West Coast Retina
Case of the Month
Feb, 2016
Presented by Kevin Patel, MD
A 25 year-old Asian woman presenting with distorted vision in the left eye.

A
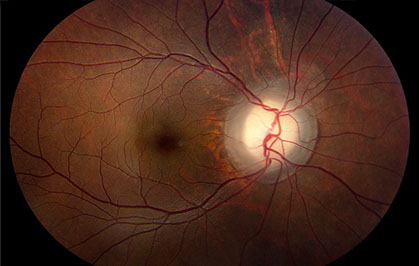
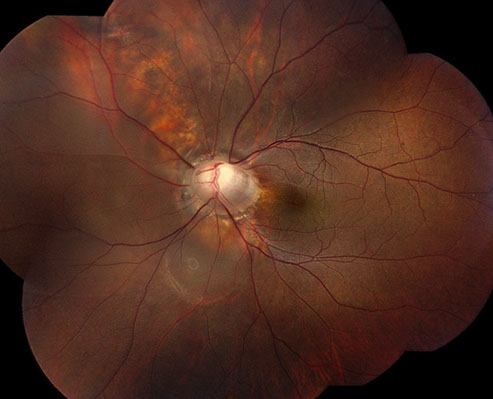
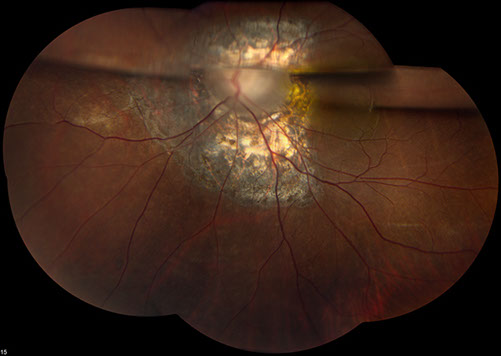
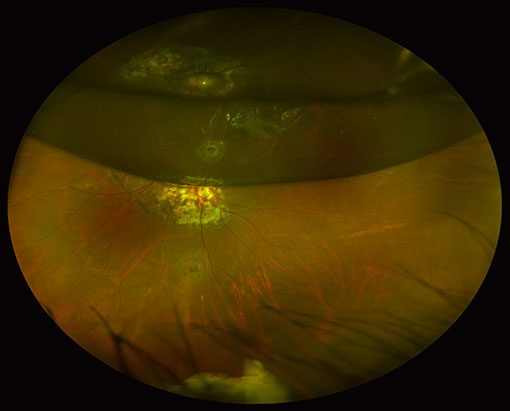
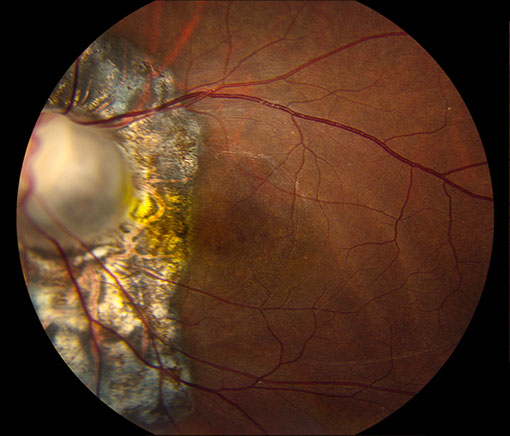
Figures 1A and B: Color fundus photographs of the right (A) and left (B) eyes. The posterior segment of the right eye has an optic nerve coloboma but an otherwise normal macula and peripheral retina (A). The left fundus has an optic nerve coloboma (B) with an associated retinal detachment extending from the optic nerve to the periphery from 8:00 to 10:30. There was also a localized area of detachment extending from the optic nerve inferiorly.
B
Case History:
A 25 year-old Asian woman presented with distorted vision in her left eye that began suddenly 2 weeks prior to presentation. The patient denied pain, flashes, floaters, or any other symptoms. Her past ocular and medical history were significant for sebaceous nevus syndrome with multiple epidermal nevi and lipodermoids. Family and social history were noncontributory.
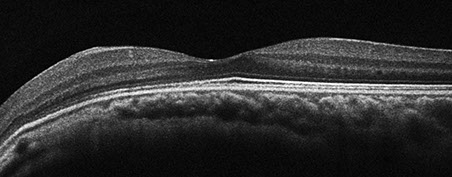
On examination, best-corrected visual acuity was 20/20 in the right eye and 20/25 in the left eye. Intraocular pressure and anterior segment examination were normal in both eyes except for a dermoid on the superotemporal sclera in the left eye. Posterior segment examination of the right eye was significant for an optic nerve coloboma, but the macula and remainder of the retina were otherwise normal (Figures 1A). The left eye also had an optic nerve coloboma (Figure 1B) with an associated retinal detachment extending from the optic nerve to the periphery from 8:00 to 10:30. There was also a localized area of detachment extending from the optic nerve inferiorly. Optical coherence tomography (OCT) of the macula was normal bilaterally (Figures 2A and B). A decision to perform vitrectomy surgery for repair of the optic nerve-associated retinal detachment was made. Vitrectomy with endolaser to the nasal peripapillary region and gas-fluid exchange (20% C3F8) was performed. The retina was attached on post-operative day 1 and remained attached for approximately 3 weeks.

A
B
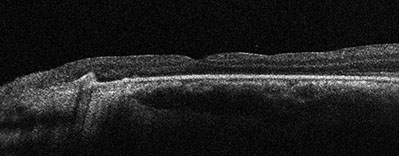
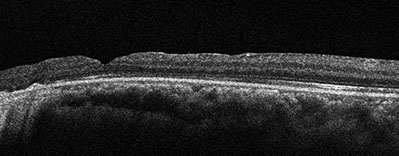
Figures 2A and B: Spectral domain OCT of the right (A) and left (B) eyes. No serous macula detachment or intraretinal edema is present. Thinning of the nerve fiber layer is noted.
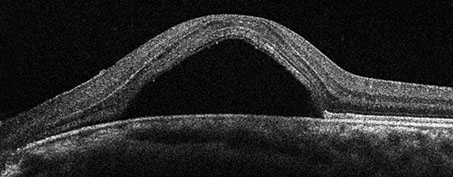
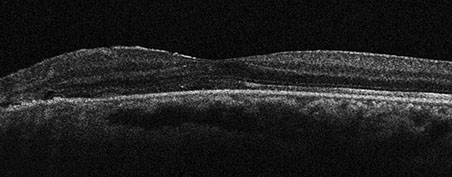
Figure 3: Optical coherence tomography of the left eye at 1 month postoperatively. Note the macular detachment.
Figure 4: Optical coherence tomography of the left eye at 5 days post supplemental peripapillary laser treatment. The fovea has reattached.
Case History (Continued)
Three weeks after surgery, the patient developed a bullous inferonasal retinal detachment extending from 6:00 to 9:30. Because she still had a large gas bubble left, she was positioned on her left side for one day in hopes of reattaching the nasal retina. The next day, she was attached inferonasally and the subretinal fluid had shifted temporally, from 3:00 to 7:30. No retinal break was noted. Peripheral laser was placed nasally, and she was instructed to maintain left-side positioning. She was attached several days after, however, 6 days after her supplemental laser treatment was given, she developed a macular detachment with subretinal fluid under her fovea (Figure 3). Her best-corrected visual acuity was 20/80 at this point. It was determined that the most likely source of the subretinal fluid was the temporal area of the coloboma, so additional laser was applied to the temporal peripapillary region. The patient was then told to position face down with her remaining 50% gas bubble. She was seen 5 days after. Her fovea was attached (Figure 4) and her best-corrected visual acuity was 20/50. However, she still had a peripheral detachment from 5:00 to 9:00. Her positioning was changed to a split time between prone and on her left side. On 2-day follow-up, there was a recurrence of the macular detachment with foveal subretinal and intraretinal fluid (Figure 5) and persistent peripheral detachment from 5:00 to 9:00. Best-corrected visual acuity decreased to 20/80. It was decided to perform additional laser to the temporal peripapillary region that day in clinic and repeat vitrectomy surgery the following day.
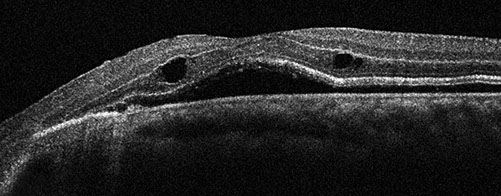
Figure 5: Optical coherence tomography of the left eye at 7 days post supplemental peripapillary laser treatment. There is a recurrence of macular detachment with foveal subretinal and intraretinal fluid.
A

B
Figures 6A and B: Color fundus photograph (A) and optical coherence tomography (B) of the left eye at 3 weeks after the second vitrectomy surgery. There is a recurrence of macular detachment with foveal subretinal and intraretinal fluid (A and B).
Case History (Continued)
Vitrectomy with endolaser photocoagulation and gas-fluid exchange (20% C3F8) was performed. The patient’s retina remained attached for 3 weeks. At this point, she again developed a macular detachment with foveal subretinal and intraretinal fluid (Figures 6A and B). Her best-corrected visual acuity decreased to 20/125. The decision for repeat vitrectomy surgery with Tisseel fibrin sealant application to the optic nerve coloboma was made. For this third vitrectomy, air-fluid exchange was done with meticulous drying of the optic nerve coloboma. Additional laser was applied to the temporal peripapillary area. Tisseel fibrin sealant was then slowly applied to fill the dried optic nerve coloboma. After the sealant clotted over the nerve, the air was exchanged with 20% C3F8 gas. Postoperatively, the patient was kept on her back for about 2 hours and then was instructed to remain face down afterwards.
The retina was attached 2 weeks after surgery, and the Tisseel clot had separated from the nerve and fallen inferiorly (Figure 7A). The macula was attached with no evidence of subretinal fluid on OCT. However, there was retinal thinning, likely secondary to peripapillary laser treatment (Figure 7B). On most recent follow-up, which was around 6 weeks postoperatively, the patient’s retina and macula remained attached (Figures 8A and B) with a best-corrected visual acuity of 20/80.
A
B
Figures 7A and B: Optos color fundus photograph (A) and optical coherence tomography (B) of the left eye at 2 weeks after the third vitrectomy surgery. The retina is attached and the Tisseel clot has separated from the nerve and fallen inferiorly (A). The macula is attached with no subretinal fluid. However, there is retinal thinning, likely secondary to peripapillary laser treatment (B).
Figures 8A – B: Color fundus photograph (A) and optical coherence tomography (B) of the left eye at 6 weeks after the third vitrectomy surgery. The retina and macula are attached (A and B).
What is your Diagnosis?
Differential Diagnosis:
The differential diagnosis of optic nerve-associated macular detachment and subretinal fluid includes the serous maculopathy associated with any of the congenital cavitary optic disc anomalies, such as optic pits, optic nerve colobomas, and morning glory anomalies.1 Macular schisis and detachments can also occur in eyes with enlarged optic nerve head cups from progressive glaucomatous damage.2 The diagnosis in our case of optic nerve coloboma with associated retinal detachment was quite clear from the patient’s initial exam.
Discussion:
Several congenital cavitary anomalies of the optic disc, including optic pits, optic nerve colobomas, and morning glory anomaly, can have an associated serous maculopathy. While these optic nerve anomalies are often described as distinct conditions, they likely fall within a clinical spectrum, with similar embryogenesis.1 The pathogenesis of the maculopathy seen in these optic disc anomalies is still poorly understood, leading to various treatment options with variable efficacy.
Typical colobomas of the optic nerve are congenital excavations located inferonasally in the disc. They are usually unilateral and visual field loss is only confined to the area of the defect. Affected eyes are otherwise normal. Optic nerve colobomas can be associated with a localized serous maculopathy. More extensive rhegmatogenous retinal detachments may occur in eyes with large associated chorioretinal colobomas.1 Our patient’s presentation falls within the spectrum between an atypical optic nerve coloboma and a morning glory anomaly. Morning glory disc anomaly is a unilateral markedly enlarged optic papilla with excavation involving the optic disc and peripapillary retina. Affected eyes typically have poor vision. Unique characteristics include radial arrangement of retinal vessels from the disc, glial hyperplasia over the center of the disc, elevated rim of peripapillary pigmented tissue, and traction on adjacent retina.3
Our patient also had a known diagnosis of a sebaceous nevus syndrome; however, the subtype was not known. Sebaceous nevus syndromes, also known as epidermal nevus syndromes, are a group of distinct disorders. Schimmelpenning syndrome is the best known of these syndromes. This condition appears to be sporadic rather than inherited. The major features of Schimmelpenning syndrome include sebaceous nevi of the head and neck, ocular choristomas or lid colobomas, cerebral defects causing seizures or mental retardation, skeletal abnormalities like scoliosis or vitamin D-resistant hypophosphatemic rickets, and cardiovascular abnormalities such as ventricular septal defects or co-arctation of the aorta.4 There is no published literature on the association of optic nerve colobomas with sebaceous nevus syndromes. Our patient had both of these conditions, so perhaps optic nerve colobomas can be seen less commonly as part of these syndromes and not yet described.
Serous maculopathy occurs in over 50% of eyes with cavitary optic disc anomalies.1 Onset is usually in early adulthood, however, detachment can occur in early infancy or later in life.5, 6 The maculopathy usually develops in a 2-step process, with intraretinal fluid accumulation occurring initially. This fluid then may percolate into the subretinal space.7 Serous detachment is usually located in the posterior pole, but large atypical colobomas may cause more extensive detachments. If left untreated, serous maculopathy typically leads to poor visual outcomes.1
The exact pathogenesis of this serous maculopathy is not well understood. Anatomically, optic disc anomalies disrupt the normal organization of axons and connective tissues at the juncture where the optic nerve exits the globe. Because of this, it is possible that the vitreous, subretinal, subarachnoid, and orbital spaces are all variably interconnected through the tissues comprising the excavated optic disc anomalies. Given this anatomic disruption, the source of intraretinal and subretinal fluid is likely from the vitreous cavity or possibly the subarachnoid space.1 Keeping this in mind, a unifying theory of pathogenesis for the serous maculopathy in cavitary optic disc anomalies is that a scleral defect permits anomalous communications between intraocular and extraocular spaces. These communications enable fluctuations in the gradient between intraocular and intracranial pressures that direct the movement of fluid through the cavitation into and under the retina.1
Numerous treatment options have been used to treat the serous maculopathy associated with cavitary optic disc anomalies. These include pharmacologic therapy with oral acetazolamide or corticosteroids, optic nerve sheath fenestration, macular buckling, inner retinal fenestration, laser photocoagulation alone, and pars plana vitrectomy with or without laser photocoagulation and gas tamponade.1 Schatz and McDonald initially described the technique of treating optic pit associated retinal detachments with a combination of laser photocoagulation, pars plana vitrectomy, and intraocular air-fluid exchange. They successfully reattached 6 eyes by using this treatment modality.8 The treatment options we employed for our patient consistently consisted of pars plana vitrectomy with laser photocoagulation and gas tamponade. Laser photocoagulation causes a juxtapapillary chorioretinal scar which functions as a barrier to fluid migration from the excavated optic nerve. Vitrectomy allows the placement of a large vitreous cavity gas bubble, which will dry and compress the retinal layers in the juxtapapillary area. This will facilitate the formation a more effective juxtapapillary laser photocoagulation scar during about a week of postoperative face-down positioning. The use of perfluorocarbon liquid or silicone oil is avoided secondary to the risk of subretinal or intracranial migration.1
While the aforementioned technique is widely accepted as the most effective treatment option, our patient failed vitrectomy with laser photocoagulation and gas tamponade on 2 consecutive occasions. As a result, we applied Tisseel fibrin sealant to the optic nerve coloboma during the third vitrectomy surgery. In a case series of 3 patients by Al Sabti et al, Tisseel fibrin sealant was applied during vitrectomy surgery to optic pits associated with macular detachment.9 The sealant was applied after meticulous drying of the optic pit was achieved during air-fluid exchange. Gas tamponade was then performed along with postoperative face-down positioning. All 3 patients had successful resolution of their macular detachments. The hypothesis of how the Tisseel fibrin sealant works is by first having a solid sheet of fibrin tamponade the pit intraoperatively, and then by stimulating a wound-healing process (gliosis) over the pit postopertively.
After this procedure was performed in our patient, she has remained attached with no evidence of macular subretinal fluid at her most recent follow-up visit, which was 6 weeks postoperatively. It should be noted that the surgeon in this case (HRM) does not believe that the Tisseel fibrin sealant played a role in the reattachment of this patient’s retina, as he believed that the additional extensive peripapillary laser photocoagulation was responsible.
Take Home Points
- Congential cavitary anomalies of the optic disc, including optic nerve colobomas, optic pits, and morning glory anomalies, may be associated with a serous maculopathy.
- The precise pathogenesis of the serous maculopathy seen in these optic disc anomalies is still unknown.
- There are numerous treatment options for this condition; the most widely accepted method involves pars plana vitrectomy with laser photocoagulation and gas tamponade.
Want to Subscribe to Case of the Month?
References:
- Jain N, Johnson MW. Pathogenesis and treatment of maculopathy associated with cavitary optic disc anomalies. Am J Ophthalmol. 2014;158:423-35.
- Zumbro DS, Jampol LM, Folk JC, et al. Macular schisis and detachment associated with presumed acquired enlarged optic nerve head cups. Am J Ophthalmol. 2007;144:70-4.
- Irvine AR, Crawford JB, Sullivan JH. The pathogenesis of retinal detachment with morning glory disc and optic pit. Trans Am Ophthalmol Soc. 1986;84:280-92.
- Happle R. The group of epidermal nevus syndromes Part I. Well defined phenotypes. J Am Acad Dermatol. 2010;63:1-22.
- Brown GC, Shields JA, Goldberg RE. Congenital pits of the optic nerve head. II. Clinical studies in humans. Opthalmology. 1980;87:51-65.
- Sugar HS. Congenital pits in the optic disc and their equivalents (congential colobomas and colobomalike excavations) associated with submacular fluid. Am J Ophthalmol. 1967;63:298-307.
- Imamura Y, Zweifel SA, Fujiwara T, et al. High-resolution optical coherence tomography findings in optic pit maculopathy. Retina. 2010;30:1104-12.
- Schatz H, McDonald HR. Treatment of sensory retinal detachment associated with optic nerve pit or coloboma. Ophthalmology. 1988;95:178-86.
- Al Sabti, K, Kumar N, Chow DR, et al. Management of optic disk pit-associated macular detachment with tisseel fibrin sealant. Retin Cases Brief Rep. 2008;2:274-7.