West Coast Retina
Case of the Month
Jan, 2014
Presented by Ken Downes, MD
A 54 year-old man with asymptomatic retinal hemorrhages found on routine exam.

A

B
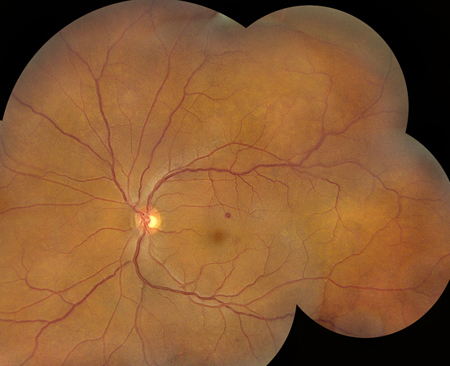
Figures 1A and B: Color fundus photograph of right and left macula and nerve. Note the scattered retinal hemorrhages in each eye, some with white centers. Mild retinal vascular tortuosity is present

A
B
Figures 2A and B: Color montage photographs of both eyes show retinal hemorrhages bilaterally, though more numerous in the right eye
Case History
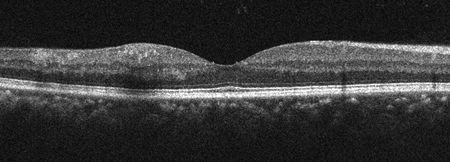
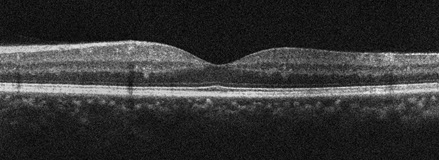
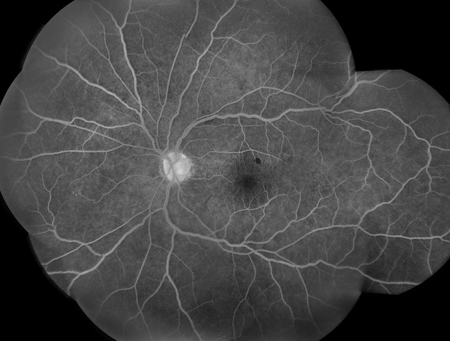
A 53-year-old asymptomatic man presented for routine eye exam. Past medical history was notable for sleep apnea and asthma. On presentation, visual acuity was 20/20 in both eyes. Intraocular pressure was 9 and 12 mmHg respectively and blood pressure was 158/86. Anterior segment examination was normal in both eyes except for mild lens changes. Posterior segment examination showed macular hemorrhages in both eyes as well as some white centered hemorrhages (Figures 1 and 2). Spectral-Domain Optical Coherence Tomography (SD-OCT) was performed showing intraretinal heme in the inner layers of the retina (Figure 3). Fluorescein angiography (FA) was performed and showed areas of blocking corresponding to the intraretinal hemorrhages and was otherwise unremarkable (Figure 4).
A
B
Figure 3A and B: Spectral domain OCT of each eye showing intraretinal hemorrhages in the inner retinal layers of the macula of the right (A) and left (B) macula.

A
B
Figures 4A and B: Montaged fluorescein angiogram of right (A) and left (B) fundus. There are scattered areas of blockage corresponding to the areas of intraretinal heme. No vascular filling defects or other abnormalities were noted.
Clinical Course
The patient was lost to follow up for seven months and returned when he noticed a black spot in his right eye associated with visual distortion. Visual acuity was 20/63 in the right eye and 20/20 in the left eye. Intraocular pressure was 13 mmHg on the right and 11 mmHg on the left. Anterior segment examination was unchanged. Posterior segment examination showed more prominent white centered hemorrhages in the macula and in the periphery of both eyes as well as a hemorrhage in the fovea of the right eye (Figure 5 and 6). SD-OCT was performed and again showed intraretinal hemorrhages, involving the fovea of the right eye.

A

B
Figure 5A and B: Color fundus photograph of the right (A) and left (B) macula. Seven months later, multiple intraretinal hemorrhages (many with white centers) are present in both eyes.

A

B
Figure 6A and B: Color fundus photograph montages of the right (A) and left (B) eye. More prominent and numerous retinal hemorrhages are present, particularly in the left eye. Note that most of the hemorrhages have white centers.
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis for bilateral intraretinal hemorrhages, macular hemorrhages and white centered hemorrhages (Roth’s spots) includes diabetes mellitus, hypertension, bilateral vascular occlusion, radiation retinopathy, interferon treatment, severe anemia, severe thrombocytopenia, leukemia, bacterial endocarditis, HIV microangiopathy, and systemic dysproteinemias such as multiple myeloma.
Clinical Course
Lab testing, including complete blood count with differential, serum electrolytes, hepatic function panel, serum blood glucose, hemoglobin A1c, erythrocyte sedimentation rate, and C-Reactive protein, were ordered. All were normal except for a white blood cell count of 292,000, of which 74% were immature/blast cells. This finding is consistent with a diagnosis of Chronic Myelogenous Leukemia with excess blasts.
Discussion
Therapy for adult leukemia has evolved and improved resulting in significantly improved survival of these patients. This improvement in survival has led to an increase in variability of ocular presentation of disease. Leukemia may involve any ocular tissue by direct infiltration, ischemia, hemorrhage, or even chemotherapeutic agent toxicity. Ocular involvement may also be seen in graft-versus host disease in patients who have undergone bone marrow transplantation. Leukemia can manifest in the adnexa, conjunctiva, sclera, cornea, anterior chamber, iris, lens, vitreous, retina, choroid, and optic nerve. Recognition of the varied ocular presentations is important for the ophthalmologist to assess the course of the disease leukemia and also to detect relapses.1 (See table below taken from Sharma ,et al 2004)
The retinopathy appearing in patients with leukemia usually consists of tortuous retinal veins, hemorrhages (intra-retinal, white-centered hemorrhages), vascular sheathing, and cotton wool spots.2 Patients often do not report ocular symptoms associated with leukemic retinopathy. In several prospective studies, approximately 50% of patients diagnosed with acute leukemia had retinopathy had presentation.2,3 Intraretinal hemorrhage were the most frequent finding encountered with cotton wool spots seen rarely. 2,3 The correlation between the hematological parameters and retinal findings has been the subject of much debate and research, and there are wide variations in laboratory values of patients who have ocular findings and those who do not.
Across several studies, elevated white count (mean > 63,000 cells/ul ) was the most significantly associated lab abnormality with intraretinal hemorrhage, white centered hemorrhage and cotton wool spots.2,3,6 Thrombocytopenia (mean platelet count < 50,000 /ul) was also significantly associated with intraretinal hemorrhage in one study.6 Hemoglobin levels were not significantly associated with leukemic retinopathy findings.2,3,6
Retrospective studies suggest that leukemic retinopathy does not carry adverse prognostic significance, and a recent prospective study showed no difference in the remission rate in those with and without retinopathy.4,5,6 Leukemic retinopathy resolves with treatment of the underlying disease. Prompt recognition of the ocular signs of leukemia is crucial to expedite diagnosis in asymptomatic patients and monitor for recurrence of disease.
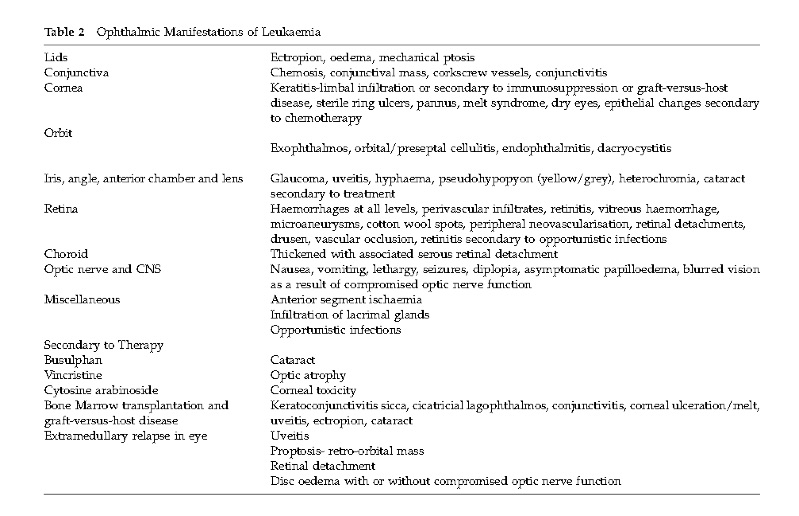
From Sharma ,et al 2004)
Take Home Points
- Recognition of the varied ocular presentations is important in assessing the course and recurrence of disease in leukemic patients
- Clinical features of leukemic retinopathy include tortuous retinal veins, hemorrhages (intra-retinal, white-centered hemorrhages), vascular sheathing, and cotton wool spots
- Retinopathy does not indicate a worse prognosis in patients with leukemia
- Leukocytosis and thrombocytopenia are associated with the presence of retinopathy in patients with leukemia
Want to Subscribe to Case of the Month?
References
- T Sharma, J Grewal, S Gupta and PI Murray. Ophthalmic manifestations of acute leukaemias: the ophthalmologist’s role. Eye (2004) 18, 663–672
- Jackson, Reddy et al. Retinal findings in adult leukaemia: correlation with leukocytosis. Clin. Lab. Haem. 1996, 18, 105–109
- S. C. Reddy and N. Jackson. Retinopathy in acute leukaemia at initial diagnosis: correlation of fundus lesions and haematological parameters. Acta Ophthalmologica Scandinavica 2004; 82: 81–85.
- Marshall R.A. (1959). A review of lesions in the optic fundus in various diseases of the blood. Blood 14, 882–891.
- Mahneke A. & Videbaek A. (1964). On changes in the optic fundus in leukemia. Acta Ophthalmologica (Copenhagen) 42, 201–210.
- Karesh J.W., Goldman E.J., Reck K., Kelman S.E., Lee E.J. & Schiffer C.A. (1989). A prospective ophthalmic evaluation of patients with acute myeloid leukemia: correlation of ocular and hematologic findings. Journal of Clinical Oncology 7, 1528–1532.