West Coast Retina
Case of the Month
February, 2010
Presented by Jon Wender, MD
A 62 year-old man with 2 weeks of decreasing vision in his left eye.
A
B
C
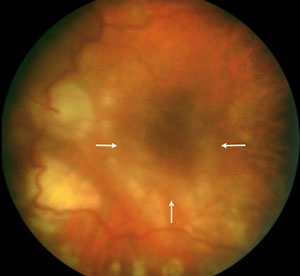
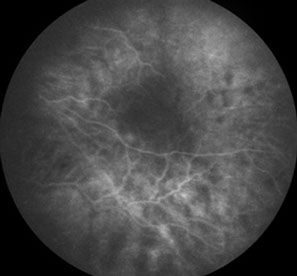
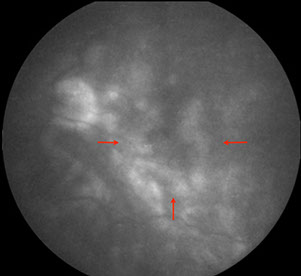
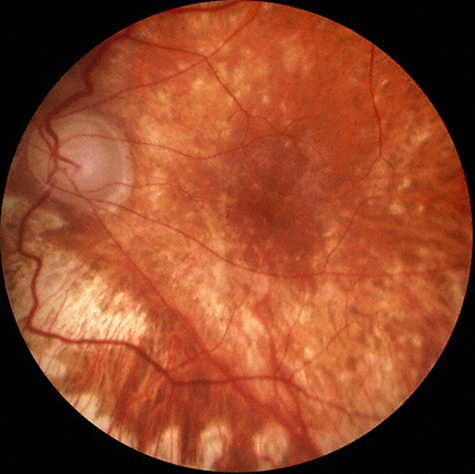
Figures 1A-C: The media of the left eye is hazy due to inflammation. Retinal whitening is present surrounding the fovea (Fig. 1A, arrows). The fluorescein angiogram in the late phases shows progressive fluorescence of the optic disc and perifoveal area due to inflammation (Arrows, Fig. 1C.
Case History
A 62-year-old man presented with a 2-week history of decreasing vision in his left eye. His past ocular history was significant for repair of a retinal detachment with pars plana vitrectomy, scleral buckle, and endolaser 3 months earlier. A retinal break had been treated with laser and cryopexy 4 months prior to presentation. He had pathologic myopia, bilateral aphakia after cataract extraction, and ocular hypertension, which was treated with topical medications. The patient’s past medical history was unremarkable.
On examination, best-corrected visual acuity was 20/20 in the right eye and 20/400 in the left eye. Intraocular pressure was 19 mm Hg in the right eye and 3 mm Hg in the left eye. Anterior segment examination of the right eye was unremarkable. Posterior segment examination of the right eye revealed mild atrophic changes consistent with high myopia. Anterior segment examination of the left eye revealed large granulomatous keratic precipitates and severe anterior chamber cell and flare. Posterior segment examination on the left showed macular edema, an attached retina and mild chorioretinal atrophy associated with high myopia (Fig 1A). Fluorescein angiography of the left eye demonstrated progressive staining from both the optic disc and perifoveal area. A posterior subtenon’s injection of triamcinolone was administered to the left eye. Five days later, the inflammation was significantly improved. (Fig. 2).
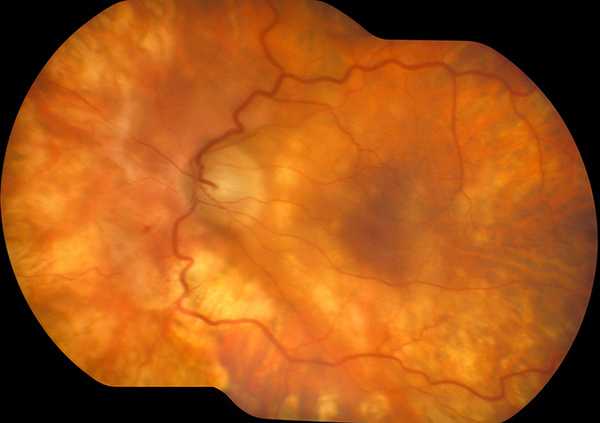
Figure 2: Five days later, the inflammation has decreased significantly. The media is clear, and the retinal whitening has almost completely resolved.
Case History (Continued)
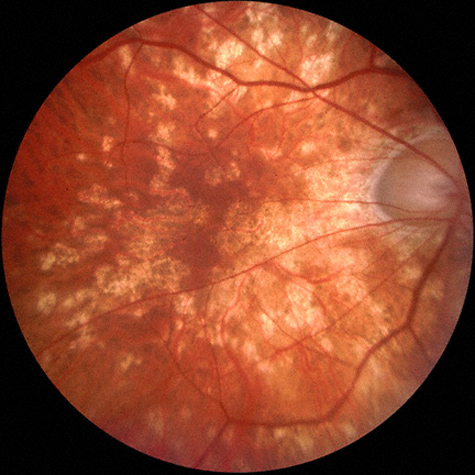
Three weeks later, the patient noted new scotomata in the right eye. At that time, the visual acuity was found to be 20/50 in the right eye and 20/125 in the left eye. Examination of the right eye revealed mild anterior chamber cell and flare as well as multiple chorioretinal lesions (Fig. 3A). In the left eye, the anterior chamber reaction and vitritis had resolved and the retina remained attached (Fig 3B). At this point, a posterior subtenon’s injection of triamcinolone acetonide was administered to the right eye.
In summary, a 62-year-old man presented with an acute bilateral granulomatous panuveitis associated with multiple chorioretinal lesions following multiple eye surgeries, the most recent of which was a gas-fluid exchange 11 weeks prior to the onset of symptoms.
B
A
Figures 3A and B: Fundus photographs of the right and left eye. Three weeks later, the inflammation is significantly improved in the left eye, but anterior segment inflammation has developed in the right eye. Note the multiple chorioretinal scars in the right macula (Fig. 3A).
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis includes multifocal choroiditis, birdshot chorioretinopathy (BSC), sarcoidosis, sympathetic ophthalmia (SO), tuberculosis, and syphilis.
Laboratory investigations, including an FTA-ABS, a serum angiotensin converting enzyme (ACE) level, and a chest x-ray, were all normal.
Given the history of multiple recent surgical procedures, the clinical course involving subsequent inflammation in the fellow eye, as well as the clinical findings of granulomatous inflammation and characteristic chorioretinal lesions, a diagnosis of sympathetic ophthalmia was made. Oral prednisone was initiated at 80 mg per day, and tapered gradually. Additional immunosuppressive agents, including cyclosporin A and chlorambucil, were also required in order to control the intraocular inflammation. Six months after the initial presentation, the visual acuity was 20/100 in the right eye and 8/200 in the left eye with no evidence of active inflammation, either clinically or on fluorescein angiography.
Discussion
Sympathetic ophthalmia is a rare cause of sight-threatening bilateral granulomatous uveitis that may occur between two weeks and several years following surgical or non-surgical trauma.1,2 The pathophysiology of SO is unclear, but is likely related to exposure of previously sequestered uveal antigens, which results in immune sensitization and intraocular inflammation.3
The epidemiology of SO is changing. Whereas non-surgical ocular injuries in young patients were previously thought to account for the majority of cases of SO, there is increasing evidence that ocular surgery, and vitreoretinal surgery has become a more common cause.4-6 Kilmartin and associates estimated a risk of SO of one in 1,152 eyes that undergo any retinal surgical procedure and one in 799 eyes undergoing pars plana vitrectomy.7
A high index of suspicion of SO is required because the clinical manifestations can be variable and may consist only of anterior chamber inflammation or vitritis.2,5 In a recent review by Castiblanco and colleagues, anterior chamber and vitreous inflammation, each occurring in roughly half of cases, were the most common clinical findings in eyes with SO. Approximately, one-third of eyes in that review presented with multifocal choroiditis consistent with Dalen-Fuchs nodules similar to our patient, whereas only one in ten eyes show serous retinal detachment.2
The visual prognosis of SO has been improving in recent years, in part, due to prompt and routine implementation of systemic immunosuppressive therapy.2,4,6,8 In the review by Castiblanco and colleagues, 95% of patients were treated with systemic corticosteroids and 75% with non-corticosteroid immunosuppressive agents.2 Accordingly, 70% of patients in that review experienced an improvement in visual acuity in the sympathizing eye. Similarly, in a recent case series by Galor and associates, greater than half of patients maintained a final visual acuity of 20/50 or better in the sympathizing eye.8
Take Home Points
- Sympathetic ophthalmia is a rare but potentially devastating cause of post-operative or post-traumatic bilateral granulomatous uveitis.
- Current data indicate that most cases of SO are related to ophthalmic surgery and that vitreoretinal surgery may be associated with a particularly high risk.
- A high index of suspicion of SO is required to make the diagnosis since most patients have intraocular inflammation only, whereas a minority have the characteristic findings of Dalen-Fuchs-like areas of chorioretinitis or serous retinal detachment.2, 5
- Prompt and appropriate treatment with systemic immunosuppressive agents has led to improved visual outcomes in recent years in patients with SO.
Want to Subscribe to Case of the Month?
References
- Chu DS, Foster CS. Sympathetic ophthalmia. Int Ophthalmol Clin 2002;42(3):179-85.
- Castiblanco CP, Adelman RA. Sympathetic ophthalmia. Graefes Arch Clin Exp Ophthalmol 2009;247(3):289-302.
- Ramadan A, Nussenblatt RB. Visual prognosis and sympathetic ophthalmia. Curr Opin Ophthalmol 1996;7(3):39-45.
- Kilmartin DJ, Dick AD, Forrester JV. Prospective surveillance of sympathetic ophthalmia in the UK and Republic of Ireland. Br J Ophthalmol 2000;84(3): 259-63.
- Ozbek Z, Arikan G, Yaman A, et al. Sympathetic ophthalmia following vitreoretinal surgery. Int Ophthalmol 2009.
- Vote BJ, Hall A, Cairns J, Buttery R. Changing trends in sympathetic ophthalmia. Clin Experiment Ophthalmol 2004;32(5):542-5.
- Kilmartin DJ, Dick AD, Forrester JV. Sympathetic ophthalmia risk following vitrectomy: should we counsel patients? Br J Ophthalmol 2000;84(5):48-9.
- Galor A, Davis JL, Flynn HW, Jr., et al. Sympathetic ophthalmia: incidence of ocular complications and vision loss in the sympathizing eye. Am J Ophthalmol 2009;148(5):704-10 e2.