West Coast Retina
Case of the Month
December, 2013
A 68 year-old, woman with progressive vision loss in both eyes
Presented by Steven Williams, MD


A

B
Figures 1A and B: Color fundus photograph of right and left macula and nerve. Both eyes demonstrate macula granular pigmentary change with surrounding chorioretinal atrophy.
Case History
A 68 year-old, Caucasian woman presented with progressive vision loss in both eyes for several months. Her vision continued to decline despite cataract surgery in both eyes. Her past medical history included hypertension, hypercholesterolemia and bipolar disorders. Her medications included losartan, sertraline, quetiapine, simvastatin, felodipine, and loratadine.
Vision in the right eye was 20/125 in the right eye and 5/200 in the left eye. Anterior segment examination was remarkable for well-centered posterior chamber intraocular lenses. There was no vitreous inflammation in either eye. Fundus examination revealed marked macular pigment granularity and mottling (Figure 1A, B). There were areas of diffuse geographic or nummular chorioretinal atrophy in the periphery of both eyes, which enhanced the visibility of the large choroidal vessels. There was also moderate arteriolar attenuation (Figure 2, B). Spectral domain OCT demonstrated diffuse atrophy of the outer retina/RPE, with relative preservation of the central foveal photoreceptor/RPE layers (Figure 3A, B). Retinal fluorescein angiography demonstrated large geographic areas of hypofluorescence, which correspond to retinal atrophy and loss of the choriocapillaris (Figure 4A, B). Humphrey automated perimetry showed generalized depression of the visual field in both eyes. The electroretinogram demonstrated marked flattening of scotopic and photopic responses.

A

B
Figures 2A and B: Color montage photographs of both eyes demonstrate extensive, geographic atrophy of the retinal pigment epithelium. The large choroidal vessels have a prominent appearance, suggesting concomitant loss of the choriocapillaris.
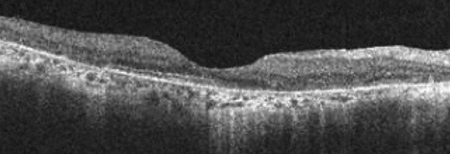
B
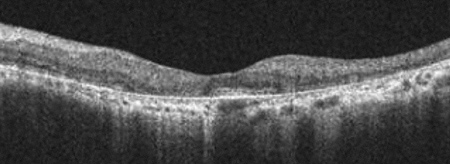
A
Figures 3A and B: Spectral domain OCT of each eye demonstrates diffuse photoreceptor and RPE atrophy with marked retinal thinning. The central subfoveal photoreceptor cell layer is relatively preserved.
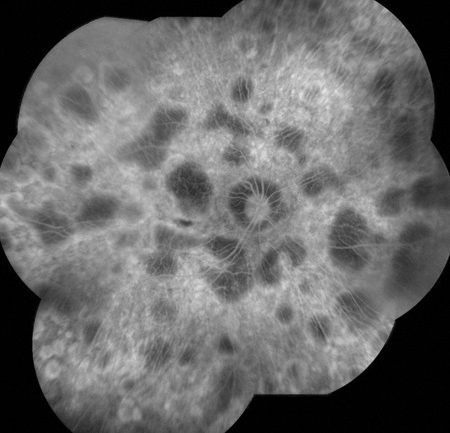
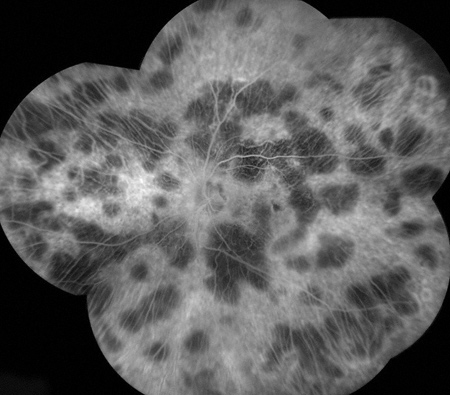
Figures 4A and B: Montaged fluorescein angiogram of each eye demonstrates geographic areas of hypofluorescence due to loss of the choriocapillaris. The large choroidal vessels are most visible in the areas of hypofluoresence.
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis for symmetrical, presumably progressive, chorioretinal atrophy includes hereditary tapetoretinal degenerations, such as retinitis pigmentosa, refsum disease, hereditary abetalipoproteinemia, gyrate atrophy, Bietti’s crystalline dystrophy, choroideremia, Kearns-Sayre syndrome and Stargardt disease; toxic or drug related retinopathies, such as thioridazine (Mellaril), chlorpromazine (thorazine), clofazimine, chloroquine; as well as infectious etiologies including, syphilis and congenital rubella.
Upon further investigation, our patient reported a history of bipolar disorder with psychotic features and was treated with Mellaril, dose ranging from 200-300 mg bid or tid for 40 years. The medication was discontinued three years prior. Of note is that her body weight was relatively constant at approximately 100 pounds (45 kg) over the years of thioridizine usage.
Discussion
Thioridazine (Mellaril) has been used in the treatment of psychosis and schizophrenia since 1959. It is a typical antipsychotic medication in the phenothiazine class and has activity as a central adrenergic, dopamine-blocking and minor anticholinergic agent. Due to cardiovascular toxicity (e.g., QTc interval prolongation, orthostatic hypotension), extrapyramidal side effects (e.g., tardive dyskinesia), degenerative retinopathy, and the development of more well tolerated anti-psychotics agents, its use has dramatically decreased. Mellaril inhibits oxidative phosphorylation in the retina, resulting in abnormal rhodopsin synthesis and photoreceptor outer segment destruction. Chorioretinal toxicity may also be related to increased drug concentration within melanin granules in the RPE and uveal melanocytes.
Patients who develop acute retinopathy usually develop nyctalopia, blurred vision or dyschromatopsia (brownish color) 3-8 weeks after receiving a daily dose in excess of 800-1000 mg. It appears that maximal daily dose is more critical than cumulative dose. Over time, a granular, salt and pepper pigmentary retinopathy develops in the macula and sometimes in the periphery. The retinopathy progresses to include patchy loss of RPE and choriocapillaris and eventual diffuse nummular or tapetoretinal degeneration with areas of hypo- or hyperpigmentation. Fluorescein angiography may demonstrate subtle RPE alterations early in the disease course, progressing to geographic areas of RPE/choriocapillaris atrophy. Vision may continue to worsen, but occasionally improves with medication discontinuation. During the first year after thioridazine exposure, visual function and electroretinogram may show improvement even as pigmentary changes progress. However, ERG response is commonly severely attenuated late in the disease course.
Take Home Points
- Thioridazine (Mellaril) toxicity is an uncommon but well-known cause of drug induced chorioretinopathy.
- Clinical features of Mellaril toxicity include granular pigmentary changes and diffuse tapetoretinal degeneration.
- Visual function and ERG findings may be relatively preserved even with progressive chorioretinopathy.
Want to Subscribe to Case of the Month?
References
- Davidorf FH. Thioridazine pigmentary retinopathy. Arch Ophthalmol. 1973 Sep;90(3):251–255.
- Meredith TA, Aaberg TM, Willerson WD. Progressive chorioretinopathy after receiving thioridazine. Arch Ophthalmol. 1978 Jul;96(7):1172–1176.
- Kozy D, Doft BH, Lipkowitz J. Nummular thioridazine retinopathy. Retina. 1984 Fall-Winter;4(4):253–256.
- Marmor MF. Is thioridazine retinopathy progressive? Relationship of pigmentary change to visual function. Br J Ophhtalmol 1990;74:739-42.