West Coast Retina
Case of the Month
October, 2013
Presented by Steven Williams, MD
A 44-year-old woman presents with chronic vision loss in the right eye

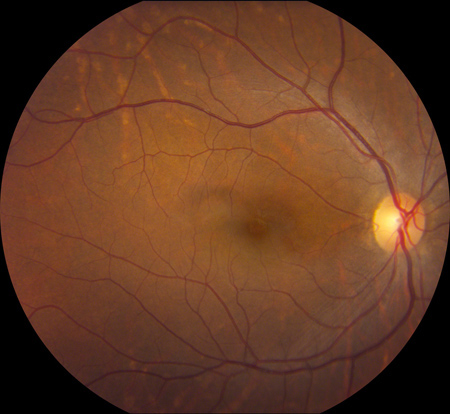
A
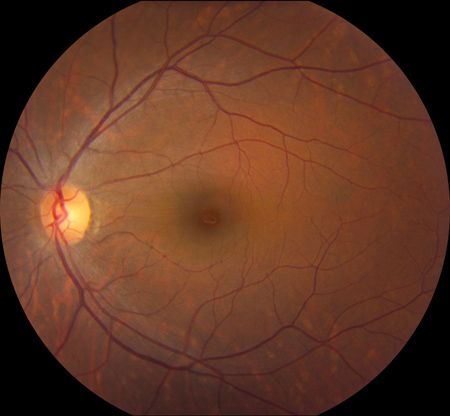
B
Figures 1A and B: Color fundus photographs of the macula and nerve of the right and left eye. Note the mild irregularity of the macula sheen in the superior macula of the right eye. The left eye appears normal.
Case History
A 44-year-old, black woman presented with non-progressive difficultly with near vision her right eye for one year. Her past ocular history was unremarkable. Past medical history was significant for rheumatic heart disease, mitral stenosis requiring valvuloplasty, and atrial fibrillation. She was taking metoprolol and prodaxa. She denies any allergies. Family history and social history were unremarkable.
Vision in the right eye was 20/20 and 20/16 in the left eye. Intraocular pressure was normal bilaterally. Examination of the anterior segment was normal in both eyes. Posterior segment examination of the right eye was remarkable for a mild irregularity of the macula sheen in the superior macula without evidence of intraretinal hemorrhage or edema. Posterior segment examination of the left eye was unremarkable (Figure 1A, B).
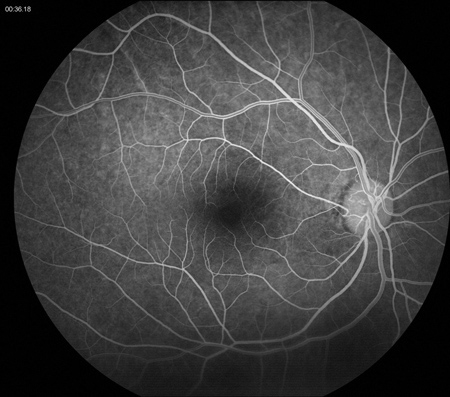
Spectral domain optical coherence tomography (SD-OCT) revealed a sector of nerve fiber layer atrophy and inner retinal atrophy with preservation of the outer retina in the superior macula in the right eye. Outside of this sector, the SDOCT of the right eye appeared normal. SD-OCT of the left eye was normal (Figure 2A, B, C). Fluorescein angiography demonstrated normal arteriovenous transit without evidence of retinal hypofluorescence, window defect or leakage in either eye. There was a cilioretinal artery present in the right eye and the area of retinal thinning appeared to correspond to the vascular distribution of the cilioretinal artery (Figure 3A, B).
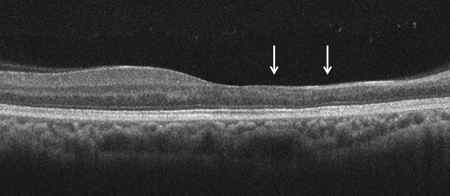
A
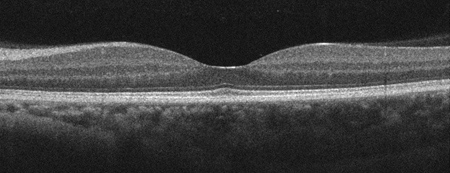
B
C
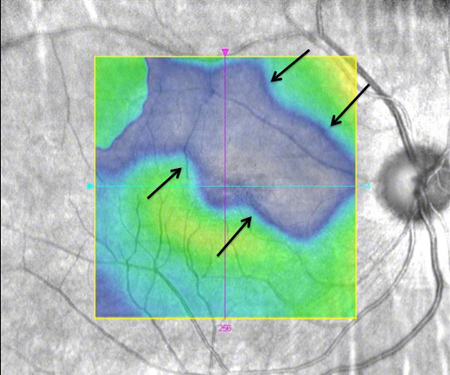
Figures 2A-C: Horizontal SD-OCT of the right macula (Fig. A) demonstrates thinning of the nerve fiber layer and loss of the inner retinal layers in the nasal macula (arrows) of the right eye with a normal temporal macula. Normal SD-OCT of the left macula (Fig. B). Figure 2C: Retinal thickness map of the right macula reveals a large sector of retinal thinning in the superior macula (black arrows).
A

B
Figures 3A and B: Fluorescein angiography of the right eye reveals normal retinal perfusion without evidence of embolus, or vascular obstruction, hypo- or hyperfluorescence. There is a cilioretinal artery in the distribution of the retinal thinning.
What is your Diagnosis?
Differential Diagnosis
Diagnostic considerations for sectoral inner retinal thinning include retinal artery occlusion and optic nerve disease. Causes of retinal artery occlusions include embolic disease (e.g. carotid and valvular heart disease), thrombosis associated with systemic causes of hypercoagulation (e.g. homocystinuria, protein S deficiency, protein C deficiency, Factor V Leiden deficiency, oral contraception, essential thrombocythemia, polycythemia, antiphospholipid syndrome), collagen vascular disease (e.g. systemic lupus, polyarteritis nodosa), and giant cell arteritis. Other uncommon causes for retinal artery occlusion include Lyme disease, syphilis, Behcet's disease and migraine. There was no evidence of optic nerve disease.
Discussion
Given the acute onset of symptoms in close temporal proximity to the mitral valvuloplasty, a clinical diagnosis of occlusion of the cilioretinal artery secondary to presumed cardiac embolus was made.
Retinal artery occlusion is a disease of older adults, with an average age of onset of 60 years. Systemic risk factors include hypertension, diabetes mellitus, smoking, ischemic heart disease and cerebrovascular disease. Retinal artery occlusions are more common in men and are associated with atheromatous plaques of the carotid artery in 50-75% of cases. Cardiac embolic disease can occur spontaneously or in the setting of angioplasty. Embolic disease can be seen in younger patients with valvular heart disease secondary to rheumatic fever, mitral valve prolapse, or other congential anomalies. One or more emboli may be visualized within the arterial tree, often lodged at bifurcations. Emboli may be composed of cholesterol (yellow, iridescent in appearance), platelet fibrin (dull, gray-white in appearance) or calcium (white, nonrefractile in appearance).
If retinal artery obstruction is only partial or of short duration, there may be no permanent retinal damage. More complete arterial blockage leads to retinal whitening and swelling within the arterial distribution distal to the obstruction. Clinically, this is seen as a cotton-wool patch that fades over several weeks, leaving an area of inner retinal atrophy, which can be a subtle ophthalmoscopic finding suggestive of prior retinal arterial occlusion. Acutely, fluorescein angiography often shows complete or partial reduction in blood flow, with variable leakage of fluorescein at the site of the obstructing emboli. However, weeks later, angiography may fail to demonstrate the arterial obstruction since flow may be re-established later. Focal vascular attenuation and sclerosis may be the only late findings in a long-standing arterial occlusion. There is rarely angiographic evidence of concomitant embolic disease in the choroidal circulation.
In the acute phase of retinal arterial occlusion, OCT demonstrates thickening and hyperreflectivity of the inner retinal layers, with decreased reflectivity of the underlying photoreceptor and retinal pigment epithelial cell layers. Retinal thickness may resolve to near normal thickness within 1 month and progresses to marked inner retinal atrophy over the next several months. In a case such as ours with cilioretinal artery occlusion, the prognosis for vision is dependent on the extent of macular perfusion that is supplied by the cilioretinal artery. Although visual prognosis is poor in central retinal artery occlusion, 35% of patients retain 20/100 or better visual acuity. With central retinal artery occlusion, neovascular glaucoma is seen in 2.5 to 15% of patients and typically develops within 2-3 months of the onset of symptoms.
Take Home Points
- Branch retinal artery occlusion tends to affect older adults with vascular risk factors and is characterized by acute inner retinal whitening and thickening which resolves over several weeks.
- Longstanding retinal artery occlusion may have subtle findings including retinal thinning, mild vascular attenuation without angiographic evidence of vascular occlusion.
- SD-OCT demonstrates inner retinal thickening and hyperreflectivity in the acute phase and inner retinal atrophy in the chronic phase of the arterial occlusion.
Want to Subscribe to Case of the Month?
References:
- Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion associated systemic and ophthalmic abnormalities. Ophthalmology 2009;166:1928-36.
- Kollarits CR, Lubow M, Hissong SL. Fretinal strokes. I. Incidense of carotid atheromata. JAMA 1972;222:1273-5.
- Rodrigues IA. Acute and chronic spectral domain optical coherence tomography features of branch retinal artery occlusions. BMJ Case Rep. May 8, 2013.
- Shah VA, Wallace B, Sabates NR. Spectral domain optical coherence tomography findings of acute branch retinal artery occlusion from calcific embolus. Indian J Ophthalmol. 2010;58(6):523-4.
- Karacorlu M, Ozdemir H, Arf Karacorlu S. Optical coherence tomography findings in branch retinal artery occlusion. Eur J Ophthalmol 2006;16:352-3.
- Cella W, Avila M. Optical coherence tomography as a means of evaluating acute ischaemic retinopathy in branch retinal artery occlusion. Acta Ophthalmol Scand 2007;85:799-801.
- Falkenberry SM, Ip MS, Blodi BA, Gunther JB. Optical coherence tomography findings in central retinal artery occlusion. Ophthalmic Surg Lasers Imaging 2006;37:502-5.
- Cornut PL, Bieber J, Beccat S, Fortoul V, et al. Spectral domain OCT in eye with retinal artery occlusion. J Fr Ophtalmol 2012;35(8):606-13.
- Ghazi NG, Tilton EP, Patel B, Knape RM, et al. Comparison of macular optical coherence tomography findings between postacute retinal artery occlusion and nonacute optic neuropathy. Retina 2010;30(4):578-85.
- Leung CK, Tham CC, Mohammed S, Li EY, et al. In vivo measurements of macular and nerve fiber layer thickness in retinal arterial occlusion. Eye (Lond) 2007;21(12):1464-8.
- Augsburger JJ, Magargal LE. Visual prognosis following treatment of acute central retinal artery obstruction. Br J Ophthalmol 1980;64:913-7.
- Duker JS, Brown GC. Iris neovascularization associated with obstruction of the central retinal artery. Ophthalmology 1988;95:1244-50.
- Duker JS, Brown GC. Neovascularization of the optic disc associated with obstruction of the central retinal artery. Ophthalmology 1989;96:87-91.