West Coast Retina
Case of the Month
September, 2009
A 66 year-old white man presented with a four-month history of bilateral central scotomas and sudden decrease of vision in the left eye.
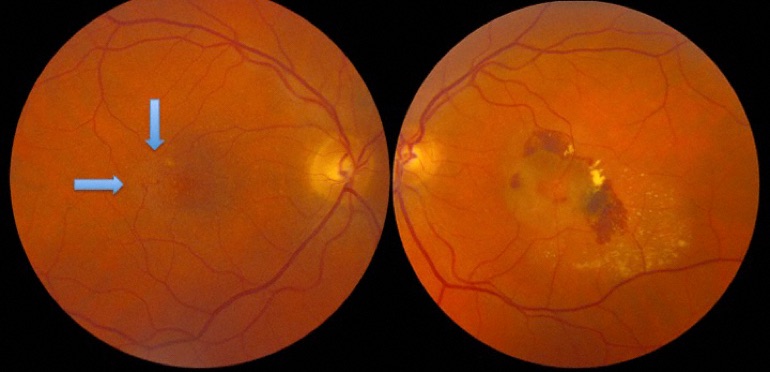
Figure 1: Color fundus photograph of the right and left eye. Note the subtle retinal graying in the temporal macula as well as the right-angled venules (arrows). In the left eye, subretinal hemorrhage, exudate and serous fluid is present in the macula
Case History
A 66 year-old white man presented with a four-month history of bilateral central scotomas and sudden decrease of vision in the left eye. His medical history is notable for hypertension for which he is taking hydrocholorthiazide and verapamil.
On examination, his best-corrected visual acuity (BCVA) was 20/25 in the right eye and 20/200 in the left eye. His IOP was 15 mmHg bilaterally. Dilated posterior segment examination of the right eye showed a subtle graying of the retina on the temporal edge of the fovea and right-angle venules temporal to the foveola (Figure 1, arrows). The left eye showed an area of subretinal hemorrhage, fluid, and exudate (Figure 1).
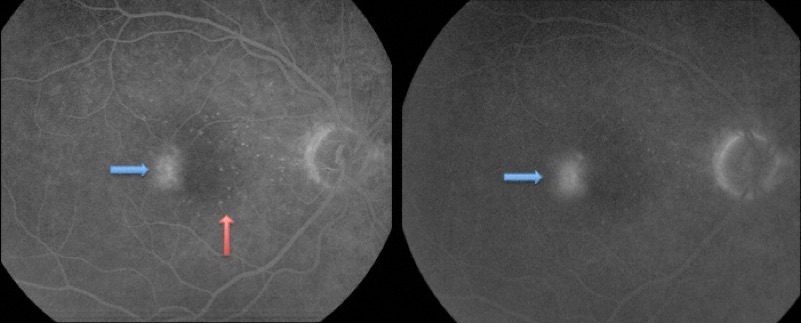
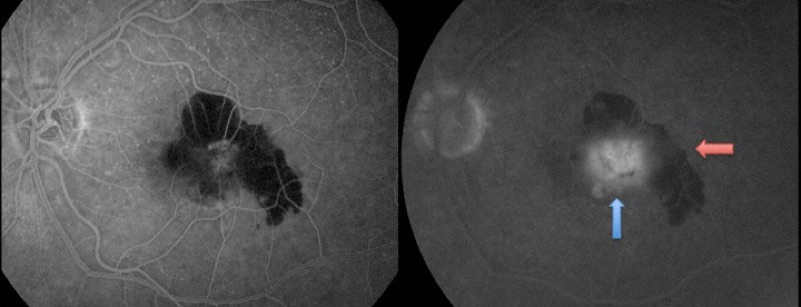
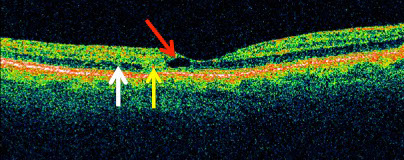
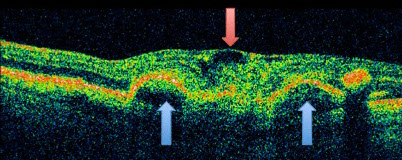
Fluorescein angiography (FA) of the right eye showed leakage temporal to the foveola (Fig 2, blue arrow) and some punctate staining of the drusenoid deposits (Figure 2, red arrow). In the left eye, there was hyperfluoresence with late leakage involving the fovea (Figure 3, blue arrow) with surrounding blockage from subretinal hemorrhage (Figure 3, red arrow). Optical coherence tomography (OCT) of the right eye revealed an inner lamellar cyst (Figure 4). In the left eye, there was evidence of retinal edema, intraretinal cysts, and pigment epithelial detachment (PED) (Figure 4).
A
B
Figures 2A and B: Early and late phase fluorescein angiograms of right eye showing punctate hyperfluorescence nasally due to small drusen deposits. (red arrow) Typical of this disorder is the temporal hyperfluorescence (blue arrows) that increases mildly on the late phase of the angiogram.
A
B
Figure 3A and B: Early and late phase fluorescein angiogram of the left eye showing mostly blocked fluorescence early due to the subretinal hemorrhage. The late phase of the angiogram shows progressive leakage (hyperflourescence, blue arrow) and blocked fluorescence due to the hemorrhage (red arrow).
A
B
Figures 4A: Optical coherence tomography of the right eye shows thinning of the central fovea and an intraretinal cyst (red arrow). Note the loss of the outer retinal layers (yellow arrow) as compared to the intact area (white arrow). This would correspond to the scotoma the patient reported. The OCT study of the left eye shows a thickened retina due to intraretinal edema (red arrow) and subretinal hemorrhage. Note the pigment epithelial detachments (blue arrows).
What is your Diagnosis?
Differential Diagnosis
The findings in the left eye are typical for choroidal neovascularization, given the history and age of this patient. Presence of subretinal hemorrhage, subretinal fluid and exudate with fluorescein angiography showing late hyperfluorescence and leakage are consistent with choroidal neovascularization. The findings in the right eye while subtle, are also very classic for the underlying cause of this patients disease. The presence of dilated retinal vessels with late retinal vascular leakage requires consideration of branch vein occlusion or other causes such as diabetic or radiation retinopathy. The presence of the right angle venules is classic for idiopathic macular telangiectasis (Fig 5)

Figure 5:
This closer view of the right macula reveals the typical right angled venules (blue arrows) assoicated with idiopathic macular telangiectasis. A more subtle finding is the graying of the retina in the temporal portion of the fovea.
Diagnosis
This patient has the classic findings of IJT which include graying of the retina (loss of retinal transparency) in the juxtafoveolar area, right-angle retinal venules, and capillary dilation with leakage on FA. In his left eye, the patient developed subretinal neovascularization as a complication of the disease process.
Treatment
The patient was started on intravitreal anti-vascular endothelial growth factor (VEGF) treatment in the left eye. On the most recent follow-up, after one intravitreal anti-VEGF (Lucentis) injection, his vision improved to 20/125 with significant reduction of retinal edema, intraretinal cystic changes, and PED on OCT.
Discussion
Idiopathic juxtafoveolar retinal telangiectasis (IJT) was first described by Gass and Oyakawa in 1982 as a unilateral or bilateral disease associated with incompetent retinal capillaries in the perifoveal or juxtafoveal area,. The initial classification was largely based on clinical examination, fluorescein angiography, and histopathology (Table 1). Recent advances in OCT provided better understanding of the nature of the vascular abnormalities in IJT. Yannuzzi and colleges revised the term to idiopathic macular telangiectasia and simplified the Gass classification (Table 1).
Retinal findings can be categorized into 3 groups. Group (or Type) 1 present with primarily unilateral disease and aneurysmal telangiectatic vessels. Aneurysmal involvement of capillaries, venules and arterioles is seen. These vessels typically show significant leakage, and cause retinal edema and exudates. Group (or Type) 2 is more common and is bilateral, and typically involve older individuals. A loss of retinal transparency producing a grayish perifoveal area is common. Early, this can be subtle and involve only the temporal portion of the fovea. The perifoveal vessels are most commonly involved in temporal portion. Ophthalmoscopically, the telangiectatic vessels may not be seen but may be seen in more advanced cases. Superficial crystal deposits can occur, as well as hyperplasia of the retinal pigment epithelium. Right angle vessels (arteriolar or venular) are a distinctive finding. Fluorescein angiography shows leakage, but the significant leakage and retinal edema that is associated with Type 1 is not seen. Localized, focal retinal dysfunction is present in these areas of retinal leakage. A late complication can be the development of subretinal neovascularization. A third type, occlusive telangiectasia, is uncommon.
Our patient presented with Gass group 2A IJT or Yannuzzi Type 2 macular telangiectasia. Subtle loss of retinal transparency (a gray hue) is present in the temporal portion of the retina (Fig 1). Also seen are right-angle venules (Figure 1 and 5). The left eye developed subretinal neovascularization that is a late occurrence in some individuals. The characteristic temporal leakage on fluorescein angiography was present in our patient (Fig. 2)
OCT imaging has expanded our understanding of this disorder. Our patient demonstrates some of the characteristic findings. An intraretinal cyst is present in the right eye. This commonly enlarges over time. Also seen in our patient was atrophy of the outer retinal layers (Fig 4).
The visual acuity is typically 20/30 or better when the patients initially seek medical attention. There is no proven treatment for the vision loss associated with type 2 macular telangiectasis. However, the subretinal neovascularization that occasionally complicates this disorder usually responds favorably to anti-VEGF treatment.
Table 1: Idiopathic Juxtafoveal Telangiectasis. Gass vs. Yannuzzi Classification
Yannuzzi Classification
Type 1: aneurysmal telangiectasia of capillaries and venules.
Gass Classification
Group 1A: unilateral, congential, telangiectatic capillaries temporal to the fovea
Group 1B: unilateral, idiopathic, telangiectasis next to the foveal avascular zone
Group 2A: bilateral idiopathic, acquired parafoveolar telangiectasis with retinal thickening temporal to the fovea, right-angle venules, retinal pigment epithelial hyperplastic plaques, subretinal neovascularization, and crystalline deposits
Group 2B: juvenile occult familial JXT
Type 2: Perifoveal telangiectasia
Group 3A: occlusive JXT with visual loss due to obliteration of perifoveal capillaries
Group 3B: occlusive JXT associated with central nervous system vasculopathy
Type 3: Occlusive telangiectasia
Take Home Points
Idiopathic juxtafoveolar retinal telangiectasis (IJT), also known as idiopathic macular telangiectasia, is a unilateral or bilateral disease associated with incompetent retinal capillaries in the juxtafoveal area.
Group 2A or type 2 macular telangiectasia is the most common form with clinical findings of graying of the retina, glistening white deposits in the superficial retina, and right-angle venules.
Fluorescein angiography shows capillary dilatation in the juxtafoveal region. OCT demonstrates characteristic inner lamellar cystic changes with preservation of the internal limiting membrane.
Choroidal neovascularization may develop as a complication and responds to anti-VEGF treatment.
Want to Subscribe to Case of the Month?
References
- Gass JD. Stereoscopic Atlas of Macular Diseases: Diagnosis and Treatment, 4th Ed. CV Mosby, June, 1999.
- Gass JD, Owakawa RT. Idiopathic juxtafoveolar retinal telangiectasis. Arch Ophthalmol. 1982;100:769-780.
- Yannuzzi, LA, Bardal, AMC, Freund, B, et al: Idiopathic Macular Telangiectasia Arch Ophthalmol. 2006;124:450-460.