West Coast Retina
Case of the Month
July, 2013
A 79 year-old woman with difficulty reading small print
Presented by Sara Haug, MD, PhD


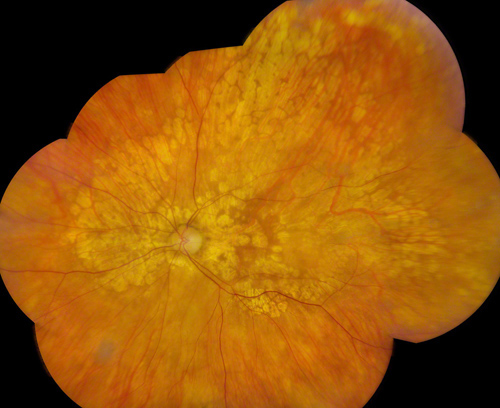
Figure 1: Color fundus photograph montage of the right eye. Peripapillary atrophy is present with extension of the pigment epithelial atrophy nasally, temporally, and superotemporally. There is geographic atrophy present in the macula, however the fovea appears to be spared.
Figure 2: Color fundus photograph montage of the left eye. Well-circumscribed atrophy of the retinal pigment epithelium is observed around the optic nerve and in the nasal, superior, and temporal quadrants. There is geographic atrophy in the macula.
Case History
A 79 year-old woman with a medical history significant for cardiac bypass surgery presents with nyctalopia and difficulty reading. She reports the symptoms have been getting progressively worse over the past six months. Aside from uncomplicated cataract surgery performed five years prior to presentation, the patient has no significant ocular history.
Vision in the right eye was 20/40 and in the left eye was 20/50. Intraocular pressures were 13 and 12 respectively. Anterior segment examination was unremarkable. A posterior chamber intraocular lenses was present in each eye. Fundus examination on the right revealed well-circumscribed areas of pigment epithelial atrophy around the optic nerve extending into the nasal and superotemporal periphery. The larger choroidal vessels were visible in the areas of atrophy. Geographic atrophy of the pigment epithelium was present in the macula, with sparing of the fovea (Figure 1). Similarly, in the left eye there was peripapillary atrophy with pigment epithelial atrophy in the nasal, superior, and temporal quadrants. There was also marked atrophy in the left macula with sparing of the fovea (Figure 2).
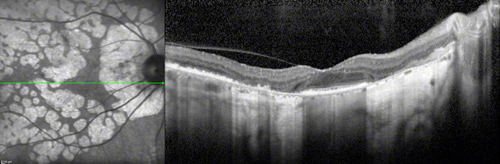
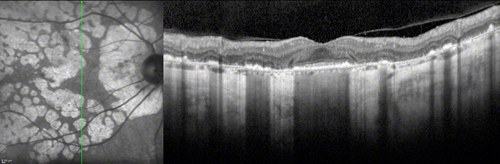
Spectral Domain-OCT images revealed loss of the outer retinal photoreceptor layers and retinal pigment epithelium in the areas of atrophy seen on fundus examination, sparing the foveal region in both eyes with a markedly attenuated choroid. (Figures 3 & 4) Fundus autofluorescence showed placoid hypofluorescent lesions due to retinal pigment epithelial atrophy. The involved areas of retinal pigment epithelial loss on fundus autofluorescence imaging appeared more widespread than was evident on color fundus photographs. The fovea appeared intact in both eyes. (Figures 5 & 6)
A
B
Figures 3A and B: Spectral Domain-OCT of the right eye. (A) Horizontal scan through the fovea shows relative preservation of retinal architecture at the fovea with loss of the photoreceptor and pigment epithelial layers in areas of atrophy and adjacent to the optic disc. (B) Vertical scan through the fovea, highlighting the loss of outer retinal layers including the retinal pigment epithelium in areas of atrophy. The choroid is markedly thinned throughout and there is increased reflectivity of the choroid and deeper sclera in the areas where the normally reflective retinal pigment epithelium is absent.
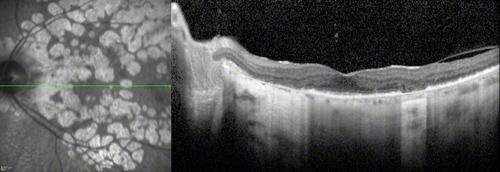
Figure 4: Spectral Domain-OCT of the left eye. Horizontal scan through the fovea reveals a relatively normal foveal depression but severe loss of the outer retinal layers, including the pigment epithelium and photoreceptors in the peripapillary region and the atrophic area just temporal to the fovea. The choroid is markedly thinned and relatively avascular. There is increased signal into the choroid and sclera in areas of atrophy.
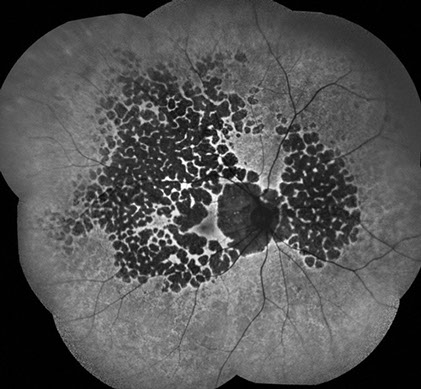
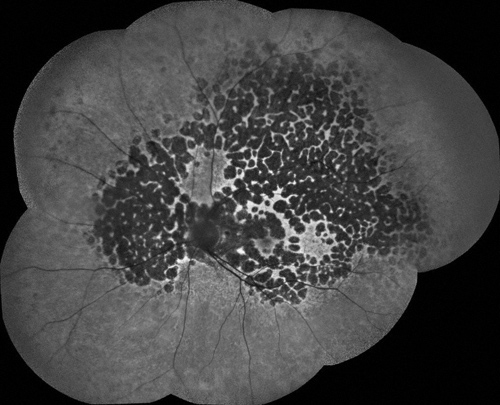
Figure 5: Fundus autofluorescence montage of the right eye reveals multiple, well circumscribed, hypofluorescent, placoid lesions throughout the fundus. Within some of the hypofluorescent lesions, small white lines representing choroidal vasculature can be identified.
Figure 6: Fundus autofluorescence montage of the left eye. There are hypofluorescent regions around the optic nerve and throughout the fundus. The fovea appears intact.
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis for atrophy of the pigment epithelium includes macular degeneration and pathologic myopia. Gyrate atrophy, retinitis pigmentosa, rod-cone dystrophies and choroidal sclerosis must also be considered. It is also possible the patient is a choroideremia carrier.
Our patient did not have a long axial length or classic drusen. Atypical macular degeneration certainly is a consideration, but given the symmetry between the two eyes and the extensive areas of atrophy is less likely. Ornithine levels were within normal limits. Electroretinography testing confirmed rod and cone dysfunction, but was not consistent with retinitis pigmentosa given the patient’s age. The funduscopic appearance of well-circumscribed and confluent chorioretinal atrophic lesions that extend beyond the macula is part of the phenotypic description for choroidal sclerosis, which is our patient’s diagnosis.
Discussion
Choroidal sclerosis is a group of retinal dystrophies that share a common phenotypic fundus appearance – scalloped, well circumscribed, and confluent chorioretinal atrophic lesions that are peripapillary, macular, and peripheral. Choroidal sclerosis was first described by Arnold Sorsby in 1935 as a bilateral disorder with a circumscribed oval area extending from the disc to well beyond the macula, revealing varying degrees of atrophy of the choroidal vessels.1 Dr. Sorsby’s observation of white, sclerotic choroidal vessels visible through the atrophic lesions prompted him to name the disorder “choroidal sclerosis”.1,2 Histologic studies have since revealed the name of choroidal sclerosis to be a misnomer, given the primary pathology is the loss of choriocapillaris, retinal pigment epithelium, and outer retina with the absence of arteriosclerotic changes in the choroidal vasculature.3
Three forms of choroidal sclerosis have been identified based on the location of the lesions; central areolar, peripapillary, and diffuse choroidal atrophy.4 Current imaging techniques such as fundus autofluorescence (FAF) and SD-OCT not only aid in diagnosis of the disease, but are also important in monitoring for disease progression. Monitoring patients with fundus autofluorescence can be invaluable as small lesions not detected by indirect ophthalmoscopy may be easily identified with FAF, permitting more accurate determination of disease progression.4
A diagnosis of choroidal sclerosis does not negate the need for further work-up in patients with the classic fundus appearance. Rather, the choroidal sclerosis phenotype includes diagnoses such as gyrate atrophy, PRPH2/rds-associated retinal degeneration, and RLBP1-associated retinitis punctate albescens among others.4-6 Identification of the choroidal sclerosis funduscopic pattern can help to guide further work-up and genetic screening in patients.4,7
Take Home Points
- Choroidal sclerosis is a family of dystrophies, classified by well-circumscribed, scalloped, and confluent areas of retinal pigment epithelial atrophy.
- Conditions such as gyrate atropy, PRPH2/rds-associated retinal degeneration, and RLBP1-associated retinitis punctate albescens fall into this family of disorders
- Choroidal sclerosis is a progressive disease that can be closely monitored with SD-OCT and fundus autofluorescence imaging.
Want to Subscribe to Case of the Month?
References
- Sorsby A. Choroidal Sclerosis: (Section of Ophthalmology). Proc R Soc Med. 1935;28:526-8.
- Sorsby A and Davey JB. Generalized choroidal sclerosis: course and mode of inheritance. Br J Ophthalmol 1955;39:257-75.
- Ashton N. Central areolar choroidal sclerosis: a histo-pathological study. Br J Ophthalmol 1953;37:140-7.
- Hwang JC, Kim DY, Chou CL, Tsang SH. Fundus autofluorescence, optical coherence tomography, and electroretinogram findings in choroidal sclerosis. Retina 2010;30:1095-103.
- Boon CJ, den Hollander AI, Hoyng CB et al. The spectrum of retinal dystrophies caused by mutations in the peripherin/RDS gene. Prog Retin Eye Res 2008;27:213-35.
- Burstedt MS, Forsman-Semb K, Folovleva I et al. Ocular phenotype of bothria dystrophy, an autosomal recessive retinitis pigmentosa associated with an R234W mutation in the RLBP1 gene. Arch Ophthalmol 2001;119:260-7.
- Archer D, Krill AE, Newell FW. Fluorescein studies of choroidal sclerosis. Am J Ophthalmol 1971;71:266-85.