West Coast Retina
Case of the Month
Nov, 2015
Presented by Ananda Kalevar, MD
A 60 year-old woman presents with decreased vision in the left eye.

A
B
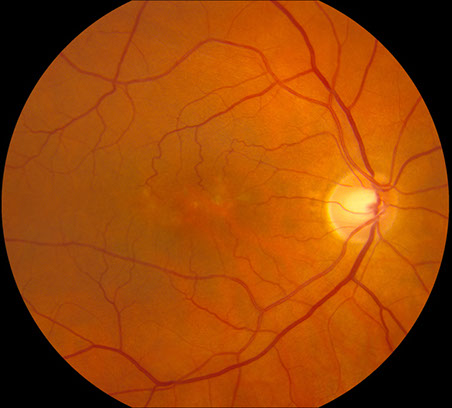
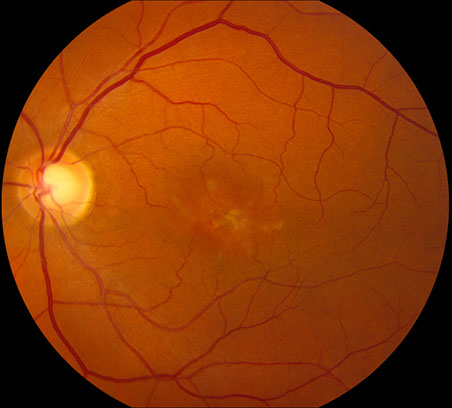
Figures 1A-B: Color fundus photographs of the right (A and C) and left (B and D) eyes. Branching yellowish material with associated retinal pigment epithelial atrophy is present in both eyes, but more prominent in the left eye
C

D
Case History
A 60 year-old woman presents with decreased central vision in her left eye over the last year. She stated that her father had "age-related macular degeneration” at age 75 and that her son had been diagnosed with Best Disease. There was no significant past ocular history. Her past medical history, social history and medications were non-contributory.
On examination, best-corrected visual acuity was 20/16 and 20/63 in the right and left eye, respectively. Intraocular pressure was normal in both eyes. The anterior segment examination was unremarkable. The posterior segment exam was remarkable for an accumulation of yellowish-grey pigment in the central macula (figure 1A-D), more prominently seen in the left eye which appeared to be deposited in a spoke-like pattern surrounded by a zone of depigmentation, resembling a butterfly.
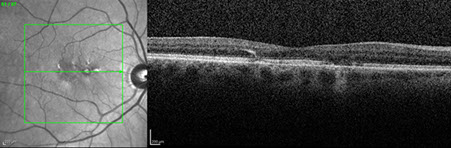
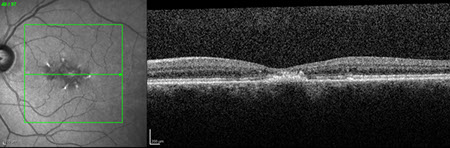
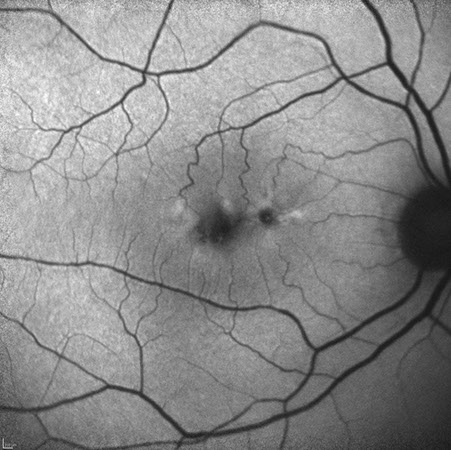
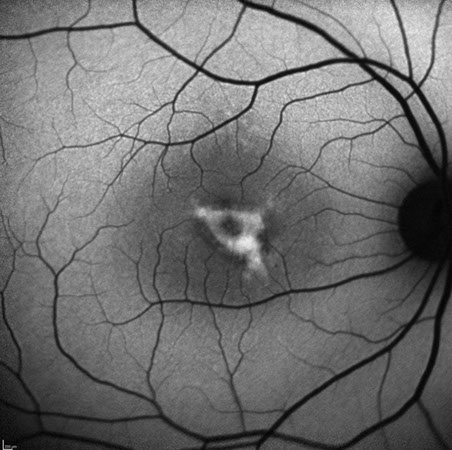
Spectral domain OCT of the right eye (figure 2A) showed changes in the outer retina, specifically patchy loss of the ellipsoid layer. Similar OCT changes are seen in the left eye (figure 2B) along with a neurosensory detachment filled with an amorphous mass with no clear structures differentiable. Fundus autofluorescence of the right eye (figure 3A) shows an area with irregular borders that has decreased autofluorescence surrounded by patchy increased autofluorescence. In the left eye (figure 3B), a larger patch of decreased autofluorescence with surrounding patchy increased autofluorescence was present.
A
B
Figures 2A and B: OCT of right (A) and left (B) eyes. Outer retinal changes and specifically patchy loss of the ellipsoid layer is evident in the right eye. Similar changes are seen in the left along with a neurosensory detachment are seen filled with an amorphous mass with no clear structures differentiable.
A

B
Figures 3A and B: Fundus autofluorescence of right (A) and left (B) eyes. Areas of reduced autofluorescence centrally are noted with a branching pattern of increased autofluorescence.
What is your Diagnosis?
Differential Diagnosis:
There are a number of different disorders to consider that can be associated with similar findings as seen in this patient including: AMD, Drusenoid RPE detachment, Best, Pattern Dystrophy, CSR, VMT, Epiretinal membrane, MEK inhibitor related vitelliform, Desferrioxamine related vitelliform, Paraneoplastic vitelliform retinopathy, Pseudoxanthoma elasticum
Additional Case History:
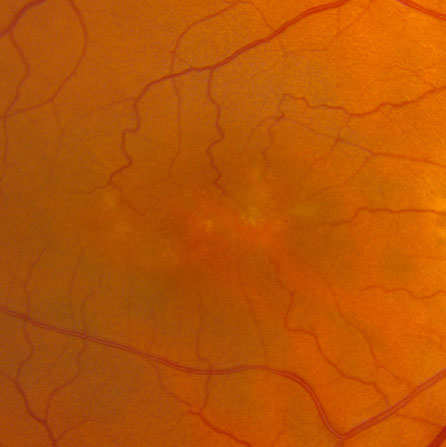
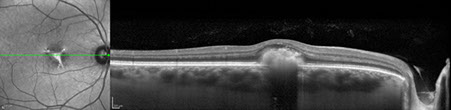
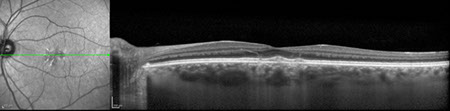
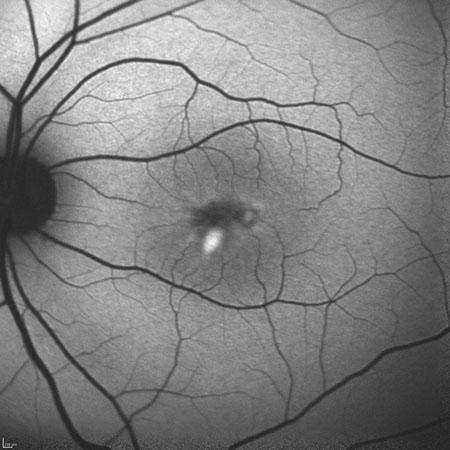
Her 39 year-old son, who had been told he had Best Disease, was evaluated. He had blurry vision in both eyes for the past 20 years. Best-corrected visual acuity was 20/63 and 20/25 in the right and left eye, respectively. His examination was remarkable for vitelliform lesions in the central macula of both eyes, more prominently seen in the right eye (figure 4A-B). On SD-OCT, neurosensory detachments are seen filled with an amorphous mass with no clear structures differentiable (figure 5A-B). On fundus autofluorescence increased autofluorescence is seen surrounded by decreased fundus autofluorescence (figure 6A-B).
DNA analysis was performed on both members of the family. Their DNA was found to be heterozygous for PRPH2 Gene (formerly termed peripherin/RDS gene). In addition, the son was found to be negative for BEST1 analysis.

A

B
Figures 4A and B: Color fundus photographs of the son’s right (A) and left (B) eyes. A large irregularly shaped vitelliform lesion is present in the right eye, and the left eye has a smaller area of material with some subtle branching pattern of material in the superonasal fovea.
A
B
Figures 5A and B: SD-OCT scans of the son's right and left eye. Note the collection of amorphous hyperreflective material primarily in the right eye.
A
B
Figures 6A and B: Fundus autofluorescence studies of the right (A) and left (B) eyes. Note the hyperfliuorescent areas that mostly correspond to the yellow vitelliform lesions seen on the fundus photos. There are some areas of reduced fluorescence as well.
Discussion
Pattern Dystrophies are a heterozygous group of inherited retinal dystrophies characterized by pigment changes at the level of the retinal pigment epithelium (RPE) which affects both eyes, specifically the macula and usually has a progressive nature.1 A broad spectrum of clinical appearances exist which are specified by the distribution of pigment. The classification of Gass discriminates between five main forms: adult-onset foveomacular vitelliform dystrophy, butterfly-shaped pigment dystrophy, reticular dystrophy, pattern dystrophy simulating fundus flavimaculatus and fundus pulverulentus.2
A mutation in PRPH2 (OMIM # 179605) is the most common cause of all these various patterns. It encodes the peripherin protein which plays a structural role in outer-segment discs in rod and cone photoreceptors.3 A heterozygous state of PRPH2 usually results in disease indicating inheritance is autosomal dominant. Clinical manifestation can be variable for the same point mutation causing a reticular pattern in one patient and adult-onset foveomacular dystrophy in another patient with the same mutation even among families as seen in our case. It has been described that one patient had a butterfly-shaped lesion in one eye and a vitelliform lesion in the other eye.3 Age of onset for pattern dystrophy is quite variable with more phenotypic variability evident with age. Vision loss typically occurs in the 4th or 5th decade in life due to geographic atrophy and/or choroidal neovascularization in 42% of cases.4 Patients with pattern dystrophy may also experience macular photostress.3 Frequently full-field electroretinograms and electro-oculograms are unremarkable.
Adult-onset foveomacular vitelliform dystrophy typically has a fundus examination showing bilateral focal autofluorescent vitelliform lesions in the posterior pole near the fovea.3 These lesions are smaller in size than those seen in Best disease. Several stages of this subtype of pattern dystrophy exist progressing from vitelliform lesion to pseudohypopyon to vitelliruptive to atrophy. PRPH2 is the most common gene affected in this subtype but BEST1, VMD2, IMPG1/2 have also been reported in a minority of cases.4
Butterfly dystrophy typically has a fundus examination where pigmentation may be yellow, white or black and accumulate in a pattern that appears like wings from a butterfly.3
Reticular dystrophy typically has a network of pigmented lines that resemble fishnet which are very well defined on fluorescein angiography and fundus autofluorescence.3
Pattern dystrophy resembling Stargardt disease typically has a fundus examination that is challenging to differentiate from true Stargardt disease. Though the majority of Stargardt disease patients have autosomal recessive inheritance, some autosomal dominant forms have been described. The later age of onset, relatively good central visual acuity and absence of dark choroid on fluorescein angiography are findings that may aid in the diagnosis of pattern dystrophy.3
Fundus pulverulentus is the rarest form of the pattern dystrophy. It is vaguely described in the literature as having a granular appearance to the macula with mottling of the retinal pigment epithelium.3
Treatment is guided to monitoring any sequelae that develop such as choroidal neovascularization or atrophy. There is no treatment that can halt progression at the moment.
Take Home Points
- Pattern Dystrophies are a heterogenous group of inherited retinal dystrophies characterized by bilateral macular pigment changes at the level of the RPE and usually has a progressive nature.
- A large spectrum of phenotypes exist with a mutation in PRPH2 (autosomal dominant inheritance) being the most common cause of all these various patterns.
- Careful clinical examination accompanied with a multi-modal imaging approach is necessary to differentiate pattern dystrophy sub types from the various entities in their differential diagnosis.
Want to Subscribe to Case of the Month?
References
- Marmor MF, Byers B. Pattern dystrophy of the pigment epithelium. Am J Ophthalmol 1977; 84 (1): 32-44.
- Gass JDM. Stereoscopic Atlas of Macular Diseases: Diagnosis and Treatment. 4th ed. St. Louis: CV Mosby; 1997: 314-325.
- Ryan S. Retina, 5th ed. 2013: 875-880
- Francis PJ, Schultz DW, Gregory AM et al. Genetic and phenotypic heterogeneity in pattern dystrophy. Br J Ophthalmol 2005; 89(9): 1115-9.
- Chowers I, Tiosano et al. Adult-onset foveomacular vitelliform dystrophy: A fresh perspective. Progress in Retinal and Eye Research 2015; 47: 64-85.