Atlas of Macula Diseases, 5th ed. Elsevier; 2012. Pg. 142.
- McDonald HR, Schatz H, Aaberg TM. Reticular-like pigmentary patterns in pseudoxanthoma elasticum. Ophthalmology. 1988;95:306-11.
- Agarwal A, Patel P, Adkins T, Gass JD. Spectrum of pattern dystrophy is pseudoxanthoma elasticum. Arch Ophthlamol. 2005;123:923-8.
- Finger RP, Charbel Issa P, Schmitz-Valckenberg S, et al. Long-term effectiveness of intravitreal bevacizumab for choroidal neovascularization secondary to angioid streaks in pseudoxanthoma elasticum. Retina. 2011;31:1268-78.