West Coast Retina
Case of the Month
September, 2011
A 40-year-old male with new onset floaters in his left eye.
Presented by Paul Stewart, MD


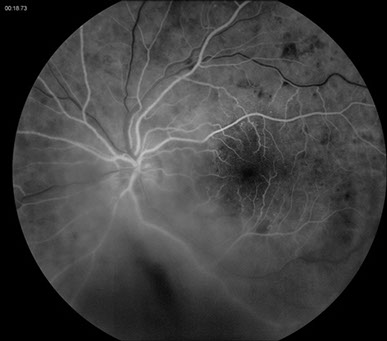
Figure 1: Fundus photograph of the right eye showing widely scattered retinal hemorrhages, with multiple white-centered hemorrhages, and cotton-wool spots in the posterior pole. In the left eye, a vitreous hemorrhage is present inferiorly. Similar retinal vascular changes are noted as seen in the right eye.

Case History
A 40-year year-old male was referred for possible retinal detachment after he became acutely aware of floaters in his left eye and blurred vision. His past ocular history was unremarkable. His past medical history included high blood pressure and he takes a baby aspirin daily. He had a medical exam and blood work done three months ago that was normal except for elevated cholesterol.
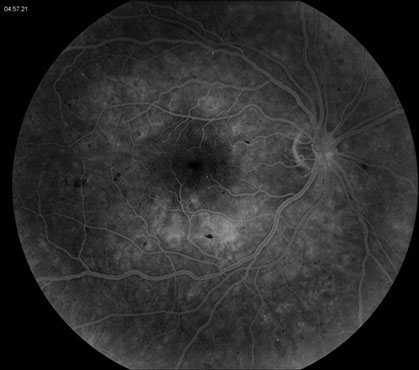
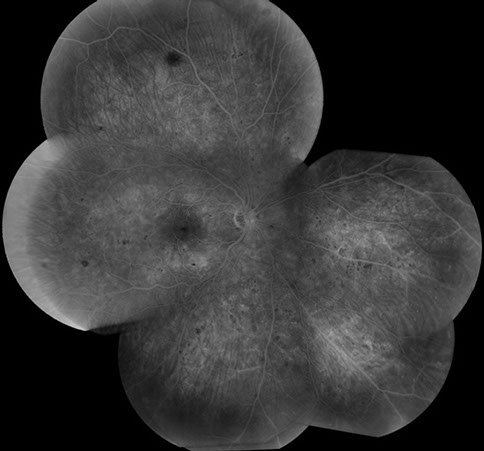
On examination, visual acuity was 20/13 in the right eye and 20/20 in the left eye. Intraocular pressure and the anterior segment examination were normal in both eyes. The blood pressure was 132/83. Visual fields were full in both eyes. The dilated fundus examination of the right eye revealed widely scattered retinal hemorrhages, cotton wool spots, microaneurysms, and some white-centered hemorrhages (Figure 1). The dilated fundus examination of the left eye revealed vitreous hemorrhage inferonasally with preretinal heme. In this eye as well, there were widely scattered retinal hemorrhages, cotton wool spots, microaneurysms and some hemorrhages with white centers (Figure 1). Fluorescein angiography showed some blockage from the vitreous hemorrhage in the left eye as well as the retinal vascular changes with multiple microaneurysms (Figure 2). Similar retinal vascular disease was seen on the fluorescein angiogram of the right eye (Figure 3).

Figures 2: Fluorescein angiogram of the left eye. Blocked fluorescence is seen inferiorly due to vitreous hemorrhage and superiorly due to scattered dot and blot retinal hemorrhages. Note the multiple microaneurysms in the macula as well as peripherally.
Figures 3: Fluorescein angiogram right eye. Note the dot and blot hemorrhages and multiple microaneurysms in the macula and peripherally.
What is your Diagnosis?
Differential Diagnosis
The differential diagnosis includes hypertensive retinopathy, diabetes, retinal vascular occlusions, radiation retinopathy, trauma, and blood dyscrasias.
Clinical Course
A careful review of the patient’s medical history was undertaken. He had recently undergone a complete medical evaluation and mild hypertension was noted. He stated that he wasn’t known to be diabetic, and believed himself to be in good health. He did note some fatigue symptoms over the last several months stating that he had more trouble running his usual 3-4 miles during his regular work-outs. He denied any history of radiation treatment, injuries, weight loss, fevers or night sweats. However, given the concern for possible blood dyscrasia, blood work was drawn the day of presentation that showed a significantly elevated white blood cell count of 194.6 K/L. There was mild anemia with hemoglobin of 10.3 g/dL. Platelets were normal at 393 K/L. A peripheral blood smear showed severe leukocytosis with marked left shift with six percent blasts and 41 percent immature granulocytes, consistent with a diagnosis of chronic myelogenous leukemia.
Discussion
A blood dyscrasia is a pathologic condition affecting the cellular elements of the blood. Chronic leukemias are characterized by mature leukocytes. They can be further characterized as having lymphocytic differentiation (chronic lymphocytic leukemia) or granulocytic differentiation (chronic myelogenous leukemia). CML represents a clonal neoplastic proliferation of the myeloid stem cells.
The fundus examination provides an excellent view of the effects of CML throughout the body. The retinal hemorrhages associated with blood dyscrasias can occur in all layers of the retina. Dot-blot hemorrhages in the inner nuclear and outer plexiform layers along with flame-shaped hemorrhages in the nerve fiber layer are the most common.1 White-centered hemorrhages are typically seen with blood dyscrasias and the white center represents either leukemic infiltrate or platelet-fibrin thrombus.2 White-centered hemorrhages can also be seen related to septic emboli, classically in the course of subacute bacterial endocarditis. The description of white-centered hemorrhages is attributed to Moritz Roth in 1872.3
Hemorrhage can also occur under the internal limiting membrane and will occasionally break through into the vitreous. Vitreous hemorrhage can also occur secondary to retinal neovascularization in CML.4 It is probable that the massive increase in white blood cells causes increased viscosity, reduced blood flow, and subsequently retinal ischemia.
Cotton-wool spots, representing infarctions in the nerve fiber layer, are also often seen in blood dyscrasias. They may result from occlusion of a precapillary arteriole by leukemic infiltrate or by platelet-fibrin thrombi.5
Microaneurysms are thought to be related to the increased viscosity caused by the elevated white blood cell count.6 They are often seen in the peripheral retina (Figure 3a), as opposed to the posterior location usually seen in diabetic retinopathy.
The ophthalmologist can often be the first doctor to see a patient with a blood dyscrasia, making it important to recognize the constellation of findings and promptly pursue further testing.
Take Home Points
- Chronic myelogenous leukemia can present with vitreous hemorrhage, intraretinal hemorrhage (often white-centered), cotton-wool spots and microaneurysms.
- Referral for further diagnostic testing should not be delayed and should include a complete blood count with differential and a peripheral blood smear.
Want to Subscribe to Case of the Month?
References
- Rosa RH and Cunningham RD. “Retinopathy of blood dyscrasias.” Duane’s Clinical Ophthalmology. Volume 2, Chp. 18. Tasman W, ed. 2006.
- Duane TD, Osher RH, Green WR. White centered hemorrhages: Their significance. Ophthalmology 1980; 87:66.
- Roth M. Ueber Netzhautaffectionen bei Wundfiebern. Dtsch Z Chim 1872; 1:471-484.
- Huynh TH, Johnson MW, Hackel RE. Bilateral proliferative retinopathy in chronic myelogenous leukemia. Retina. 2007; 27(1): 124-125
- Sharma T, Grewal J, Gupta S, Murray PI. Ophthalmic manifestations of acute leukaemias: the ophthalmologist's role. Eye 2004; 18: 663-672.
- Jampol LM, Goldberg MF, Busse B. Peripheral retinal microaneurysms in chronic leukaemia. Am J Ophthalmol 1975; 80: 242-248.