West Coast Retina
Case of the Month
February, 2013
Presented by Ako Takakura, MD, MPH
46-year-old African-American man referred with persistently decreased vision in his left eye for two months following uncomplicated trabeculectomy surgery.

Figure 1: Color photo of the left macula showing a ‘salt-and-pepper’ pattern pigmentation, severe optic disc cupping related to long-standing glaucoma, and a serous macular detachment. There was no evidence of vitritis, or of prior or active retinal or choroidal inflammation.
Case History
A 46-year-old African-American man presented for evaluation of persistently decreased vision in the left eye following uncomplicated trabeculectomy surgery with Mytomycin-C two months earlier. Past ocular history was notable for long-standing glaucoma. Past medical history was notable for congenital heart disease and long-standing bilateral hearing loss.
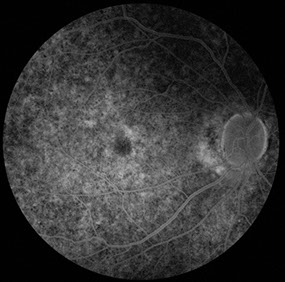
Best-corrected vision was 20/20 in the right eye and hand motion at 2 feet in the left eye. Intraocular pressure (IOP) was 16 mm Hg on the right and 14 mmHg on the left. Anterior segment examination of the right eye showed no anterior chamber cell, diffuse iris atrophy with loss of iris crypts, and mild nuclear sclerotic cataract. Anterior segment examination on the left revealed mild conjunctival injection, a well-formed avascular bleb superiorly, no anterior chamber cell, and diffuse iris atrophy and mild nuclear sclerotic cataract similar to the right eye. Posterior segment examination on the right showed no vitreous inflammation, widespread retinal vascular attenuation, and salt-and-pepper retinopathy (Fig. 2). Posterior segment examination on the left revealed occasional vitreous cells, widespread retinal vascular attenuation, salt-and-pepper retinopathy, severe optic disc cupping, and a serous macular detachment (Fig. 1).
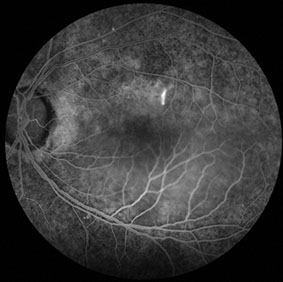
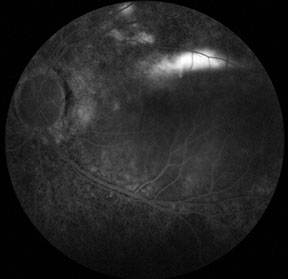
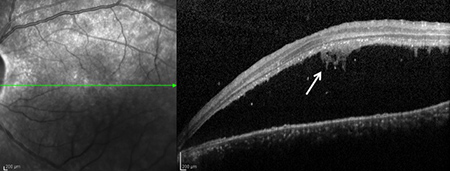
Fluorescein angiography (FA) on the right showed changes consistent with widespread alterations in the RPE, but was otherwise unremarkable. Fluorescein angiography on the left eye showed similarly widespread changes consistent with salt-and-pepper retinopathy, an early 'smoke-stack' pattern of hyperfluorescence with progressive filling of the serous detachment space, and areas of late patchy hyperfluorescence at the superonasal edge of the detachment space (Fig. 3). Spectral domain optical coherence tomography (SD-OCT) of the left eye confirmed the presence of a serous retinal detachment with amorphous material adherent to the under surface of the detached retina, as well as isolated retinal pigment epithelial (RPE) detachments in the area of late patchy hyperfluorescence seen on FA (Fig. 4). B-scan ultrasonography also demonstrated the serous retinal detachment on the left, but showed no evidence of posterior eye wall thickening or of retrobulbar fluid.

Figure 2: Color photo of the right macula revealing similar alterations in the RPE, but no optic disc pallor or evidence of serous retinal detachment.
A
B
C
Figures 3A-C: Mid- and late-phase fluorescein angiograms showing widespread changes consistent with salt-and-pepper retinopathy. In the mid-phase frame of the left eye, a ‘smoke-stack’ pattern of hyperfluorescence is noted with progressive filling of the serous detachment along with areas of late patchy hyperfluorescence at the superotemporal edge of the detachment space.
A
B
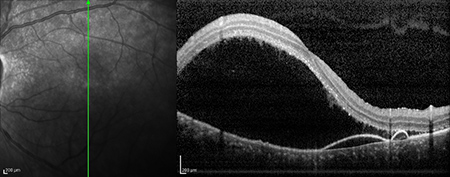
Figures 4A and B: Horizontal (A) and vertical (B) Spectral Domain - Optical Coherence Tomography (SD-OCT) of the left eye showing a serous retinal detachment with amorphous material adherent to the undersurface of the detached retina (arrow). The vertical scan B) shows isolated pigment epithelial detachments.
What is your Diagnosis?
Differential Diagnosis
The findings of serous retinal detachment, associated with localized detachments of the RPE, and the classic smoke-stack appearance on the FA are typical features of central serous chorioretinopathy (CSCR). Other considerations would include hypotony maculopathy, which is perhaps the most common cause of serous macular detachment following trabeculectomy surgery. However, it is not associated with RPE detachments or a smoke-stack pattern of leakage on FA, and would be uncommon given the lack of retinal folds or striae and our patient's IOP of 14mmHg.1,2 Serous detachments can also occur in nanophthalmos,3–5 or microphthalmos,6,7 but tend not to show either RPE detachments or focal RPE leaks characteristic of CSCR. Sympathetic ophthalmia and Vogt-Koyanagi-Harada disease can cause serous retinal detachment accompanied by vitritis, and rarely can be asymmetric or unilateral,8 but would not be expected to produce RPE detachments or a smoke-stack on FA. Furthermore, no ophthalmoscopic or angiographic evidence of inflammation was found. B-scan ultrasonography showed no evidence of posterior scleritis.
Clinical Course
Given the patient's history of congenital heart disease and long-standing hearing loss, together with bilateral pigmentary retinopathy and long-standing glaucoma, an A-scan ultrasound was performed and demonstrated an axial length of 21.78 mm on the right and 19.71 mm on left eye - confirming microphthalmos and further supporting the diagnosis of congenital rubella.
Discussion
This is a case of central serous chorioretinopathy (CSCR) following uncomplicated trabeculectomy in a patient with microphthalmos and long-standing glaucoma in the setting of congenital rubella.
Congenital rubella syndrome was first described by the Australian ophthalmologist Norman Gregg in 1941.9 Gregg noted a direct relationship between congenital cataract and maternal infection with German measles. Congenital rubella syndrome can have many systemic manifestations, but is commonly associated with congenital heart defects, hearing loss, neurologic deficits and ocular complications, including congenital cataracts, glaucoma, pigmentary retinopathy, and microphthalmos.10 The last major rubella epidemic in the United States was in the mid-1960's11 and although we have no serologic evidence of infection in our patient, our patient was born in 1964 and had many of signs of this distinctive syndrome.
The occurrence of CSCR in the setting of a small eye is rare, but has been described previously.12 Blair et al described a case of a 11-year old boy with Hallermann-Streiff syndrome - a rare disorder characterized by bird-like facies, dental anomalies, dwarfism, congenital cataract, microphthalmos, hypotrichosis and cutaneous atrophy. Their patient presented with central serous choroidopathy characterized by profuse leakage through the RPE on fluorescein angiogram in an eye with an axial length 14.5 mm.12
Central serous chorioretinopathy has also been reported following glaucoma surgery.13 Aydin and associates described a patient with 'central serous retinal detachment' that occurred following trabeculectomy surgery for traumatic glaucoma. It should be noted, however, that the patient had 'profound' post-operative hypotony and that the choroidal leakage suggestive of CSCR occurred from an area of the RPE damaged during the preceding trauma. Of note, while the hypotony resolved within one week of glaucoma surgery, the serous retinal detachment persisted for two months.13
Take Home Points
- Central serous chorioretinopathy can occur in anatomically small eyes, and/or following trabeculectomy surgery.
- Congenital rubella should be considered and axial lengths obtained in patients with other changes consistent with congenital rubella, including pigmentary retinopathy, congenital glaucoma, heart disease, and/or hearing loss.
Want to Subscribe to Case of the Month?
References
- Suner I, Greenfield D, Miller M, Nicolela M, Palmberg P. Hypotony Maculopathy after Filtering Surgery with Mitomycin C: Incidence and Treatment. Ophthalmology 1997;104(2):207–15.
- Costa VP, Arcieri ES. Hypotony maculopathy. Acta Ophthalmologica Scandinavica 2007;85(6):586–97.
- Han L, Fraco JDC. Nanophthalmos with longstanding choroidal effusion and serous retinal detachment. Aust N Z J Ophthalmol 1997;25:15–7.
- Krohn J, Seland J. Exudative retinal detachment in nanophthalmos. Acta Ophthalmologica Scandinavica 1998;76(4):499–502.
- Uyama M, K T, Kozaki J, et al. Uveal Effusion Syndrome: Clinical Features, Surgical Treatment, Histologic Examination of the Sclera, and Pathophysiology. Ophthalmology 2000;107(3):441–9.
- Nishina S, Suzuki Y, Azuma N. Exudative retinal detachment following cataract surgery in Hallermann-Streiff syndrome. Graefe’s Archive for Clinical and Experimental Ophthalmology 2008;246(3):453–5.
- Marc C, Guigou S, Boulicot C, Denis D. Bilateral retinal detachment in Hallermann-Streiff-François syndrome: A case report. Journal Français d’ophtalmologie 2011;34:118–21.
- Roe RH, Rathinam SR, Wong RW, McDonald HR, Jumper JM, Cunningham Jr ET. Delayed fellow eye involvememt in patients with Vogt-Koyanagi-Harada disease. The British Journal of Ophthalmology 2009;93(5):701–2.
- Gregg N. Congenital cataract following German measles in the mother. Trans Ophthalmol Soc Aust 1941;3:35–46.
- Khandekar R, Al Awaidy S, Ganesh A, Bawikar S. An epidemiological and clinical study of ocular manifestations of congenital rubella syndrome in Omani children. Archives of Ophthalmology 2004;122(4):541–5.
- O’Neill J. The ocular manifestations of congenital infection: a study of the early effect and long-term outcome of maternally transmitted rubella and toxoplasmosis. Tr Am Ophth Soc 1998;XCVI:813–77.
- Blair N, Brockhurst R, Lee W. Central Serous Choroidopathy in the Hallermann-Streiff Syndrome. Annals of Ophthalmology 1981;13(8):987–90.
- Aydin A, Cakir A, Unal MH, Ersanli D. Central serous retinal detachment following glaucoma filtration surgery. Journal français d’ophtalmologie 2012;35(7):529.e1–5.