West Coast Retina
Case of the Month
March, 2015
Presented by Kevin Patel, MD

A 40 year-old woman presenting with distorted vision in the right eye.
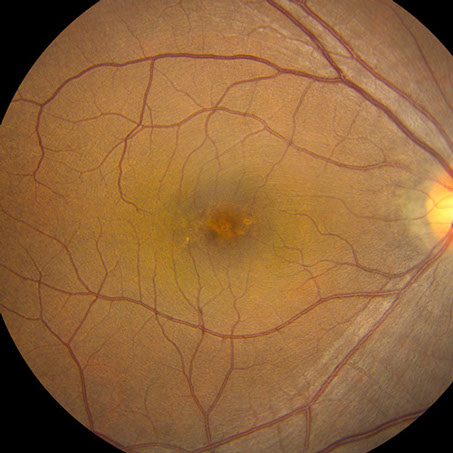
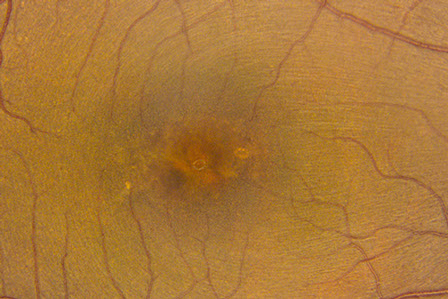
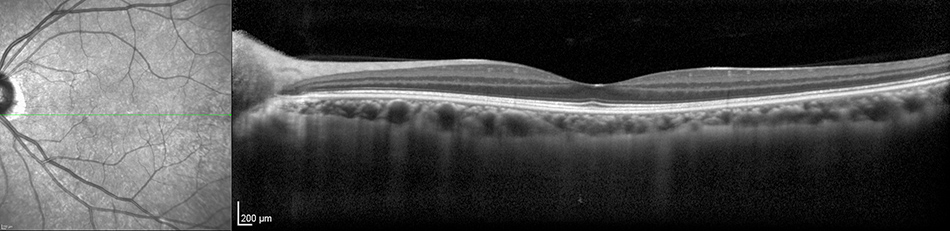
Figure 1 and Detailed view: Color fundus photograph of the right macula. Note the pigment mottling under the fovea.
Case History
A 40 year-old Caucasian woman presented with a one-year history of distorted vision in the right eye. The patient was unsure of the definite time of onset, but felt that her central vision became gradually distorted over the past year. She complained that images were intermittently moving or shaking. There was no associated pain or other ocular symptoms. The patient denied any visual changes in her left eye. There was no significant past ocular history. Her past medical history was only remarkable for genital herpes and fibromyalgia. She did not take any medications regularly. The patient’s social history was noncontributory while her family history was only significant for her mother having glaucoma.
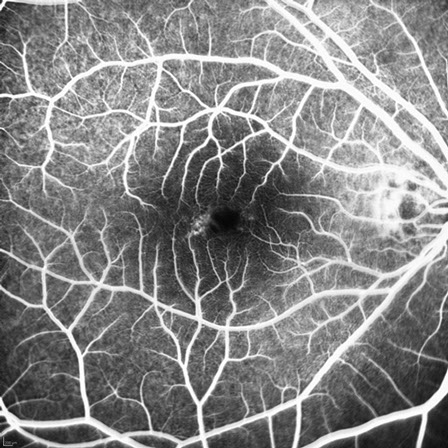
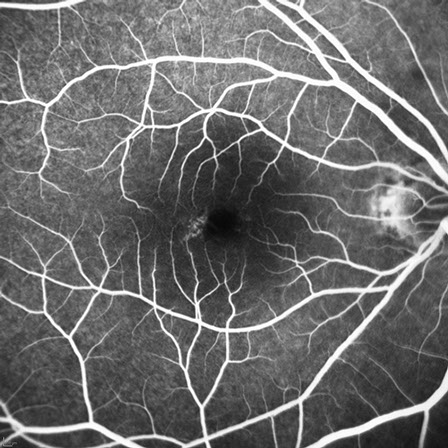
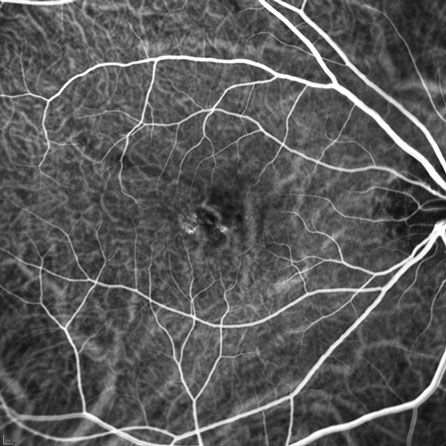
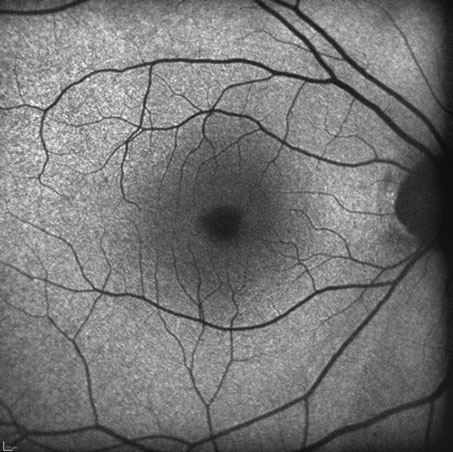
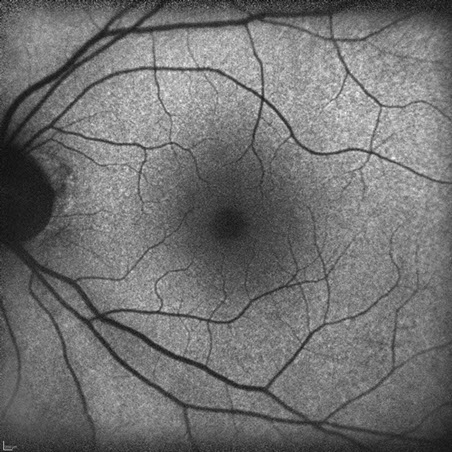
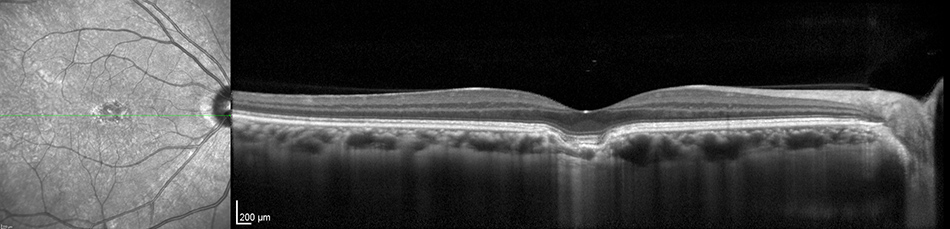
On examination, best-corrected visual acuity was 20/20 in the right eye and 20/16 in the left eye. Intraocular pressure and anterior segment examination was normal for both eyes. Posterior segment examination of the right eye revealed foveal RPE changes but was otherwise normal (Figure 1 and Detail). The posterior segment of the left eye was completely normal. Fluorescein angiography (FA) of the right eye only showed focal areas of hyperfluorescence temporal to the fovea (Figure 2A) which did not change in intensity in the late (Figure 2B) frames, suggestive of window defects from RPE atrophy. FA of the left eye was unremarkable. Indocyanine green angiography (ICGA) of the right eye showed mild, early punctate hyperfluorescence on the nasal and temporal edge of the fovea (Figure 3A) with increased fluorescence in the late phase (Figure 3B). ICGA of the left eye was normal. Fundus autofluorescence was unremarkable in both eyes (Figures 4A and B). Optical coherence tomography (OCT) of the right eye demonstrated a discrete depression within the choroid within the central fovea. The retinal contour was relatively normal as were the inner retinal layers. The RPE band followed the contour of the choroidal excavation without separation from the photoreceptors (Figure 5A). However, disruption of the RPE and RPE-Outer Segment junction was present on the temporal edge of the excavation (Fig 5A, detail). Spectral domain OCT of the left eye was unremarkable (Figure 5B).
A
B
Figure 2A and B: Fluorescein angiogram of the right macula. Note the mild increased fluorescence at the temporal edge of the fovea. No leakage is present.
A

B
Figures 3A and B: Indocyanine angiogram of the right macula. Mild increased fluorescence is present under the fovea which increases somewhat in the later phases of the study.
A
B
Figures 4A and B: Fundus autofluorescence of the right and left eye. The studies are unremarkable.
A
B
Figures 5A and B: Horizontal Spectral Domain Optical Coherence Tomography scan through the right and left macula. The study is normal in the left eye. In the right eye, note the discrete depression under the fovea. The overlying retinal layers appear to deep into the depression and are mostly intact (see detail below)
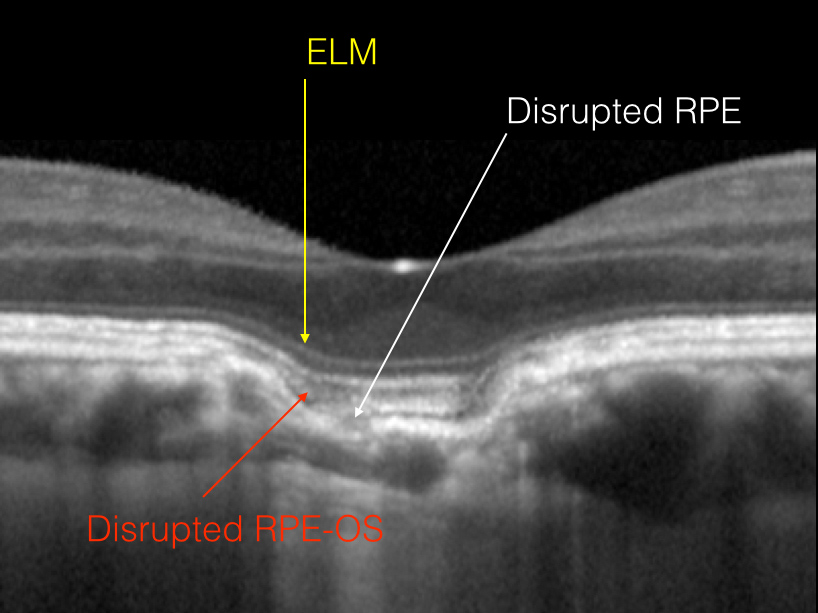
Figure 5A detail view: Note the disruption of the RPE on the temporal edge of the fovea. The overlying RPE and outer segments appear to be disrupted as well, but the ELM remains intact. The retinal layers deep into the choroidal depression
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis of focal outer retinal and choroidal cavitation includes focal choroidal excavation (FCE), macular staphyloma, and causes of choroidal thinning, such as trauma, posterior uveitis, retinal or choroidal vascular disease, or prior retinal or choroidal infection.
Given that our patient’s choroidal excavation was unilateral, associated with good vision and intact outer retina, and not associated with prior ocular disease or trauma, the findings are consistent with focal choroidal excavation.
Discussion
Focal choroidal excavation (FCE) was first described by Jampol et al as a case report in which excavation of the choroid was detected by time-domain OCT in an eye with good visual acuity and normal appearance of the overlying retina.1 Several other studies have subsequently described the condition, and expanded the findings with the aid of more advancing imaging. The precise etiology is also unclear and it is debated whether this condition is congenital or occurs secondary to multifactorial causes.2,3 Long-term prognosis is not known due to the limited follow-up of reported series.
There are several distinct clinical features of FCE. Most patients have relatively good visual acuity, are mildly myopic, and have unilateral involvement. Some patients describe metamorphopsia. On funduscopic examination, the presence of choroidal excavation is usually subtle and difficult to appreciate. A mild disturbance of the retinal pigment epithelium may be seen. Yellowish plaque-like lesions can also be seen in FCE. Fluorescein angiographic findings can vary depending on the degree of RPE alterations. ICG often shows relative hypofluorescence in the area of excavation; there may also be punctate areas of hyperfluorescence. Spectral domain OCT is revealing for FCE. In most instances, the excavation is located subfoveal or juxtafoveal; however, it may be extrafoveal. Occasionally, two areas of excavation are present, often near each other. FCE can be divided into two categories based on OCT characteristics: conforming and nonconforming. In both categories, the inner retina is intact and the RPE band follows the contour of the choroidal excavation. In conforming FCE, there is no separation between the photoreceptor tips and the RPE (as is the case in our patient). In nonconforming FCE, there is separation of the photoreceptors from the RPE with subretinal fluid accumulating in the space between. For conforming eyes, all of the outer retinal layers are visible on OCT, while in nonconforming eyes, there can be attenuation of the ellipsoid zone and RPE bands.2,3
The clinical course of FCE is not well understood given the lack of long-term follow-up of patients with the condition. Margolis et al described 13 eyes of 12 patients with FCE, and lesions in 12 of the 13 eyes remained stable while the remaining eye developed choroidal neovascularization (CNV). Mean follow-up in this study, however, was less than 1 year.2 Obata et al described 21 eyes of 17 patients with FCE over a mean follow-up of 37 months. The appearance of the excavation was unchanged in all eyes while central serous chorioretinopathy and choroidal neovascularization developed in 1 eye each.3
While the etiology of FCE is still unknown, there may be an association with other ocular diseases, such as central serous chorioretinopathy and choroidal neovascularization.4-6 A recent study by Ellabban et al examined 116 consecutive eyes with central serous chorioretinopathy and found FCE in 9 eyes (7.8%) of 8 patients. All these patients were myopic, in contrast to most patients with central serous chorioretinopathy who are emmetropic or hyperopic. In all 9 eyes, the focal excavations were located within or adjacent to areas of fluorescein leakage. Seven of these 9 eyes underwent ICGA, and the focal excavations were located in within areas of choroidal hyperpermeability. The relationship of FCE and the pathogenesis of central serous retinopathy is uncertain.4
A number of studies have established that CNV can be a rare complication of FCE. Xu et al specifically looked at the characteristics of CNV in eyes with FCE. Fifteen eyes of 12 patients had CNV secondary to FCE. The CNV in all eyes were classic as defined by their FA findings. CNV occurred in both conforming and nonconforming FCE. All CNV lesions responded well to intravitreal anti-VEGF agents. CNV regressed after just a single injection in 13 of 15 eyes. The remaining 2 eyes required only a second injection to achieve resolution of the CNV. Also, nonconforming FCE converted to conforming FCE after successful treatment of CNV.5 Lee et al also reviewed 16 eyes of 16 patients with both FCE and CNV. Nine eyes had Type 1 CNV lesions (beneath the RPE) while 7 eyes had Type 2 CNV (in the subneurosensory retinal space). Seven of the 9 eyes with Type 1 CNV had classic CNV on FA, and the other 2 eyes had occult CNV. All 7 eyes with Type 2 CNV had classic CNV. Fifteen of the 16 eyes received treatment with intravitreal anti-VEGF therapy. CNV resolution was achieved in all of the treated eyes with a mean of 3.7 injections during a mean follow-up period of 14.5 months.6
Take Home Points
- Focal choroidal excavation (FCE) is a condition of unknown etiology in which there is excavation of the choroid with normal overlying retina.
- Patients with FCE typically maintain good vision as these lesions tend to remain unchanged over time.
- Choroidal neovascularization is a rare complication of FCE that may reduce vision; however, it tends to respond well to treatment with anti-VEGF therapy.
Want to Subscribe to Case of the Month?
References
- Jampol LM, Shankle J, Schroeder R, et al. Diagnostic and therapeutic challenges. Retina. 2006;26:1072-1076.
- Margolis R, Mukkamala SK, Jampol LM, et al. The expanded spectrum of focal choroidal excavation. Arch Ophthalmol. 2011;129:1320-1325.
- Obata R, Takahashi H, Ueta T, et al. Tomographic and angiographic characteristics of eyes with macular focal choroidal excavation. Retina. 2013;33:1201-1210.
- Ellabban AA, Tsujikawa A, Ooto S, et al. Focal choroidal excavation in eyes with central serous chorioretinopathy. Am J Ophthalmol. 2013;156:673-683.
- Xu H, Zeng F, Shi D, et al. Focal choroidal excavation complicated by choroidal neovascularization. Ophthalmology. 2014;121:246-250.
- Lee JH, Lee WK. Choroidal neovascularization associated with focal choroidal excavation. Am J Ophthalmol. 2014;157:710-718.