West Coast Retina
Case of the Month
Oct, 2015
Presented by Kevin Patel, MD
A 57 year-old Asian man presenting with peripheral retinal hemorrhages in the right eye.


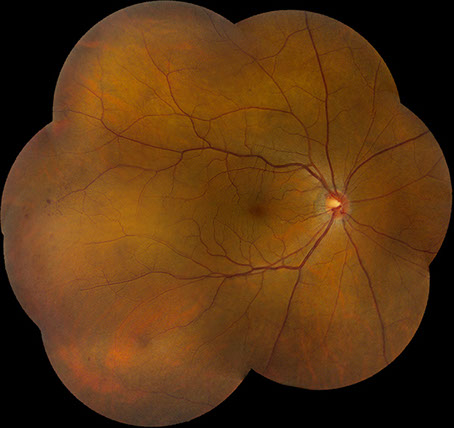
A

C
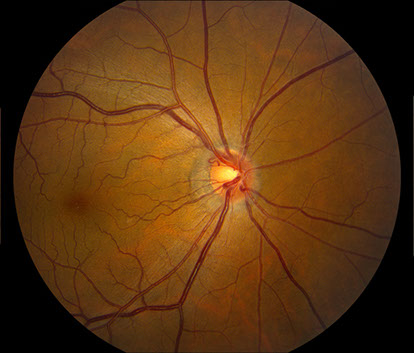
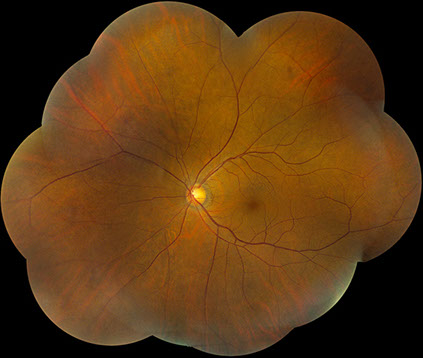
Figures 1A – D: Color fundus photographs of the right (A and B) and left (C and D) eyes. The posterior segment of the right eye has optic nerve hyperemia and a few small dot-blot hemorrhages in the macula (A) and very mild venous dilation with several larger retinal hemorrhages in the temporal and inferior mid-periphery (B). The left fundus shows mild venous dilation(C and D).
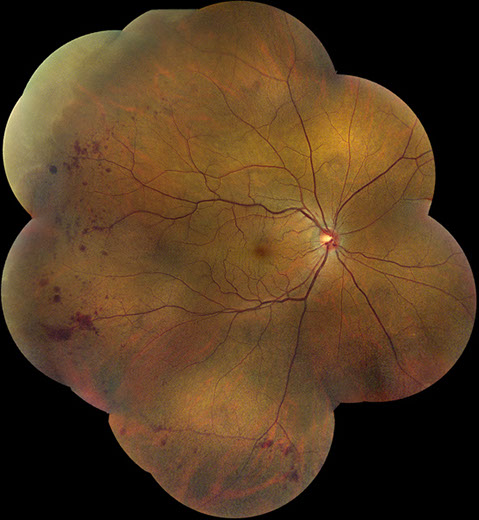
B
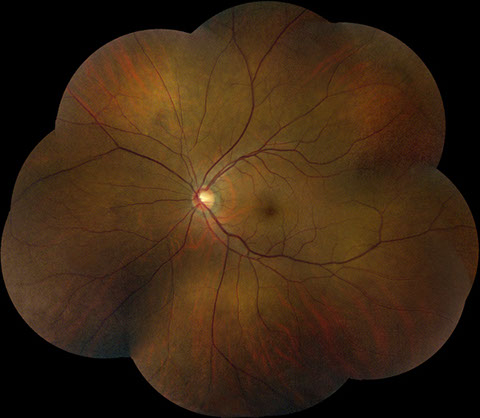
D
Case History:
A 57 year-old Asian man was referred for evaluation of retinal hemorrhages in the mid-periphery of the right eye. The patient denied any decreased vision, pain, or other ocular symptoms. His past ocular, family, and social history were all noncontributory. His only medications were alendronate, glucosamine, calcium, vitamin D, and low-dose aspirin.
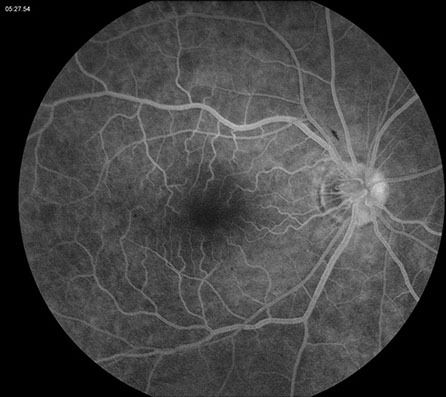
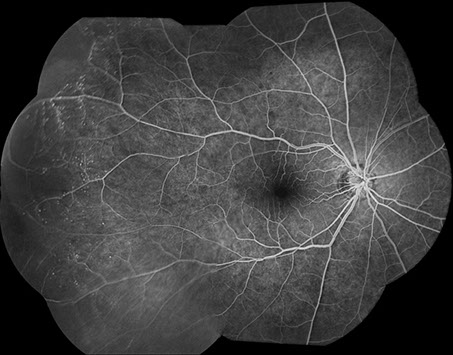
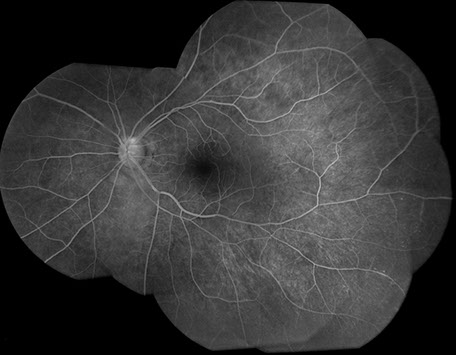
On examination, best-corrected visual acuity was 20/20 bilaterally. Intraocular pressure and anterior segment examination were normal in both eyes. On posterior segment examination of the right eye, there was optic nerve hyperemia and a few small dot-blot hemorrhages in the macula (Figure 1A). There was also very mild dilation but no increased tortuosity of the retinal veins and several larger retinal hemorrhages in the temporal and inferior mid-periphery (Figure 1B). The posterior segment of the left eye showed mild venous dilation (Figures 1C and 1D). Fluorescein angiography (FA) of the right eye was significant for spots of hypofluorescence in the macula and temporal and inferior retinal periphery corresponding to blockage from the scattered retinal hemorrhages and peripheral nonperfusion along with several small microaneurysms temporally (Figures 2A – 2C). FA of the left eye was unremarkable (Figure 2D).
What is your Diagnosis?
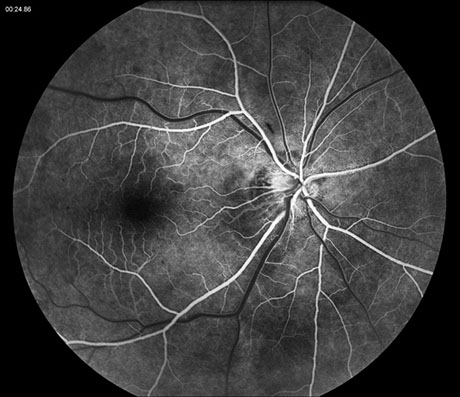
A
B

C

D
Figures 2A – D: Fluorescein angiogram (FA) of the right (A – C) and left (D) eyes. The right eye demonstrates spots of hypofluorescence in the macula (A and B) and temporal and inferior retinal periphery (C) corresponding to blockage from the scattered retinal hemorrhages and peripheral nonperfusion along with several small microaneurysms temporally (C). The left eye is normal (D).
Differential Diagnosis:
The differential diagnosis of retinal venous dilation with peripheral hemorrhages is broad. In addition to retinal vein occlusion and ocular ischemia due to carotid artery disease, conditions that may cause serum hyperviscosity can lead to such retinal changes. These include monoclonal gammopathies like Waldenstrom’s macroglobulinemia, multiple myeloma, primary systemic amyloidosis, and monoclonal gammopathy of undetermined significance. Other conditions causing serum hyperviscosity are polycythemia, essential thrombocytosis, leukemia, and polyclonal gammopathies, such as chronic liver disease, rheumatoid arthritis, systemic lupus erythematosus, and Sjogren’s syndrome. The retinopathy associated with hyperviscosity typically consists of retinal venous dilation, increased venous tortuosity, retinal hemorrhages, and retinal and optic disc edema.
A

C
B
Figures 3A – C: Color fundus photographs at 32 months of follow-up of the right (A and B) and left (C) eyes. The right fundus has persistent venous dilation but a decrease in the number of peripheral retinal hemorrhages (A). There is a small collateral vessel at the optic nerve (B). The posterior segment of the left eye is unremarkable (C).
Additional Case History and Clinical Course:
Past medical history withheld for the purpose of discussion was that our patient had a known diagnosis of Waldenstrom’s macroglobulinemia with increased production of IgM. At presentation, his serum viscosity was 2.4 cP and his IgM level was 4200 mg/dl.
On all of the patients’ subsequent follow-up examinations, the visual acuity remained stable at 20/20 bilaterally. At 32 months of follow-up, the right eye posterior segment still had venous dilation but the peripheral retinal hemorrhages had decreased in number. (Figure 3A). A small collateral vessel was also visible at the optic nerve (Figure 3B). The posterior segment of the left eye was unremarkable (Figure 3C). Fluorescein angiography at this follow-up visit displayed less hypofluorescence from blockage but increased peripheral nonperfusion and microaneurysms temporally (Figure 4A). FA in the left eye revealed a lesser degree of peripheral nonperfusion and microaneurysms temporally (Figure 4B). Serum viscosity at this time was 2.6cP and his IgM level was 4700mg/dl.
Approximately 4 years after his initial visit, the patient began treatment of his Waldenstrom’s macroglobulinemia due to anemia, fatigue, and body aches. He had 5 treatments with rituximab along with plasmapheresis at variable intervals. Two years later, he underwent additional treatment with 6 cycles of chemotherapy. This subsequently led to a significant decrease in the patient’s IgM level and normalization of serum viscosity. On the patient’s most recent follow-up examination, approximately 7 years after his initial visit and one year after his completion of chemotherapy, visual acuity measured 20/20 in both eyes, and the venous dilation and peripheral retinal hemorrhages in the right eye had resolved (Figure 5A). The posterior segment of the left eye remained unremarkable (Figure 5B). Serum viscosity at this time was normal at 1.7 cP and his IgM was 1100 mg/dl.
A
B
Figures 4A – B: FA montage of the right (A) and left (B) eyes 32 months after presentation. The right eye displays less hypofluorescence from blockage but increased peripheral nonperfusion and microaneurysms temporally (A). The left eye demonstrates a lesser degree of peripheral nonperfusion and microaneurysms temporally (B).

A
B
Figures 5A – B: Color fundus photographs at the most recent follow-up visit of the right (A) and left (B) eyes, approximately 7 years after presentation, and one year following second round of chemotherapy with normalization of blood counts. The posterior segment of the right eye appears normal as the venous dilation and peripheral retinal hemorrhages have resolved (A). The left fundus remains unremarkable (B).
Discussion:
Waldenstrom’s macroglobulinemia is a B-cell lymphoproliferative disorder with lymphoplasmacytic infiltration of the bone marrow and lymphatic tissue leading to overproduction of the monoclonal immunoglobulin protein IgM. Manifestations of the disease are secondary to infiltration of the bone marrow and extramedullary sites and elevated serum levels of IgM, and include pancytopenia, organomegaly, neuropathy, and effects of serum hyperviscosity.1 Serum hyperviscosity can also lead to the hyperviscosity syndrome, which may cause fatigue, weight loss, neurological symptoms, epistaxis, gastrointestinal hemorrhages, congestive heart failure, and retinopathy.2
In Waldenstrom’s macroglobulinemia, the increase in serum viscosity leads to microvascular sludging with decreased blood flow to the retina and increased intravascular pressure within the retinal venous circulation. As a result, hyperviscosity-related retinopathy may develop. This consists of retinal venous dilation and beading, increased venous tortuosity, peripheral and central retinal hemorrhages, retinal and optic disc edema, and retinal vascular occlusions.2,3 If severe, visual acuity can be affected. A study of 46 patients with Waldenstrom’s macroglobulinemia evaluated the correlation between retinal changes and serum IgM and viscosity levels. They found that signs of retinopathy, such as retinal hemorrhages and venous dilation, occurred at wide ranges of serum IgM and viscosity levels. However, the severity of retinopathy generally worsened as levels of serum IgM and viscosity increased.2
In addition to the typical findings of retinopathy secondary to hyperviscosity, patients with Waldenstrom’s macroglobulinemia may also present with serous macular detachments. Baker et al described 8 eyes of 4 patients with Waldenstrom’s macroglobulinemia and hyperviscosity syndrome who developed serous macular detachments.4 There was a lack of leakage on fluorescein angiography in all eyes, making the pathologic mechanism for this serous detachment unclear. A hypothesis was that intraretinal IgM accumulates in cystoid macular edema, which then migrates to the subretinal space through focal outer retinal defects. The accumulation of high-molecular weight IgM molecules in the subretinal space theoretically leads to an osmotic gradient. This, in turn, causes fluid transudation from intraretinal edema into the subretinal space. The visual prognosis for eyes with serous macular detachments is guarded. In this case series, the majority of these eyes had persistent subretinal fluid despite systemic treatment.4
Treatment of Waldenstrom’s macroglobulinemia is complex and involves chemotherapeutic drugs and possible stem cell transplant. Plasmapheresis is used to treat the hyperviscosity.1 In a study by Menke et al, 9 patients with hyperviscosity syndrome and retinopathy secondary to Waldenstrom’s macroglobulinemia were evaluated for their response to plasmapheresis.5 Serum IgM and viscosity levels decreased after plasmapheresis. This led to improvement in the severity of retinopathy in all patients as well. In addition, hemodynamic measurements showed significant reduction in venous diameter with accompanying increased venous blood speed.5
Take Home Points:
- Waldenstrom’s macroglobulinemia is a B-cell lymphoproliferative disorder characterized by overproduction of IgM.
- Serum hyperviscosity in Waldenstrom’s macroglobulinemia can lead to retinopathy, with retinal venous dilation, increased venous tortuosity, retinal hemorrhages, optic disc edema, and serous macular detachments.
- Systemic treatment with plasmapheresis can lead to reduction in serum viscosity and improvement in the severity of retinopathy
Want to Subscribe to Case of the Month?
References:
- Agarwal A. Gass’ Atlas of Macula Disease, 5th ed. Elsevier; 2012. Pg 192-193.
- Menke MN, Feke GT, McMeel JW, et al. Hyperviscosity-related retinopathy in Waldenstrom macroglobulinemia. Arch Ophthalmol. 2006;124:1601-6.
- Agarwal A. Gass’ Atlas of Macula Disease, 5th ed. Elsevier; 2012. Pg 608.
- Baker PS, Garg SJ, Fineman MS, et al. Serous macular detachment in Waldenstrom macroglobulinemia: a report of four cases. Am J Ophthalmol. 2013;155:448-55.
- Menke MN, Feke GT, McMeel JW, et al. Effect of plasmapharesis on hyperviscosity-related retinopathy and retinal hemodynamics in patients with Waldenstrom’s macroglobulinemia. Ivest Ophthalmol Vis Sci. 2008;49:1157-60.