West Coast Retina
Case of the Month
June, 2015
Presented by Steven Williams, MD
A 52-year-old Indian woman presented with decreased vision in both eyes

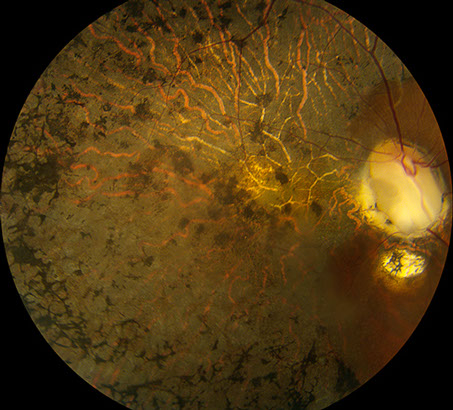
A
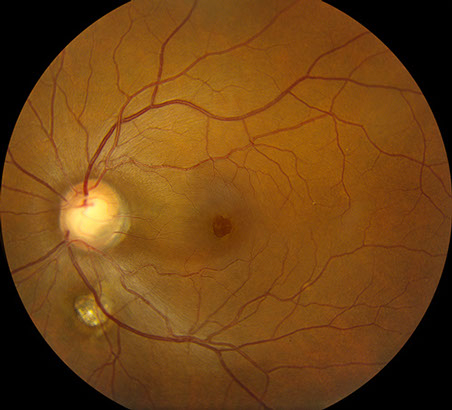
B
Figures 1A and B: Colors fundus photos of the right and left eye. Note the bilateral optic nerve pits and chorioretinal colobomas. The right eye (A) has extensive RPE disruption in the posterior pole from presumed chronic serous retinal detachment, which spontaneously resolved. There is serous detachment of the macula of the left eye (B). Note the false appearance of a full thickness macula hole.
Case History
A 52-year-old Indian woman presented with decreased vision in both eyes which had progressively worsened in the right eye for the last two years and in the left eye for the prior two months. Past ocular and medical histories were unremarkable. The patient had no history of renal disease or family history of ocular disease.
On examination, best-corrected visual acuity was 6/200 in the right eye and 20/63 in the left eye. Intraocular pressures were normal. Anterior segment examination was unremarkable, except for mild posterior subscapular cataract in the right eye. Posterior segment examination revealed bilateral colobomatous changes of the optic nerve, retina and choroid. There was diffuse pigment epithelial disruption and atrophy in the posteriorly pole and mid-periphery of the right eye (Figure 1A). The macula of the left eye demonstrated an area of retinoschisis extending from the disc, associated with foveal retinal detachment (Figure 1B). Spectral domain OCT demonstrated diffuse outer retinal atrophy and disorganization in the right eye and retinoschisis associated with subretinal fluid in the left eye (Figure 2). A clear connection between the optic disc cavitation and the retinoschisis cavity could also be seen (Figure 2B).
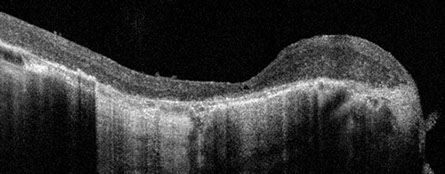
A
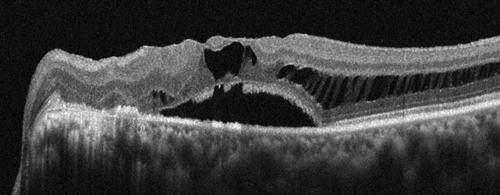
Figures 2A and B: SD-OCT of the right eye and left eye. There is gross thinning, outer retinal degeneration, and mild epiretinal membrane formation in the right eye (A). In the left eye, there is extensive retinoschisis that is associated with subretinal fluid at the fovea (B). The connection between the optic disc pit and the retinoschisis is clearly seen (arrow).
B
Differential Diagnosis
The differential diagnosis for optic nerve head anomalies associated with macula detachment includes congenital and acquired optic nerve pit, papillorenal syndrome, morning glory deformity, tilted disc syndrome, optic disc hypoplasia, juxtapapillary staphyloma, and pathologic myopia. Our patient had bilateral optic pits associated with chorioretinal colobomas and serous macula detachment of the left eye.
Discussion
Optic pit is a rare anomaly of the optic nerve head that can result from inadequate closure of the fetal ocular fissure. This anomaly can be associated with other ocular abnormalities including microphthalmos, optic nerve coloboma, lens coloboma, persistent fetal vasculature, orbital cyst and intracranial abnormalities. It is bilateral in 10-15% of cases and may follow an autosomal dominant inheritance pattern. Familial cases have been associated with PAX6 gene mutations on chromosome 11p13. The pit is usually located on the temporal aspect of the optic nerve, near the margin of the disc, and is often associated with an overlying gray membrane that frequently has holes within it. Histopathology shows that the optic pit contains dysplastic retina that extends through a defect in the lamina cribrosa into the subarachnoid space.
Optic pits usually present in young adults with decreased vision in the setting of serous detachment of the macula. The macula detachment often has a tear-drop configuration extending from the vicinity of the optic pit. Many patients develop a central, well-defined area of retinal detachment surrounded by a less well-defined area of retinoschisis. There is seldom a posterior vitreous detachment. Fluorescein angiography in early macula detachments may show no abnormalities in the early phases, while demonstrating late staining of the optic disc and rarely, dye leakage into the subretinal space. Patients with RPE changes from chronic macula detachment may show early hyperfluorescence in areas of depigmentation without evidence of abnormal retinal or choroidal permeability. The subretinal fluid is the product of vitreous fluid and in some cases, cerebrospinal fluid.
Optical coherence tomography may demonstrate a communication between the vitreous and/or subarachnoid space with the subretinal space and/or the intraretinal layers. OCT may also delineate the extent of subretinal fluid and schisis formation. Detachments often begin with progressive macular schisis, with fluid that extends through the external limiting membrane to cause subfoveal macular detachment and acute vision loss. Spontaneous reattachment is not uncommon, but may take several months to years. Prolonged detachment may lead to poorer visual outcomes. Long-term follow-up suggests that 50-75% of eyes will have visual acuity reduced to 20/100 or worse in 5-9 years.
Surgical treatment options include a combination of pars plana vitrectomy with intravitreal gas tamponade, peeling of the internal limiting membrane and photocoagulation across the neck of the detachment to close the communication to the subretinal or intraretinal space. No technique has proven superior and often multiple treatments are needed to achieve retinal reattachment. In most cases the submacular fluid can be displaced inferiorly by gas tamponade. Serous retinal detachment can recur months to years after treatment. Rarely, gas or silicone oil tamponade may migrate through the pit into the subarachnoid space.
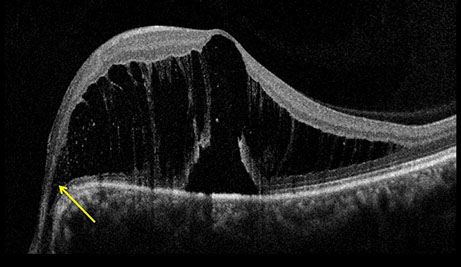
Our patient underwent vitrectomy with posterior hyaloid disinsertion, gas fluid exchange and papillomacular bundle laser, and prone positioning. Vision improved to 20/40. At 6 week follow up, the connection to the optic pit was eliminated and the nasal retinoschisis had resolved (Figures 3A and B). It may take months for the final attachment of the macula as the chronic subretinal fluid resolves.
B
Figures 3A and B: Fundus photograph and SD-OCT of the left eye 6 weeks following vitrectomy with posterior hyaloid disinsertion, gas-fluid exchange, papillomacular bundle laser, and prone positioning. Note the absence of retinoschisis in the papillomacular bundle. The macula detachment will resolve over time, as the direct communication with the optic pit has been eliminated.

A
Take Home Points
- Optic nerve pit is an uncommon optic nerve anomaly that can be associated with serous retinal detachment.
- Although serous retinal detachment may resolve spontaneously, pars plana vitrectomy surgery with gas tamponade and laser is necessary for better visual outcomes.
Want to Subscribe to Case of the Month?
References
- Agarwal A. Gass’ Atlas of Macula Diseases, 5th Ed. Elsevier; 2012. Pg. 1256-68.
- Brown, GC, Shields JA, Patty, BE. Congenital pits of the optic nerve head. ll. Clinical studies in humans. Ophthalmology 1980;87:51-65.
- Sobol WM, Blodi CF, Folk JC, et al. Long-term outcome in patients with optic nerve pit serous retinal detachment of the macula. Ophthalmology 1990;97:1539-42.
- Avci R, Yilmaz S, Inan UU, Kaderli B, et al. Long-term outcomes of pars plana vitrectomy without interal limiting membrane peeling for optic disc pit maculopathy. Eye (Lond). 2013;27(12):1356-67.
- Shukla D, Kalliath J, Tandon M, Vijayakumar B. Vitrectomy for optic disc with macula schisis and outer retinal dehiscence. Retina. 2012;32(7):1337-42.
- Hirakata A, Inoue M, Hiraoka T, McCuen BW 2nd. Vitrectomy without laser treatment or gas tamponande for macular detachment associated with an optic nerve pit. Ophthalmology. 2012;119(4):810-8