West Coast Retina
Case of the Month
November, 2014
Presented by Kevin Patel, MD
A 56 year-old man presenting with decreased vision in the left eye

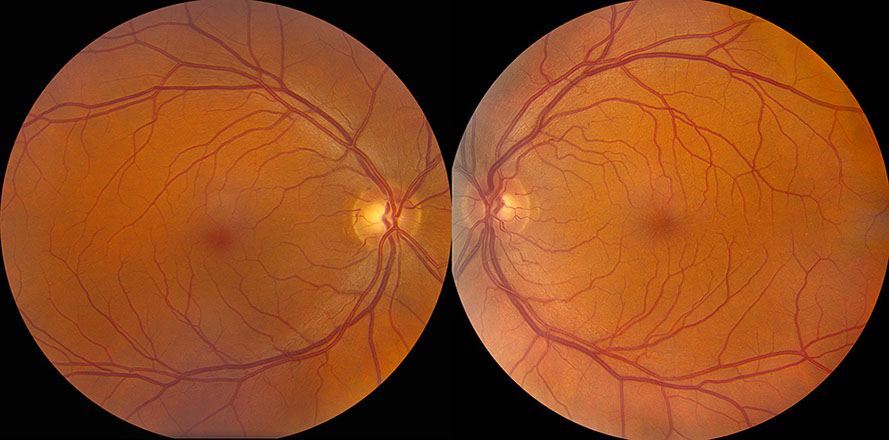

Figuress 1A and B: Color fundus photographs of the right (A) and left (B) eyes. The macula of the right eye (A) appears normal. Note the foveal striae in the left eye (B and inset).
Case History:
A 56 year-old white man was referred with decreased vision in the left eye for three-months duration with a gradual onset. He denied eye pain or any other ocular symptoms. He also denied any significant past ocular history. Past medical history was only significant for hypercholesterolemia for which he takes lovastatin and low-dose aspirin. The patient’s social history was noncontributory, and there was no family history of any ocular conditions.
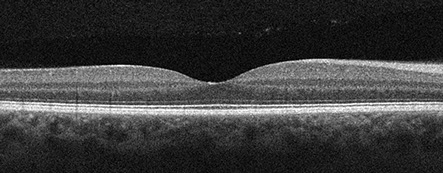
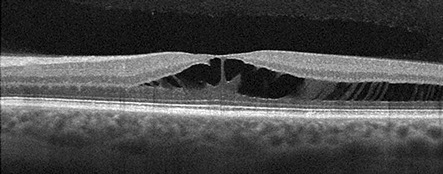
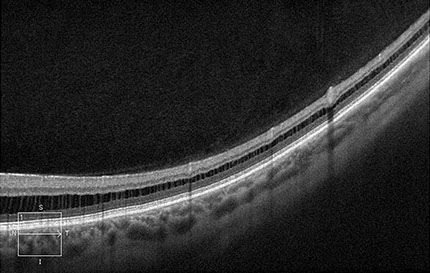
On examination, visual acuity was 20/25 in the right eye and 20/63 in the left eye. Intraocular pressure and anterior segment examination were normal in both eyes. Posterior segment examination of the right eye was significant for a normal appearing macula, and peripheral RPE changes (Figure 1A). The left eye had foveal striae (Figure 1B) and peripheral RPE changes. Optical coherence tomography (OCT) of the macula was normal in the right eye (Figure 2A) but demonstrated significant foveomacular retinoschisis with splitting predominantly within the outer plexiform layer (Figure 2B). No evidence of vitreomacular traction was present in the left eye. OCT imaging also showed that the retinoschisis continued to the temporal midperiphery (Figure 2C). Fluorescein angiography was normal in both eyes. Specifically no retinal vascular leakage was noted in the macula of the left eye. En face reconstruction of the OCT of the left macula revealed photoreceptor axons and elongated Müller cell processes extending through the the area of foveomacular retinoschisis in Henle’s layer (Figure 3).
A
B
C
Figures 2A-C: Optical coherence tomography of the macula is unremarkable in the right eye (A). The left eye (B) demonstrates significant foveomacular retinoschisis with involvement predominantly within the Henle’s layer. There is no visible vitreomacular traction. The retinoschisis continues temporally into the midperiphery (C).
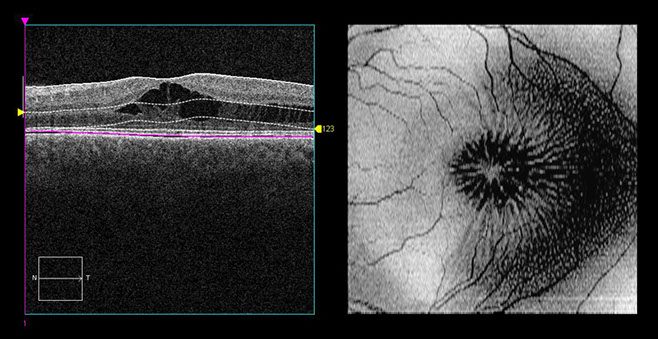
Figure 3: En face optical coherence tomography of the left macula displays elongated photoreceptor axons and Müller cell processes within the area of foveomacular retinoschisis (within Henle’s layer). A reference image for the en face optical coherence tomography shows the area of analysis (between the dotted lines).
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis for conditions with foveomacular retinoschisis includes congenital juvenile X-linked retinoschisis, myopic degeneration, optic pit maculopathy, glaucoma, myotonic dystrophy, vitreomacular traction, and stellate nonhereditary idiopathic foveomacular retinoschisis. Non-leaking cystoid macular edema can often be confused with or considered synonymous with foveomacular retinoschisis, and its causes must also be considered in the differential. These include enhanced S-cone syndrome (or Goldmann-Favre syndrome), retinitis pigmentosa, nicotinic acid maculopathy, and certain chemotherapy medications such as paclitaxel and docetaxel.
Additional Case History
The patient has been followed for approximately five years. The foveomacular retinoschisis of the left eye has remained stable. The patient’s visual acuity in the left eye has fluctuated at each clinic visit, but most recently, it was 20/25. The right eye examination has remained normal over this time with no areas of retinoschisis. He has continued on the same medications of lovastatin and low-dose aspirin. The patient has no other significant ocular conditions, and there is no family history of any ocular diseases, including any form of retinoschisis. Given the unilaterality of the foveoschisis, good visual acuity, lack of other associated ocular conditions, and limited exposure to medications, the most likely diagnosis is stellate nonhereditary idiopathic foveomacular retinoschisis.
Discussion
Foveomacular retinoschisis is most often associated with congenital juvenile X-linked retinoschisis (CXLR), a disorder secondary to a mutation in the RS1 gene coding for retinoschisin. All affected individuals have foveal schisis with half also developing peripheral schisis. This disorder almost exclusively occurs in males due to the X-linked inheritance pattern.1
Pathologic myopia associated with staphyloma is another cause of foveomacular retinoschisis that appears to be due to fovemacular traction.2 Likewise, partial posterior vitreous detachment has also been implicated in causing foveal schisis in myopic patients.3
Optic disc pits can also lead to foveomacular retinoschisis as fluid extends into the inner and outer retinal layers.4 Glaucoma is another ocular condition that has been associated with foveal schisis. Glaucomatous optic nerve damage leads to thinning of the nerve fiber layer and optic disc cupping. This, in turn, may lead to microholes and structural defects in the inner retinal layers around the optic disc, forming a pathway for fluid to enter a potential schisis cavity.5
Several other conditions or medications can cause non-leaking cystoid macular edema, which can be considered synonymous with foveomacular retinoschisis. Enhanced S-cone syndrome (or Goldmann-Favre syndrome) is an autosomal recessive disorder with many ocular manifestations. In addition to foveal schisis, there are RPE pigmentary alterations, cataracts, and optically empty vitreous. The macular and peripheral retinoschisis tends to be quite extensive, and patients generally have severely reduced vision.6 Nicotinic acid and taxane-derived medications (paclitaxel and docetaxel) can lead to cystoid spaces in the outer plexiform layer and inner nuclear layer that do not leak on FA. These usually resolve with discontinuation of the medication.7-9
Ober and colleagues recently described 22 eyes in 17 patients who had foveomacular retinoschisis without a known hereditary or acquired predisposing condition.10 These cases were felt to describe a new condition termed “stellate nonhereditary idiopathic foveomacular retinoschisis.” Twelve patients had unilateral findings while 5 had bilateral findings. Initial visual acuity was 20/50 or better in all eyes with a mean visual acuity of 20/27. On examination, none of the eyes demonstrated features of vitreoretinal interface abnormalities or myopic traction maculopathy. None of the patients had a family history of CXLR or other hereditary maculopathies. Eight patients (11 eyes) had genetic testing performed for mutations in the RS1 gene, and no mutations were detected. OCT of the macula demonstrated splitting within the outer plexiform layer with lesser involvement of the outer nuclear layer in all eyes. Visual acuity remained relatively stable (at least 20/40 or better) in all but one eye, which had a decrease from 20/20 to 20/200 after development of subretinal fluid.10
TAKE HOME POINTS:
- The differential diagnosis for foveomacular retinoschisis is broad as this condition can be secondary to a large number of other ocular conditions.
- Stellate nonhereditary idiopathic foveomacular retinoschisis is an uncommon cause of unilateral foveomacular retinoschisis, and the diagnosis can be made when there is a lack of other associated ocular conditions and no family history of retinoschisis.
- Most patients with this condition are minimally symptomatic and have relatively good visual acuity.
Want to Subscribe to Case of the Month?
References
- Sieving PA, MacDonald IM, Meltzer MR, et al. X-linked juvenile retinoschisis. In: Pagon RA, Adam MP, Bird TD, et al, eds. GeneReviews. Seattle, WA; University of Washington, Seattle; updated May 12, 2009.
- Gaucher D, Haouchine B, Tadayoni R, et al. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol. 2007;143:455-62.
- VanderBeek BL, Johnson MW. The diversity of traction mechanisms in myopic traction maculopathy. Am J Ophthalmol. 2012;153:93-102.
- Lincoff H, Lopez R, Kreissig I, et al. Retinoschisis associated with optic nerve pits. Arch Ophthalmol. 1988;106:61-7.
- Zumbro DS, Jampol LM, Folk JC, et al. Macular schisis and detachment associated with presumed acquired enlarged optic nerve head cups. Am J Ophthalmol. 2007;144:70-4.
- Theodossiadis PG, Koutsandrea C, Kollia AC, et al. Optical coherence tomography in the study of the Goldmann-Favre syndrome. Am J Ophthalmol. 2000;129:542-4.
- Joshi MM, Garretson BR. Paclitaxel maculopathy. Arch Ophthalmol. 2007;125:709-10.
- Spirn MJ, Warren FA, Guyer DR, et al. Optical coherence tomography findings in nicotinic acid maculopathy. Am J Ophthalmol. 2003;135:913-4.
- Teitelbaum BA, Tresley DJ. Cystic maculopathy with normal capillary permeability secondary to docetaxel. Optom Vis Sci. 2003;80:277-9.
- Ober MD, Freund KB, Shah M, et al. Stellate nonhereditary idiopathic foveomacular retinoschisis. Ophthalmology. 2014;121:1406-13.