West Coast Retina
Case of the Month
May, 2011
A 34-year-old woman with multiple blind spots.
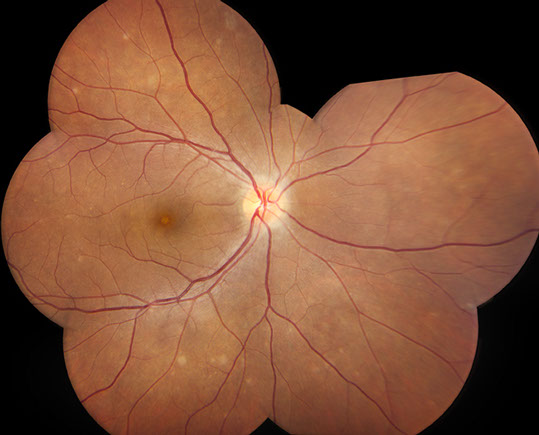
Figure 1: Color photo montage of the right eye showing optic disc hyperemia and multiple scattered deep retinal yellow-white dots on examination.
Case History
A 34-year-old Hispanic woman presented with a four-day history of blurry vision in her right eye with photophobia, multiple blind spots, and intermittent photopsias. She denied any eye pain or floaters and her review of systems was negative. She was myopic and her past medical history was unremarkable.
On examination, her best-corrected visual acuity was 20/50 in the right eye and 20/20 in the left. There was no relative afferent pupillary defect. The intraocular pressure and anterior segment examination was normal in both eyes.
There was mild vitritis in the right eye. Fundus examination revealed a hyperemic optic disc with attenuation of the foveal reflex in the right eye and multiple scattered yellow-white deep retinal dots of varying sizes concentrated in the posterior pole with extension to the equator (Fig. 1). The left eye was normal.
Fluorescein angiography revealed early hyperfluorescence and late staining of the lesions with leakage from the optic disc of the right eye (Figure 2). Autofluorescence imaging showed subtle hyperautofluorescence of the spots (Figure 3). Indocyanine green angiography revealed multiple hypofluorescent spots, more numerous than seen on examination and fluorescein angiography, (with some peripapillary hypofluorescence, Figure 4). Spectral domain optical coherence tomography (OCT) through a lesion at the fovea and another in the parafoveal area showed disruption of the outer segment-RPE junction as well as the photoreceptor inner segment-outer segment (IS-OS) junction (Figure 5).
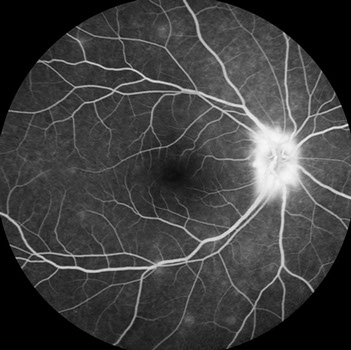
Figure 2: Fluorescein angiography revealed early hyperfluorescence and late staining of the lesions with leakage from the optic disc of the right eye
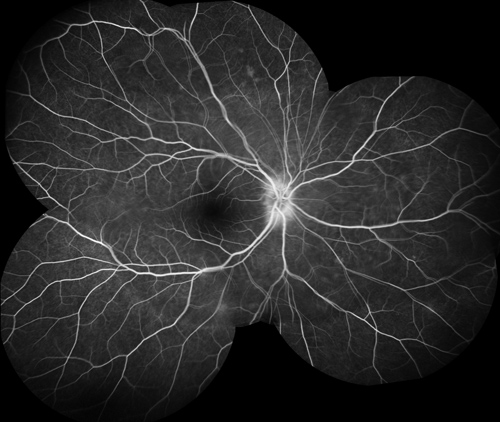

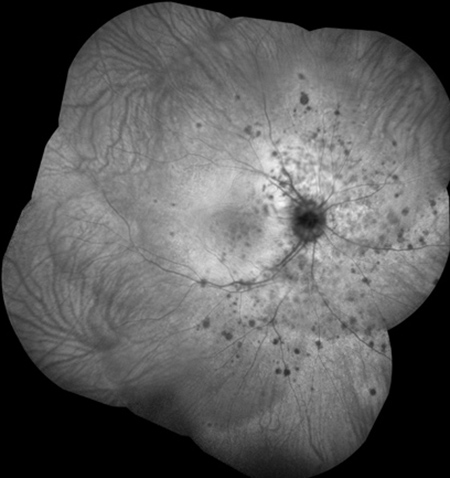
Figure 3: Fundus autofluorescence imaging showed subtle hyperautofluorescence of the deep retinal spots.
Figure 4: Indocyanine green angiography revealed multiple hypofluorescent spots, more numerous than seen on examination and fluorescein angiography.
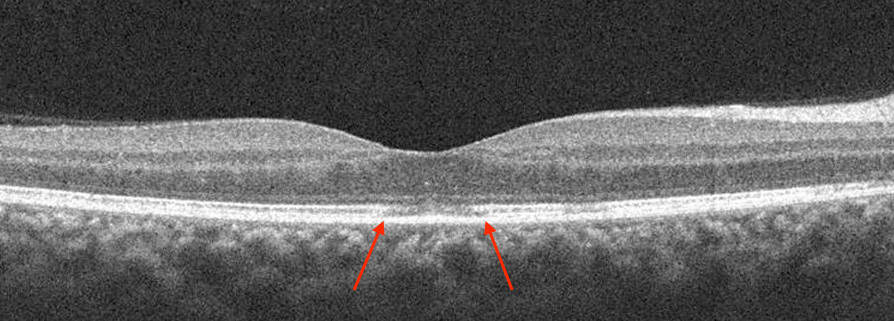
Figure 5: Spectral domain optical coherence tomography through a lesion at the fovea and another in the parafoveal area showed disruption of the outer segment-RPE junction as well as the photoreceptor inner segment-outer segment (IS-OS) junction (arrows).
What is your Diagnosis?
Differential Diagnosis
A 34-year-old Hispanic woman presented with acutely symptomatic blurry vision, intermittent photophobia, photopsias, and an enlarged blind spot in her right with optic disc hyperemia and multiple scattered yellow-white dots on examination (Figure 1).
The differential diagnosis includes acute idiopathic blind spot enlargement syndrome, acute zonal occult outer retinopathy, multifocal choroiditis, acute macular neuroretinopathy, and multiple evanescent white dot syndrome.
Discussion
MEWDS is an idiopathic inflammatory condition of the retina that typically presents with acute, unilateral (80%) blurred or decreased vision with central or peripheral scotomata in otherwise healthy young (10–47 years), moderately myopic females (90%), frequently following a flu-like prodrome.1 Funduscopy during the acute phase of the disease reveals multiple, discrete white or yellow spots (100–200 μm) at the level of the retinal pigment epithelium (RPE) or deep retina, typically in a perifoveal location. These spots are transitory and are frequently missed; they leave instead a granular macular pigmentary change. There may be few associated vitreous cells, mild blurring of the optic disc, and in rare instances, isolated vascular sheathing.1
Fluorescein angiography is characteristic, revealing punctate hyperfluorescent lesions in a wreath-like configuration surrounding the fovea that stain late. Indocyanine green (ICG) angiography shows multiple hypofluorescent lesions that are more numerous than those seen on examination (with hypofluorescence around the optic nerve) or on fluorescein angiography, and that typically fade with resolution of the disease suggesting pathologic choroidal nonperfusion or RPE inflammation.2-4 Visual field abnormalities are variable and include generalized depression, paracentral or peripheral scotomata, and enlargement of a blind spot and correlate well with ICG angiography.2, 3 Electroretinographic (ERG) abnormalities include diminished a-wave and early receptor potential amplitudes, both of which are reversible. The multifocal ERG and electro-oculogram (EOG) localize the disease process to the RPE/photoreceptor complex.5
The spectral domain OCT images show subtle disruptions of the photoreceptor IS/OS junction in eyes with MEWDS. This may suggest that MEWDS is more likely associated with RPE inflammation. Swollen, but intact, RPE cells appear normal on OCT imaging but the inflammation of the RPE cells could interrupt the orientation of photoreceptor outer segments acutely, causing attenuation of OCT signal from the IS/OS junction as the outer segments become misaligned.6
The prognosis for MEWDS is excellent, with visual recovery occurring between two to ten weeks without treatment.
Our case presented with a classic picture of sudden visual blurring in one eye, hyperemic optic nerve head, and multiple deep whitish retinal spots. The ICG findings and spectral domain OCT were characteristic of MEWDS, and the clinical course resulted in the expected recovery of vision.
Take Home Points
- MEWDS is an inflammatory chorioretinopathy of unknown etiology that predominantly presents unilaterally in young myopic females with photopsias, blurred vision, and blind spots.
- Though MEWDS is predominantly a clinical diagnosis, spectral domain OCT and ICG angiography are useful adjuncts in diagnosis and monitoring . OCT shows subtle disruptions of the photoreceptor IS/OS junction. Some of the early choroidal lesions that are undetectable on clinical examination are more apparent on ICG angiography.
- MEWDS has an excellent prognosis and requires no treatment.
Want to Subscribe to Case of the Month?
References
- Jampol LM, Sieving PA, Pugh D, Fishman GA, Gilbert H. Multiple evanescent white dot syndrome, I: clinical findings. Arch Ophthalmol 1984;102:671-674.
- Borruat FX, Auer C, Piguet B. Choroidopathy in multiple evanescent white dot syndrome. Arch Ophthalmol 1995;113:1569–1571.
- Obana A, Kusumi M, Miki T. Indocyanine green angiographic aspects of multiple evanescent white dot syndrome. Retina 1996;16:97–104.
- Gross NE, Yannuzzi LA, Freund KB et al. Multiple evanescent white dot syndrome. Arch Ophthalmol. 2006 ;124:493-500.
- Sieving PA, Fishman GA, Jampol LM, Pugh D. Multiple evanescent white dot syndrome, II: electrophysiology of the photoreceptors during retinal pigment epithelial disease. Arch Ophthalmol. 1984;102:675-679.
- Nguyen MH, Witkin AJ, Reichel E, Ko TH, Fujimoto JG, Schuman JS, Duker JS. Microstructural abnormalities in MEWDS demonstrated by ultrahigh resolution optical coherence tomography. Retina 2007;27:414-8.