West Coast Retina
Case of the Month
Mar, 2016
Presented by Ananda Kalevar, MD
A 68 year-old woman presents with blurred vision in both eyes.

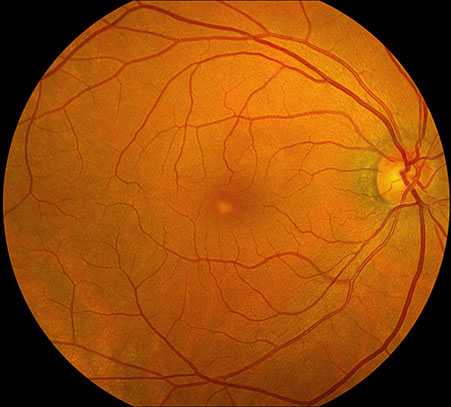
A
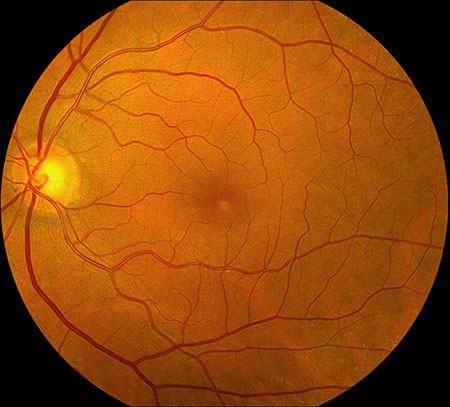
B
Figures 1A-B: Color fundus photographs of the right (A) and left (B) eyes. Accumulation of yellowish subfoveal vitelliform material is noted, that is more prominent in the right eye than the left eye.
Case History:
A 68 year-old woman presents with a one-year history of blurred central vision in both eyes. Her past ocular history, medical history, family history, social history and medications were non-contributory.
On examination, best-corrected visual acuity was 20/30 in both eyes. Intraocular pressure was normal in both eyes. The anterior segment examination was unremarkable. The posterior segment exam was remarkable for an accumulation of yellowish subfoveal deposits (figure 1A-B), more prominently seen in the right eye.
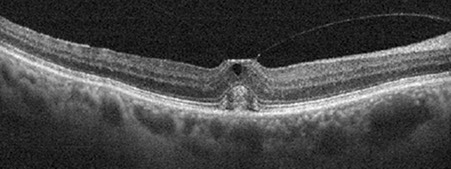
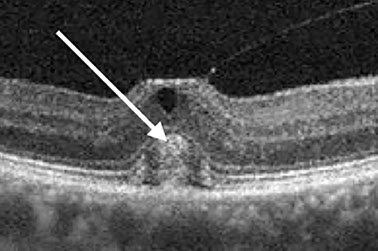
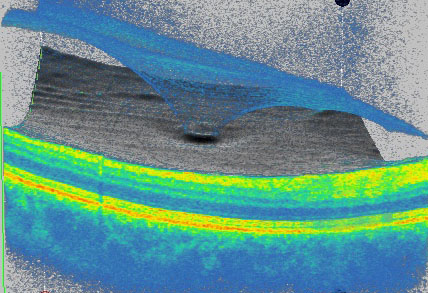
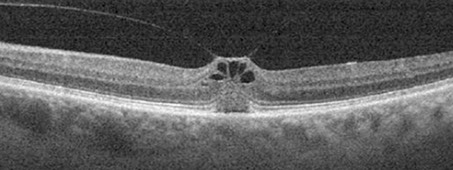
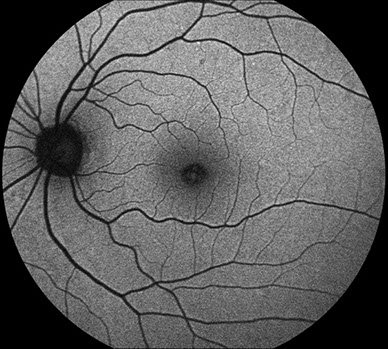
Spectral domain OCT of the right eye (figure 2A, inset and B) shows an attached hyaloid at the center of the macula causing tractional elevation of the fovea. Inner cystic changes are seen along with hyperreflective material in the subretinal space bounded anteriorly by the ellipsoid layer. Similar OCT changes are seen in the left (figure 2C). Fundus autofluorescence of both eyes (figure 3A-B) showed mild hyperautofluorescence which corresponded to the yellowish sub-foveal deposits, more prominently seen in the left eye.
A
B
Figures 2A-C: SD-OCT of the right (A, inset and left (C) eyes. In each eye, we see an attached posterior hyaloid causing tractional elevation of the fovea with inner cystic changes (mostly in the left eye). There is the “cotton ball” sign (white arrow) in the right eye (Fig 2A and inset). Fig 2B is a 3D rendering of the vitreomacular interface and shows a very discrete, focal vitreomacular attachment.
C

A
B
Figures 3A-B: Fundus autofluorescence images of the right (A) and left (B) eyes. Mild hyperautofluorescence areas seen more prominently in the left than in her right which correspond to the visible yellowish subfoveal material.
What is your Diagnosis?
Differential Diagnosis
Epiretinal membrane, Best’s disease, Pattern Dystrophy, Neovascular AMD, Solar Retinopathy, CSR, Popper’s maculopathy
Additional Case History
The patient has been monitored closely and over the course of four years she has remained stable with good vision. At her most recent examination her visual acuity was 20/40 in both eyes. Fundus examination remained similar demonstrating pseudo-vitelliform lesions. On SD-OCT, vitreomacular traction persisted without resolution or progression.
Discussion
Reese and coworkers in 1970 first described loss of vision associated with an incomplete separation of the vitreous from the macula.1 They coined the term, vitreomacular traction (VMT) syndrome and were able to confirm these findings histologically. With the advent of OCT, significant insight about the vitreoretinal interface (VRI) has been achieved.
OCT has helped with the understanding of the pathophysiology of the posterior vitreous detachment (PVD). As the eye ages, gel liquefaction occurs and through this a cascade of events is triggered whereby the vitreoretinal adhesions are weakened.2 OCT has demonstrated that PVD usually commence in the perifoveal macula and then with continued liquefaction and collapse of the vitreous body, posterior hyaloid detaches from the inner limiting membrane. Presence of a Weiss ring is usually indicative of vitreo-papillary separation and the completion of a unremarkable PVD. Complications of PVD are more likely in patients with ocular inflammatory diseases, hereditary vitreoretinal conditions, myopia, trauma and vascular diseases.2
Abnormal PVD progression can result in various complications. Occasionally, the adhesion of the vitreous cortex to the macula can result in traction known as VMT syndrome. Recently, the International Vitreomacular Traction Study (IVTS) Group3 developed an OCT-based classification system maculopathies associated with vitreomacular traction. They defined vitreomacular adhesion (VMA) as unperturbed retinal anatomy and VMT as a distorted foveal anatomy due to vitreous traction. In addition, they classified the size of attachment into either focal (<1500 microns) or broad (>1500 microns).3
VMT can occur at any age, sex or race. Patients with VMT can suffer from decreased vision, blurry vision, micropsia or metamorphopsia. On clinical exam, VMT can have various presentations such as macular edema, subretinal fluid, pseudo-vitelliform lesion (our case above), pseudo-hole (Figure 4) or epiretinal membrane. The most significant complication from VMT is progression to a full thickness macular hole.
Management options for VMT are observation, pharmacologic agents such as Ocriplasmin or vitrectomy surgery to peel the posterior hyaloid from the macula, thereby releasing traction.4 The majority of patients with VMT maintain good vision with mild amounts of metamorphopsia. Many patients that are observed without treatment undergo spontaneous complete PVD and relief of the traction at the fovea. A minority, for unknown reasons, continue to maintain traction for many years as seen in our case presented.

Figure 4: Color fundus photographs of the right eye of another patient with vitreomacular traction. A pseudo-hole appearance is evident.
Take Home Points
- Understanding of the vitreomacular traction syndrome has been significantly improved with the advent of OCT.
- VMT can have several clinical presentations.
- Management options for VMT are observation, treatment with pharmacologic agents, or surgery.
Want to Subscribe to Case of the Month?
References
- Reese AB, Jones IS, Cooper WC. Vitreomacular traction syndrome confirmed histologically. Am J Ophthalmol. 1970;69:975–977.
- Bottos J, Elizalde J, Arevalo JF, Rodrigues EB, Maia M. Vitreomacular traction syndrome. J Ophthalmic Vis Res. 2012, Apr; 7(2): 148-161.
- Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, Sadda SR, Sebag J, Spaide RF, Stalmans P. The international vitreomacular traction study group classification of vitreomacular adhesion, traction and macular hole. Ophthalmology. 2013; 1-9.
- McDonald HR, Johnson RN, Schatz H. Surgical results in the vitreomacular traction syndrome. Ophthalmology. 1994;101:1397–1402.