West Coast Retina
Case of the Month
October, 2009
46-year-old man with acute unilateral vision loss.
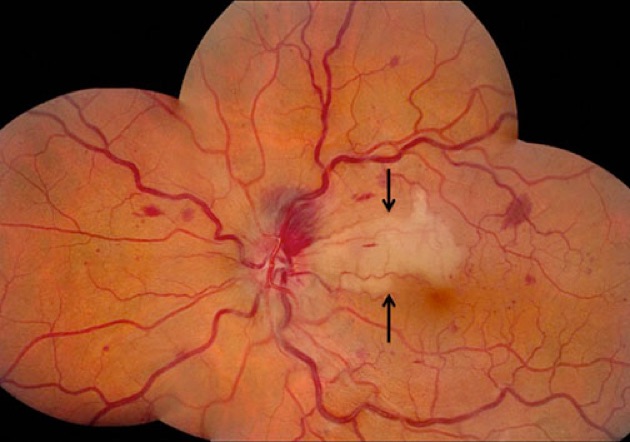
Figure 1: Fundus photo montage of the left eye. Note the dilated and tortuous veins due to a central retinal vein occlusion. There is an area of retinal whitening involving the papillomacular bundle and the region superior to the macula (black arrows).
Case History
A 46-year-old man presented with a one day history of blurred vision in his left eye. Three days prior to presentation, he noted a transient episode of blurred central vision in the left eye. The past medical, ocular, family, and social history were non-contributory.
The visual acuity was 20/25 in each eye. The intraocular pressure and anterior segment examination were normal. The fundus examination of the right eye was within normal limits. In the left eye, there were dilated and tortuous retinal veins, intraretinal hemorrhages in all four quadrants and a prominent area of retinal whitening in the papillomacular bundle extending just superior to the macula (Figure 1). The nerve was swollen. Fluorescein angiography revealed an arterial occlusion corresponding to the retinal whitening seen clinically (Figure 2).
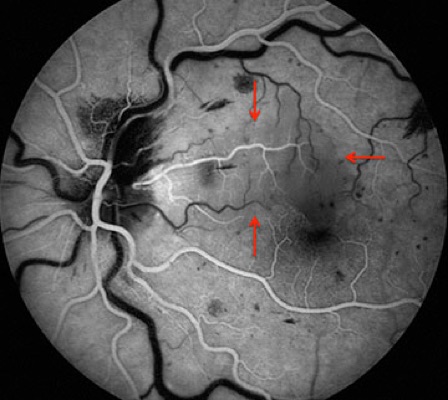
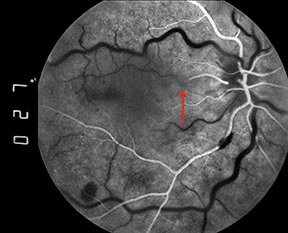
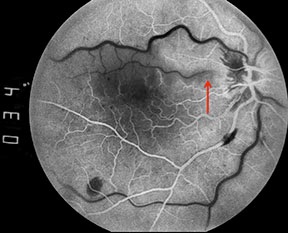
Figure 2: Early phase fluorescein angiogram of the left eye. Note the area of vascular nonperfusion corresponding to the area of whitening seen clinically (red arrows).
What is your Diagnosis?
Discussion
This patient has a cilioretinal artery occlusion secondary to a central retinal vein occlusion. The cilioretinal artery contributes to macular circulation in roughly 20% of eyes.1 Cilioretinal artery occlusion occurs in approximately 5% of all cases of central retinal vein occlusion (CRVO).2 The perfusion pressure of the posterior ciliary artery, which supplies both the choroidal circulation and the cilioretinal artery, is lower than that of the central retinal artery. An increase in intraluminal capillary pressure occurs after CRVO because there is resistance to retinal venous outflow. As a result, perfusion of the retinal capillary bed supplied by the cilioretinal artery may become impaired in the presence of CRVO.3 In our case, the cilioretinal artery had already re-perfused by the time the patient was evaluated and the fluorescein angiogram done (Fig 3, yellow arrow).
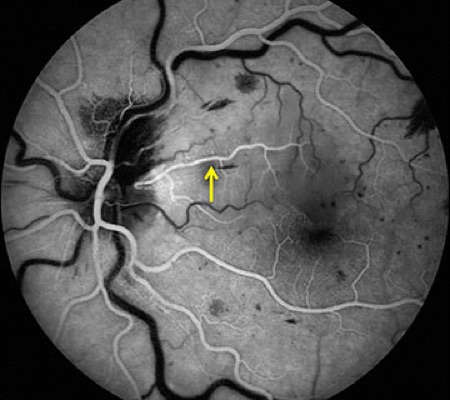
Figure 3: Early phase fluorescein angiogram of the left eye. Note that the cilioretinal artery has re-perfused and demonstrates complete fluorescein dye filling (yellow arrow).
Discussion (Continued)
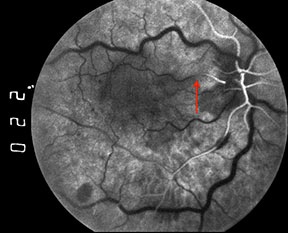
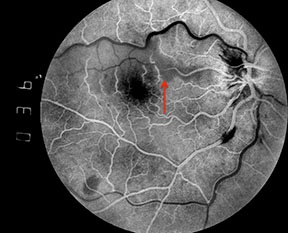
Filling of the cilioretinal artery occurs concurrently with that of the choroidal circulation, about 1 to 2 seconds prior to filling of the retinal arterioles. In eyes with cilioretinal artery occlusion, however, a delay in filling may be observed.4 This delayed filling is more likely to be observed if fluorescein angiography is performed soon after the onset of symptoms, prior to the development of venous collaterals.5 Intermittent cilioretinal artery occlusion may also result in a fluorescein angiographic finding of an oscillating blood column within the cilioretinal artery, with filling during systole and nonfilling during diastole (Figures 4).
Transient vision loss, as observed by the patient presented herein, is thought to be common in patients with combined CRVO and cilioretinal artery occlusion.5 Visual outcomes in combined CRVO and cilioretinal artery occlusion are usually favorable unless the CRVO is ischemic or the entire parafoveal capillary net is affected by the cilioretinal artery occlusion.3,5
Figures 4: A series of early phase fluorescein angiograms on another patient with a combined central retinal vein occlusion and cilioretinal artery occlusion demonstrates an interesting phenomenon. Note that the column of fluorescein dye in the cilioretinal artery advances and retreats with systole and diastole (red arrows).

Take Home Points
- The perfusion pressure of the cilioretinal artery, which is supplied by the posterior ciliary artery, is less than that of the central retinal artery. Therefore, occlusion of the cilioretinal artery often occurs as a result of elevated intraluminal capillary pressure caused by CRVO
- Fluorescein angiography may reveal an obstruction, a delay in filling, or even an oscillating column of blood in the cilioretinal artery
- Transient vision loss is a common complaint in combined CRVO and cilioretinal artery occlusion
- Visual outcomes are usually favorable, particularly in young patients with non-ischemic CRVO and in the absence of involvement of the entire parafoveal capillary net by cilioretinal artery occlusion
Want to Subscribe to Case of the Month?
References
- Justice J, Jr., Lehmann RP. Cilioretinal arteries. A study based on review of stereo fundus photographs and fluorescein angiographic findings. Arch Ophthalmol 1976;94(8):1355-8.
- Fong AC, Schatz H, McDonald HR, et al. Central retinal vein occlusion in young adults (papillophlebitis). Retina 1992;12(1):3-11.
- Schatz H, Fong AC, McDonald HR, et al. Cilioretinal artery occlusion in young adults with central retinal vein occlusion. Ophthalmology 1991;98(5):594-601.
- Sharma S, Brown G. Retinal Artery Obstruction. In: Retina, 3 ed. Vol. 2. Ryan S, editor. St. Louis: Mosby, 2001; 1360-1.
- Hayreh SS, Fraterrigo L, Jonas J. Central retinal vein occlusion associated with cilioretinal artery occlusion. Retina 2008;28(4):581-94.