West Coast Retina
Case of the Month
January, 2010
Presented by Evelyn Fu, MD
A 22-year-old man with sudden decrease in vision in his left eye
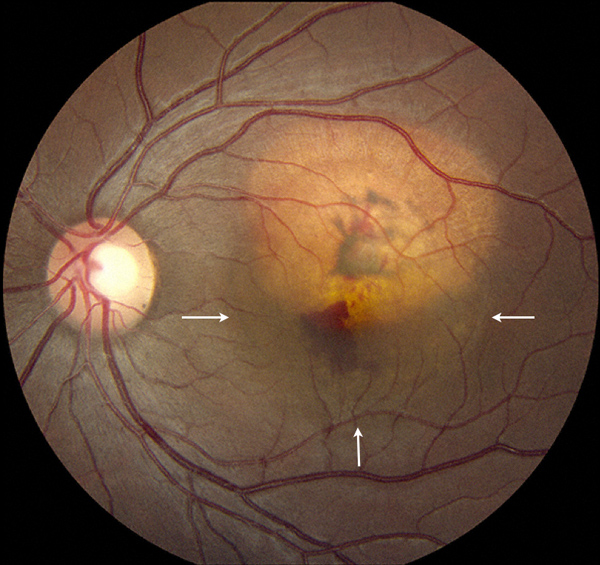
Figure 1: The fundus photograph of the left eye reveals a yellowish choroidal lesion. Note the subretinal hemorrhage and sensory retinal detachment (arrows).
Case History
A 22-year-old Hispanic man presented with a sudden decrease in vision in the left eye for one week. His past ocular and medical history is non-contributory.
On examination, his best-corrected visual acuity (BCVA) was 20/20 in the right eye and 20/50 in the left eye. The intraocular pressure and anterior segment examination were normal in each eye. The right fundus was normal. In the left macula, there was a slightly elevated, ovoid, yellowish subretinal mass 4mm x 3mm in size with clear margins (Figure 1). Overlying the lesion, there was retinal pigment epithelial clumping, deep retinal and sub-retinal hemorrhage, a grayish-green membrane, and a shallow sensory detachment of the macula.
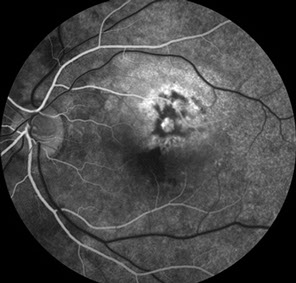
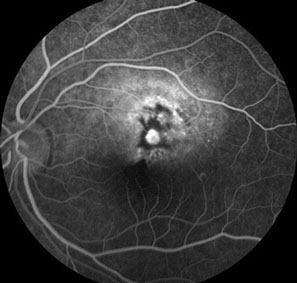
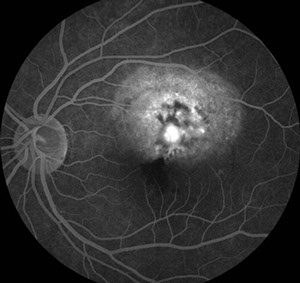
Fluorescein angiography (FA) demonstrated patchy early hyperfluorescence with staining of the elevated subretinal mass. In the center of the mass, there was an area of lacy hyperfluorescence with mild leakage. There was also pooling of fluorescein corresponding to the area of a sensory detachment (Figure 2A-C). B-Scan ultrasonography showed a slightly elevated, highly echo-reflective lesion with acoustic shadowing of the structures posterior to the mass (Figure 3).
A
B
C
Figures 2A-C: The fluorescein angiogram of the left eye reveals irregular early hyperfluorescence (Fig. 2A) with increasing fluorescence centrally and some pooling of dye (Figs. 2B and C).
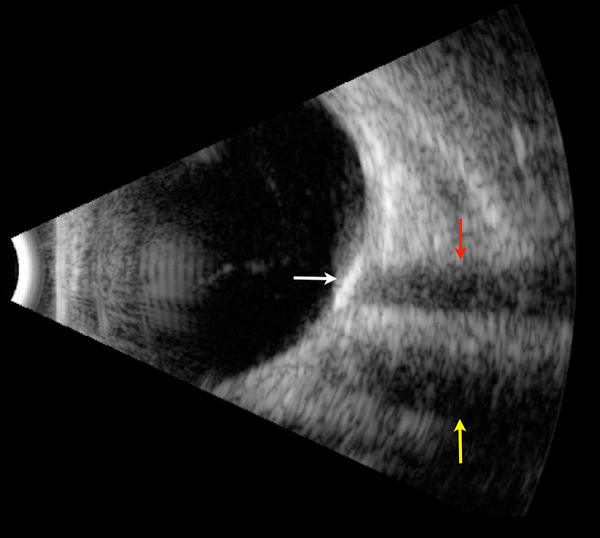
Figure 3: B-scan ultrasound shows a hyperreflective lesion (white arrow) with dense shadowing (red arrow). The other area decreased reflectivity is the shadow of the optic nerve (yellow arrow).
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis of an amelanotic subretinal lesion includes choroidal osteoma, choroidal hemangioma, amelanotic nevus or melanoma, metastasis, primary intraocular lymphoma, and posterior scleritis.
Choroidal osteoma is characteristically a yellow-white, oval lesion with distinct margins and varying degrees of overlying retinal pigment epithelial changes. Fluorescein angiography typically shows early patchy hyperfluorescence with late staining. Ultrasound evaluation is characteristic and shows high reflectivity with acoustic shadowing. In contrast, choroidal hemangioma is typically a reddish-orange mass with indistinct boarders and diffuse hyperfluorescence on fluorescein angiography. Amelanotic melanoma has low to medium internal reflectivity on A-scan. Choroidal metastasis usually are pale, white to yellow lesions with overlying serous detachment. The extent of serous leakage can often be quite extensive even for small lesions. Fluorescein angiography usually shows punctate areas of hyperfluorescence and significant leakage. Primary intraocular lymphoma, unlike choroidal osteoma, shows low internal reflectivity. Posterior scleritis is often associated with pain and shows thickened sclera with fluid in sub-Tenon's space on ultrasound.
Our patient was diagnosed with choroidal osteoma given the characteristic ultrasongraphic feature of acoustic shadowing. His case was complicated by the development of a choroidal neovascular (CNV) membrane.
Discussion
Choroidal osteoma was first reported by Gass and coworkers in 1978.1 It is usually unilateral and most commonly occurs in healthy young females in their second to third decade. It is most common in the juxtapapillary or peripapillary area but may extend into the macula. The basal diameter may range from 2—22mm but the tumors are usually flat or minimally elevated, less than 2.5mm in height. These lesions are composed of mature bone in various stages of calcification. Histopathologically, the choroid is replaced by a plaque-like bony mass.
About 40% of choroidal osteomas enlarge in size. However, the rate of growth is very slow. Choroidal neovascularization is the most significant complication and occurs in about 50% of cases by ten years.2 Laser photocoagulation, photodynamic therapy, and anti-angiogenic agents have been used to treat this complication. Choroidal osteoma itself is untreatable, though decalcification can occur following laser treatment or photodynamic therapy.
Take Home Points
- Choroidal osteoma is typically a yellow-white, oval lesion with distinct margins and varying degrees of overlying retinal pigment epithelial changes
- FA shows early patchy early hyperfluorescence with late staining.
- A highly reflective lesion with acoustic shadowing on ultrasonography is diagnostic.
- Choroidal neovascularization is the most significant complication and can be treated with laser photocoagulation, photodynamic therapy, and anti-angiogenic agents.
Want to Subscribe to Case of the Month?
References
- Gass JDM, Guerry RK, Jack RL, Harris G. Choroidal osteoma. Arch Ophthalmol 1978;96:428-35.
- Shields CL, Shields JA, Augsburger JJ : Choroidal osteoma. Surv Ophthalmol 1988;33:17-27.