West Coast Retina
Case of the Month
June, 2010
Presented by Jon Wender, MD
A 22 year-old Hispanic female with 2 week history of decreased vision in her right eye.

Figures 1: Color photograph and montage of the right eye shows a gray-greenish lesion in the peripapillary area with an overlying epiretinal membrane and retinal folds at the temporal edge of the macula

Case History
A 22-year-old mildly obese Hispanic female presented with a 2-week history of decreased vision in her right eye. She also reported severe right-sided temporal and frontal headaches treated with hydrocodone for one month prior to presentation. Persistent headaches necessitated an emergency department visit where neurologic examination, lumbar puncture, and magnetic resonance imaging (MRI) of the brain were within normal limits. Her past ocular history was non-contributory. Ten months prior to presentation, she gave birth to a healthy full-term infant following an uncomplicated pregnancy.
Visual acuity was 2/200 in the right eye, and 20/20 in the left eye. The intraocular pressure was within normal limits in each eye and the blood pressure was 125/81 mm Hg. Anterior segment examination was normal bilaterally with no evidence of inflammation. The posterior segment examination of the right eye revealed an elevated gray-green mass involving the macula, peripapillary region, and nasal, superior, and inferior midperiphery (Figure 1). This lesion was associated with an epiretinal membrane, intrinsic retinal vascular tortuosity, and retinal folds at its temporal edge. The posterior segment examination of the left eye was normal.
Fluorescein angiography (FA) of the right eye revealed early hypofluorescence secondary to blockage by the hyperpigmented component of the lesion (Figure 2) as well as late hyperfluorescence, consistent with extensive retinal vascular leakage . Spectral domain optical coherence tomography (SD-OCT) of the right eye demonstrated an epiretinal membrane, retinal folds, extensive macular thickening, and cystoid macular edema (Figure 3).
Figures 2: Fluorescein angiography reveals early hyperfluorescence and significant vascular tortuosity within the lesion. Fluorescence increases rapidly revealing late leakage

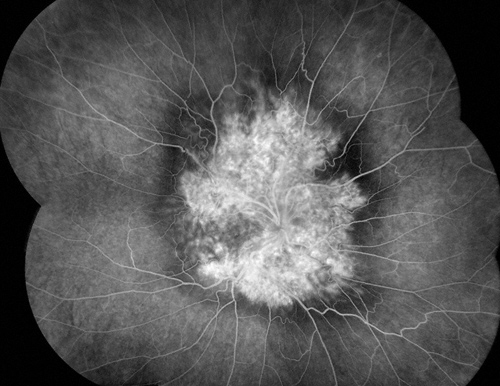
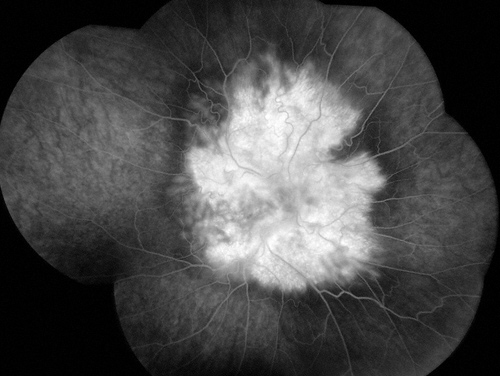
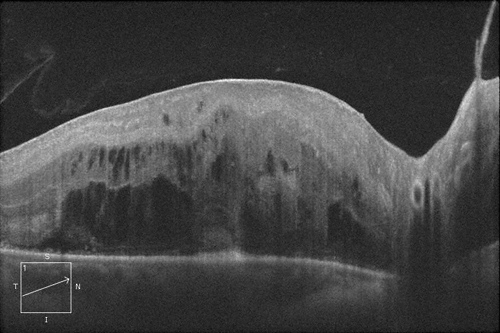
Figure 3: Spectral domain optical coherence tomography reveals significantly retinal thickening with intraretinal edema, and an epiretinal membrane.
What is your Diagnosis?
The examination as well as the FA and OCT1 findings were consistent with a diagnosis of Combined Hamartoma of the Retina and Retinal Pigment Epithelium (CHRRPE).
Discussion
Combined hamartoma of the retina and RPE, described by Gass in 1973,2 is a rare, typically unilateral, benign proliferation of the retina, RPE, retinal vessels, and vitreous. The age at diagnosis ranges from less than one month3 to the seventh decade.4 Common presenting symptoms are painless vision loss and strabismus, but others include floaters, leukocoria and, rarely, ocular pain.3, 4 Gender predilection is unclear, as some studies have revealed a male predominance,3, 5 while another large review demonstrated an equal distribution between men and women.4
Although some reports suggest that CHRRPE may be acquired, the majority of the evidence points to a developmental etiology. Indications that some cases may be acquired include a report of CHRRPE following an episode of papilledema6 as well as an association between CHRRPE and pathologic evidence of prior anterior segment trauma, as described by Spencer.2 The fact that the diagnosis is frequently made during infancy or childhood, however, is suggestive of a developmental etiology.3 Case reports of CHRRPE occurring in association with optic disc coloboma,4 optic nerve head drusen,4 optic disc pits,2 and X-linked retinoschisis2 also suggest a developmental origin.
Ticho and colleagues reported a case of CHRRPE that was diagnosed following an episode of meningoencephalitis.7 The presence of severe headaches in our patient at the time of diagnosis likewise prompted suspicion of associated intracranial pathology. Meningitis and encephalitis were ruled out, however, based on normal neurologic examination, cerebrospinal fluid analysis, and neuroimaging. Headache in this case was therefore presumed to be an incidental finding unrelated to the ocular pathology.
There are no reports, to our knowledge, of acute visual loss secondary to CHRRPE associated with pregnancy. Other types of hamartomas, however, including orbital hemangiomas, are known to enlarge during pregnancy.7 Blurred vision following pregnancy in this case may be incidental, or may suggest that CHRRPE can also enlarge or decompensate during pregnancy, resulting in the onset of symptoms during the postpartum period.
Visual loss due to CHRRPE results from a combination of factors including amblyopia, involvement of the lesion with the optic nerve or the macula, or tractional distortion of the macula by an associated epiretinal membrane (ERM).3, 4 Progressive visual decline, in some cases due to epiretinal membrane contraction, may also occur.4 Apparent enlargement over time of a CHRRPE may result in misdiagnosis as a malignant tumor,2 which, in some cases, has prompted unwarranted enucleation.
Published reports of visual outcomes after treatment of CHRRPE have provided conflicting results. McDonald and colleagues reported that surgery to remove the ERM component of CHRRPE in 2 patients (a 44-year-old woman and a 26-year-old man) resulted in decreased angiographic evidence of retinal vascular leakage, but did not improve visual acuity.8 Others have demonstrated, however, that removal of an ERM associated with CHRRPE may result in visual acuity improvement, particularly if patients are younger or if the hamartoma does not directly involve the macula.9,10 In such cases, peeling of an ERM may decrease distortion of the macula and thereby improve visual results.9 Amblyopia therapy may also improve visual outcomes if the lesion is diagnosed in infancy or childhood.4
Take Home Points
- Combined hamartoma of the retina and RPE is a rare, benign lesion associated with variable degrees of vision loss depending on whether the optic nerve or macula is involved.
- Patients with CHRRPE typically present during childhood but, in some cases, symptoms may not be noticed until later in adult life.
- Surgical intervention is inconsistent in achieving visual improvement but may be more likely to do so in younger patients as well as in cases in which the lesion does not involve the macula.
Want to Subscribe to Case of the Month?
References
- Shields CL, Mashayekhi A, Dai VV, et al. Optical coherence tomographic findings of combined hamartoma of the retina and retinal pigment epithelium in 11 patients. Arch Ophthalmol 2005;123(12):1746-50.
- Gass JD. An unusual hamartoma of the pigment epithelium and retina simulating choroidal melanoma and retinoblastoma. Trans Am Ophthalmol Soc 1973;71:171-83; discussions 84-5.
- Shields CL, Thangappan A, Hartzell K, et al. Combined hamartoma of the retina and retinal pigment epithelium in 77 consecutive patients visual outcome based on macular versus extramacular tumor location. Ophthalmology 2008;115(12):2246-52 e3.
- Schachat AP, Shields JA, Fine SL, et al. Combined hamartomas of the retina and retinal pigment epithelium. Ophthalmology 1984;91(12):1609-15.
- Font RL, Moura RA, Shetlar DJ, et al. Combined hamartoma of sensory retina and retinal pigment epithelium. Retina 1989;9(4):302-11.
- Hrisomalos NF, Mansour AM, Jampol LM, et al. "Pseudo'-combined hamartoma following papilledema. Case report. Arch Ophthalmol 1987;105(12):1634-5.
- Ticho BH, Egel RT, Jampol LM. Acquired combined hamartoma of the retina and pigment epithelium following parainfectious meningoencephalitis with optic neuritis. J Pediatr Ophthalmol Strabismus 1998;35(2):116-8.
- McDonald HR, Abrams GW, Burke JM, Neuwirth J. Clinicopathologic results of vitreous surgery for epiretinal membranes in patients with combined retinal and retinal pigment epithelial hamartomas. Am J Ophthalmol 1985;100(6):806-13.
- Zhang X, Dong F, Dai R, Yu W. Surgical management of epiretinal membrane in combined hamartomas of the retina and retinal pigment epithelium. Retina;30(2):305-9.
- Cohn AD, Quiram PA, Drenser KA, et al. Surgical outcomes of epiretinal membranes associated with combined hamartoma of the retina and retinal pigment epithelium. Retina 2009;29(6):825-30.