West Coast Retina
Case of the Month
January, 2013
Presented by Paul Stewart, MD
A 48-year-old woman referred for evaluation of a lesion in her left eye

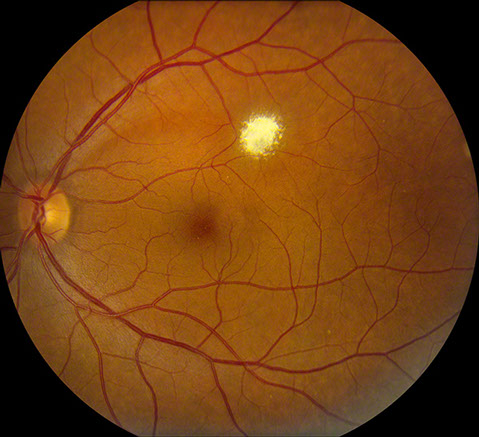
Figure 1: Color fundus photo of the left eye showing discrete, superficial yellow-white lesion with scalloped borders superotemporal to the fovea. No intrinsic vascularity is apparent.
Case History
A 48 year-old woman was referred for evaluation of a left eye fundus lesion that had first been noted two years earlier. She had no ocular complaints. Her past ocular history was significant for narrow angles treated with peripheral iridectomies without complication. She had no significant past medical or family history.
The patient’s vision was 20/13 and 20/16. Her intraocular pressures were 15mm Hg in both eyes. Her anterior segment examination was normal in both eyes. The dilated fundus examination of the right eye was normal. The left fundus exam showed clear ocular media and there was a healthy optic nerve. Within the superior macula there was a yellow-white lesion less than one disc diameter in size (Figure 1). There were no feeding or draining vessels and there did not appear to be any intrinsic vascularity. An arcuate nerve fiber layer defect corresponded with the location of the lesion.
Optical coherence tomography showed distortion of the normal retinal architecture with hyper-reflective granular material that appeared to spare the underlying RPE and Bruch’s membrane (Figure 2).
Fundus autofluorescence showed mild hyperautofluorescence with a small nidus of hypoautofluorescence at the inferior aspect of the lesion (Figure 3).
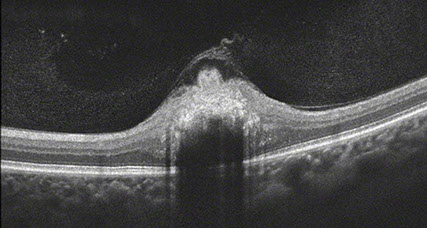
Figure 2: OCT-SD shows replacement of normal retinal layers with hyperreflective granular material that appeared to involve the superficial layers and spared the underlying RPE and Bruch’s membrane.
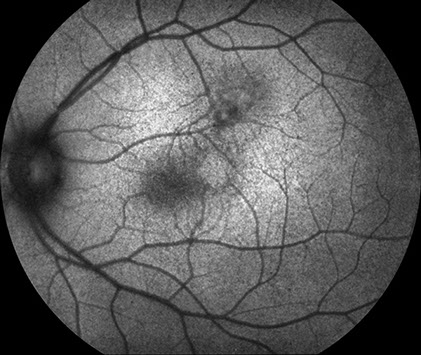

Figure 3: Fundus autofluorescence shows that the lesion has areas of mild increased and decreased autofluorescence.
Figure 4: Humphrey visual field demonstrating a scotoma inferotemporal to fixation corresponding to the lesion.
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis of a well-circumscribed yellow-white lesion of the retina includes retinal astrocytic hamartoma, acquired retinal astrocytoma, retinoblastoma, retinocytoma, myelinated retinal nerve fibers, granuloma, reactive gliosis, unifocal helioid choroiditis (solitary idiopathic choroiditis) and presumed solitary circumscribed retinal astrocytic proliferation.
Clinical Course
The lesion has remained unchanged on follow-up for more than one year. Humphrey visual field testing was performed and showed a scotoma corresponding to the lesion (Figure 4).
Discussion
Presumed solitary circumscribed retinal astrocytic proliferation (PSCRAP) is a recently described entity that occurs in middle-age to older patients with a small, solitary and defined lesion.1 The lesion is opaque and is confined to the retina. It is not associated with subretinal fluid, exudation or a feeder vessel. Our case exhibits all of these characteristics. The majority of the cases presented by the Shields were unchanged on follow-up, similar to our patient who was unchanged two years after presentation.
The differential diagnosis includes a retinal astrocytic hamartoma, which is typically diagnosed early in life and often associated with tuberous sclerosis. In these instances, the lesions are often multiple or bilateral. They tend to be located in the peripapillary region and can be translucent.2 Our patient did not have any of the stigmata of tuberous sclerosis. The margin of the lesion in retinal astocytic hamartomas is often less distinct than what is found with PSCRAP.
Acquired retinal astrocytomas tend to be progressive and may be associated with exudation or exudative retinal detachment.3 These lesions may correspond to astrocytomas of the CNS. Our patient’s lesion has been stable without change and lacks any exudation.
In a recent large series looking at retinocytomas, sometimes called spontaneously regressed retinoblastoma, the phenotype was described to include gray translucent tumors, intralesional calcification, RPE alterations and intralesional cysts.4 Our lesion is smaller than what is typically seen with a retinocytoma and does not have the characteristic features of that lesion.
Unifocal helioid choroiditis, also known as solitary idiopathic choroiditis, is another entity that presents with a yellow-white circumscribed lesion in the posterior pole.5,6 There is an active phase with overlying neurosensory detachment, which occasionally will have vitreous cell. In the inactive phase there is a discrete yellow-white choroidal lesion. Our case differs because of its location within the retina, rather than the choroid.
In summary, our patient has a presumed solitary circumscribed astrocytic proliferation. This lesion is a well-circumscribed, opaque intraretinal lesion without exudation or feeding vessels that should remain stable on follow-up. It differs from other white or yellow-white lesions of the retina in important ways that enable the clinician to appropriately reassure the patient as to its benign prognosis.
Take Home Points
- PSCRAP is a well-circumscribed, opaque lesion arising within the retina.
- This is a benign lesion, not known to cause visual loss.
Want to Subscribe to Case of the Month?
References
- Shields JA, Bianciotto CG, Kivela T. Presumed solitary circumscribed retinal astrocytic proliferation. Arch Ophthalmol. 2011. 129: 1189-1194.
- Kimoto K, Kishi D, Kono H, et al. Diagnosis of an isolated retinal astrocytic hamartoma aided by optical coherence tomography. Acta Ophthalmol. 2008. 86: 921-922.
- Vilaplana D, Castilla M, Poposki V, et al. Acquired retinal astrocytoma managed with endoresection. Retina. 2006. 26: 1081-1082.
- Abouzeid H, Balmer A, Moulin A, et al. Phenotypic variability of retinocytomas: preregression and postregression growth patterns. Br J Ophthalmol. 2012. 96: 884-889.
- Hong PH, Jampol LM, Dodwell DG, et al. Unifocal helioid chroidtitis. Arch Ophthalmol. 1997. 115: 1007-1013.
- Shields JA, Shields CL, Demirci H, et al. Solitary idiopathic choroiditis. Arch Ophthalmol. 2002. 120: 311-319.