West Coast Retina
Case of the Month
May, 2013
A 30 year-old man with loss of vision in his left eye.
Presented by Paul Stewart, MD

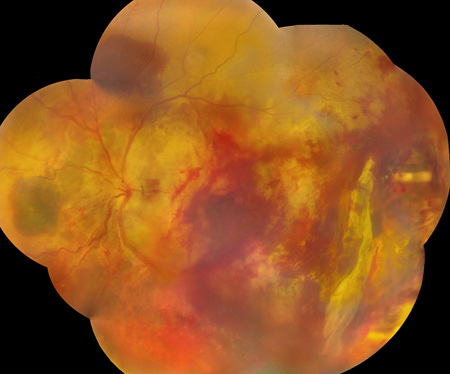
Figure 1: Color fundus photo montage of the left eye. Temporally there is an area of scrolled retina and choroid with bare sclera immediately anteriorly. There are large areas of subretinal hemorrhage as well as preretinal and vitreous hemorrhage
Case History
A 30 year-old male prison inmate was referred for evaluation of trauma to the left eye. He had been involved in an altercation that resulted in a guard firing a 40mm diameter hard foam projectile. The non-lethal crowd dispersal missile was fired from 15 feet away and hit the man in the left eye causing an orbital fracture, lid laceration and trauma to the left retina. He was in good health without any medications. He had no history of prior ocular surgery or trauma.
His left eye had hand motion vision. The anterior segment examination revealed subconjunctival hemorrhage. The dilated fundus examination (Figure 1) showed mild vitreous hemorrhage. There were scattered retinal hemorrhages, along with whitening of the central retina. The vessels were engorged and there was swelling of the optic nerve. In the temporal periphery there was disruption of the retina and choroid with visible bare sclera. On fluorescein angiography (Figure 2) there was subretinal blockage, leakage from the regions around the disc.
His right eye was 20/25 and the anterior segment was normal. The intraocular pressure was 15mmHg. The dilated fundus examination showed a yellow-orange lesion along the inferior arcade (Figure 3). The remainder of the fundus examination was unremarkable. B-scan ultrasonography (Figure 4) showed a highly echogenic focus in the area corresponding to the yellow-orange lesion.
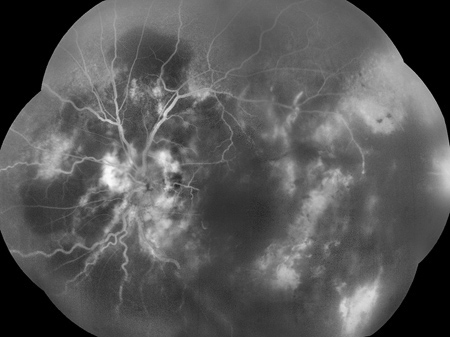
Figure 2: Fluorescein angiogram montage of the left eye. Dye leakage around the disc is present and there is some blockage of fluorescence centrally due to preretinal and vitreous hemorrhage. There are linear areas of deep hyperfluorescence in multiple locations due to choroidal rupture.

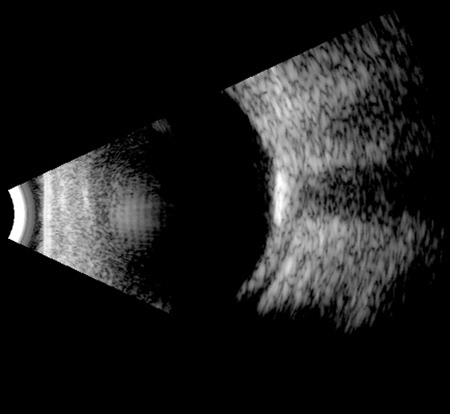
Figure 3: Color fundus photo of the right eye. Note the yellow-orange lesion, sharply-delineated choroidal inferonasal to the fovea.
Figure. 4: B-scan ultrasound of the right eye. Note the highly echogenic lesion. This corresponds to the yellow-orange lesion seen on fundus examination.
What is your Diagnosis?
Discussion
This patient suffered a high velocity impact trauma that caused a chorioretinal rupture, multiple choroidal ruptures, commotio retina and vitreous hemorrhage. Traumatic chorioretinal rupture was originally termed chorioretinitis sclopetaria and is a rare finding in non-penetrating ocular trauma. The first report was in the German literature in 1901 of an injury associated with a bullet that passed next to the eye.1 The derivation of sclopetaria may refer to the Latin “sclopetum,” which was a type of 14th century Italian handgun. It may also derive from the old English verb “sclow,” which means to scratch or tear. Although the original descriptions included the terms retinitis or chorioretinitis, an inflammatory component is not thought to contribute to this disease process.
Martin, et al. in 1994 described a series of sclopetaria patients and proposed that the mechanism of injury is rapid deformation of the globe by an object or its shock wave.3 They postulate that there is a sudden increase in the tensile stresses of the sclera, vitreous and other layers resulting in rupture of the choroid and retina, but not of the elastic posterior hyaloid. There is subsequent retraction of the choroid and retina, exposing bare sclera. Because the retina and choroid retract as a unit there is no access for fluid to the subretinal space that could lead to a retinal detachment. The posterior hyaloid is typically intact as these injuries tend to happen in young males with formed vitreous, perhaps also preventing fluid from having access to the subretinal or suprachoroidal space. Because of the lack of detachment, these eyes should be monitored by observation alone. There have been reports of tears occurring remote from the area of chorioretinal rupture months after the initial injury, making continued observation of these patients important.
Our patient has been followed with observation. His vision remains hand motion and his retina remains attached. The lack of visual recovery in this case is likely related to the injury to the macula.
Commotio retinae is produced by blunt trauma to the eye opposite the site of impact. It is associated with initial loss of vision and typically of normal visual recovery.4 There can be disruption of the outer segments of the photoreceptors and damage to the retina pigment epithelium. In some cases with more damage to the RPE, there is leakage from the RPE on angiography and subsequent scarring in these regions that can limits visual recovery.
Our patient was also found to have an unrelated choroidal osteoma in the right eye. Choroidal osteoma is a benign tumor with bone that replaces the choroid. They are typically unilateral and seen in young women. The tumors can show growth and can be associated with choroidal neovascular membranes.5 Decalcification of the tumor can be a sign of chronicity. Our patient’s choroidal osteoma will need to be watched. If it begins to proceed toward the fovea or if there is a choroidal neovascular membrane that develops, he will need treatment to preserve vision in what is now his better seeing eye.
Take Home Points
- Traumatic chorioretinal rupture, or sclopetaria, is a result of high-velocity injury.
- Sclopetaria does not need surgical intervention due to the characteristic response of the eye to the injury.
- Visual prognosis depends on the extent of involvement of the macula and angiography can be helpful by looking at the RPE leakage.
- Choroidal osteoma is a benign tumor with bone replacing the choroid.
Want to Subscribe to Case of the Month?
References
- Goldzier W. Beitrag zur pahtologie der orbitalen schussverletzungen. Z. Augenheikd. 1901. 6: 277.
- Kimoto K, Kishi D, Kono H, et al. Diagnosis of an isolated retinal astrocytic hamartoma aided by optical coherence tomography. Acta Ophthalmol. 2008. 86: 921-922.
- Martin DF, Awh CC, McCuen BW, et al. Treatment and pathogenesis of traumatic chorioretinal rupture (sclopetaria). Am J Ophthalmol. 1994. 117: 190-200.
- Mansour AM, Green WR, Hogge C. Histopathology of commotio retinae. Retina. 1992. 12: 24-28.
- Shields CL, Sun H, Demirci H, et al. Factors predictive of tumor growth, tumor decalcification, choroidal neovascularization, and visual outcome in 74 eyes with choroidal osteoma. Arch Ophthalmol. 2005. 123: 1658-1666.