West Coast Retina
Case of the Month
September, 2014
Presented by Kevin Patel, MD
A 66 year-old man presenting with decreased vision in the left eye

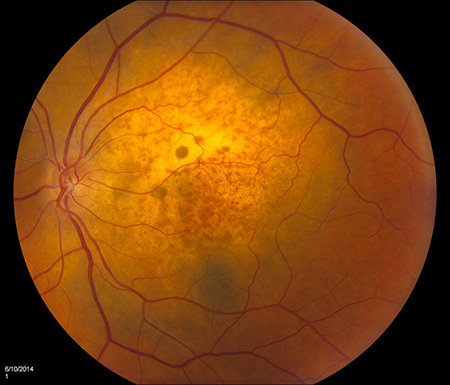
A

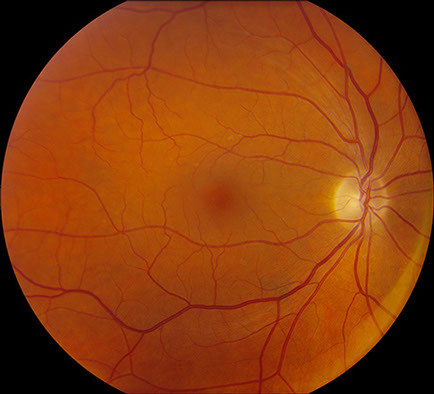
B
Figures 1A and B: Color fundus photographs of the right (A) and left (B) eye. The right eye (A) has only small drusen and mild RPE changes. The left (B) shows an amelanotic choroidal mass in the macula measuring 8 mm x 8 mm in size and extending superiorly from the fovea. There is adjacent subretinal fluid and macular edema as well.
Case History
A 66 year-old Caucasian man presented with decreased vision in the left eye for one week duration. He denied eye pain or any other ocular symptom. There was no significant past ocular history. The patient’s medical history was significant for a hiatal hernia repair, acid reflux, and hay fever.
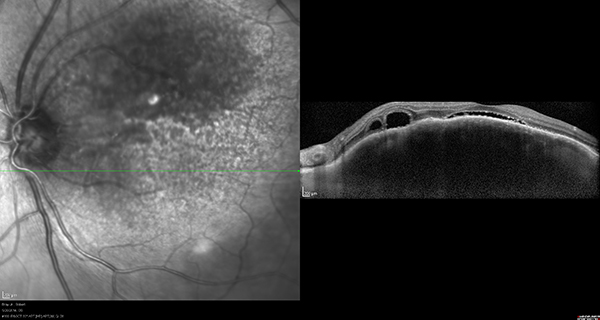
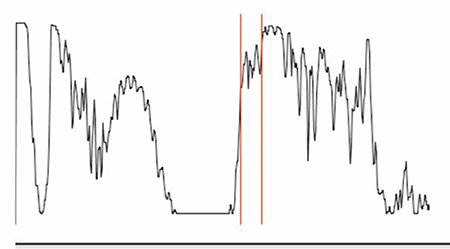
On examination, visual acuity was 20/25 in the right eye and 20/100 in the left eye. Intraocular pressure was normal and anterior segment examination was unremarkable except for mild cataracts in both eyes. Posterior segment examination of the right eye was only remarkable for small drusen and RPE changes in the macula and reticular pigment degeneration in the periphery (Figure 1A). Posterior segment examination of the left eye was significant for an amelanotic choroidal mass in the macula measuring 8 mm x 8 mm in size and extending from the nerve temporally. There was adjacent subretinal fluid and macular edema (Figure 1B). There was also some reticular pigment degeneration in the periphery. Fluorescein angiography was unremarkable for the right eye; in the left eye, it showed irregular early hypofluorescence (Figure 2A) and late hyperfluorescence (Figure 2B) consistent with subretinal fluid and a serous retinal detachment. Optical coherence tomography (OCT) of the macula was normal in the right eye (Figure 3A) but showed thickening of the macula in the left eye with subretinal fluid (Figure 3B). Enhanced depth imaging optical coherence tomography (EDI-OCT) of the left macula revealed additional characteristics of the choroidal mass, including choroidal thickening with shadowing, irregular anterior surface contour, obliteration of the choriocapillaris, and overlying subretinal fluid (Figure 3C). Echography revealed a choroidal mass with a height of 2 mm and medium to high reflectivity (Figure 4A and B).

A
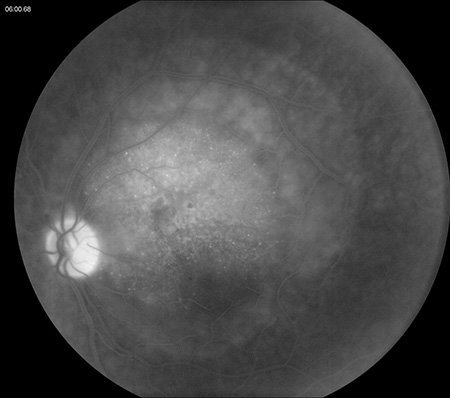
B
Figures 2A and B: Fluorescein angiogram of the left eye showing irregular early hypofluorescence (A) and late hyperfluorescence (B) consistent with subretinal fluid and a serous retinal detachment.
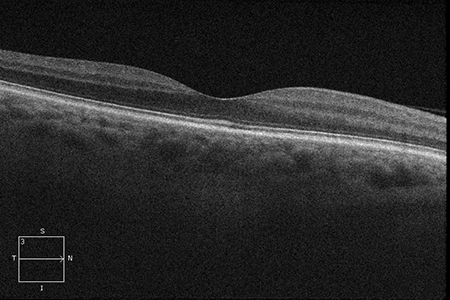
A
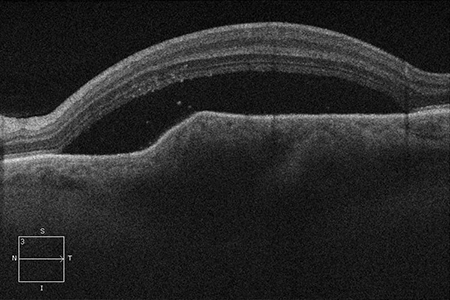
B
C
Figures 3A-C: Optical coherence tomography is unremarkable in the right eye (A). The left eye (B) has thickening of the macula in the left eye with subretinal fluid. Enhanced depth imaging optical coherence tomography of the left eye reveals choroidal thickening with shadowing, irregular anterior surface contour of the mass, obliteration of the choriocapillaris, and overlying subretinal fluid (C).
A
Figures 4A and B: Echography of the left eye showing a choroidal mass with a height of 2 mm and medium to high reflectivity
What is your Diagnosis?
B
Differential Diagnosis
The differential diagnosis for a solitary choroidal mass is broad and includes several clinical entities. One major category consists of benign tumors, such as choroidal nevi, melanocytomas, choroidal cavernous hemangiomas, choroidal osteomas, and sclerochoroidal calcification. A second category is malignant tumors, which consists of choroidal malignant melanomas, metastatic carcinomas, and uveal lymphoma. Inflammatory or infectious conditions can also mimic a choroidal mass. These include posterior scleritis and choroidal granulomas, such as can occur in sarcoidosis or tuberculosis.
Additional Case History
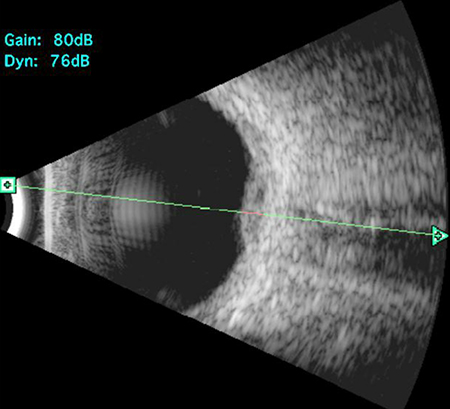
Noteworthy in our patient was a history of cigarette smoking (currently smokes 1 pack/day). Given this history and the amelanotic nature of the lesion, the most likely diagnosis in this case is a choroidal metasisis from lung carcinoma. A systemic workup was subsequently performed to evaluate the patient for a primary malignancy. A CT-scan of the chest revealed a large anterior left upper lobe mass consistent with a neoplasm (Figures 5A and B) and left hilar and mediastinal adenopathy consistent with metastatic spread. A PET-CT scan showed 2 lesions in the upper lobe of the left lung along with multiple metastases to the bone and liver (Figures 6A – C). Chemotherapy was initiated, and 10 days after the first cycle, the choroidal lesion had marked regression. Visual acuity remained decreased at 20/250, but posterior segment examination of the left eye revealed reduction in the size of the amelanotic mass and resolution of the subretinal fluid (Figures 7A and 7B). OCT of the left eye showed absence of subretinal fluid but thinning of the macula with disruption of the IS/OS junction (Figure 8). Echography of the choroidal mass revealed a flat lesion measuring 0.9mm.
A
B
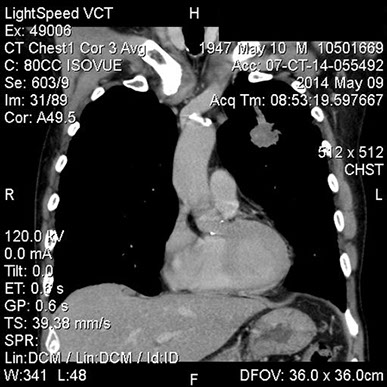
Figures 5A and B: CT-scan of the chest revealing a large anterior left upper lobe mass and hilar adenopathy consistent with a neoplasm.
A
B
C
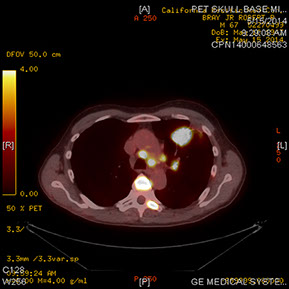
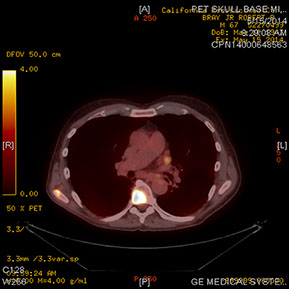
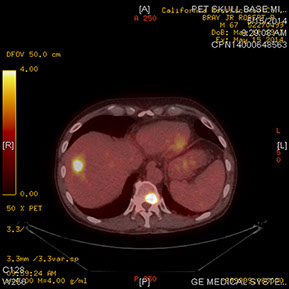
Figures 6A–C: PET-CT scan showing lesions in the upper lobe of the left lung (A) along with multiple metastases to the bone (B) and liver (C)
A

B
Figures 7A and B: Color fundus photographs of the left eye 10 days after chemotherapy was initiated. There is reduction in the size of the mass and resolution of the subretinal fluid and development of a ‘leopard spot’ appearance of the retinal pigment epithelium
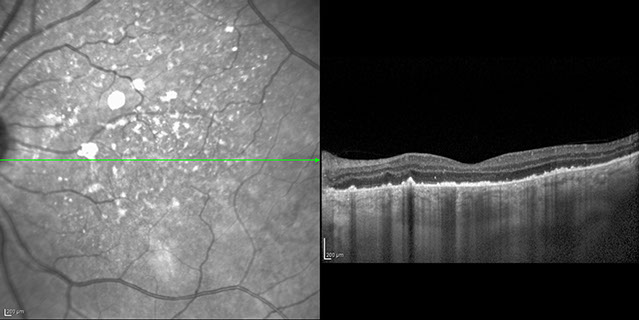
Figure 8: Optical coherence tomography of the left eye showing absence of subretinal fluid but thinning of the macula with disruption of the IS/OS junction.
Discussion
Metastatic carcinoma to the choroid typically presents as a pale white or yellow-white choroidal lesion, often associated with an overlying serous retinal detachment. Metastatic lesions are often mildly elevated (less than 3 mm) as compared to choroidal melanomas. In addition, they may be solitary or consist of multiple lesions in one or both eyes.1,2 Metastatic carcinomas are presumably often located in the macula due this area’s rich blood supply. Fluorescein angiography is not useful in diagnosing metastatic lesions as it usually reveals a nonspecific irregular, widespread area of fluorescein leakage. Echography of metastatic lesions usually reveals medium to high internal reflectivity with an irregular pattern, which is higher than melanomas and can help differentiate these tumors. The use of EDI-OCT in characterizing choroidal masses has provided further insight to diagnostic characteristics of choroidal metastases. In a recent case series, the Shields discussed the imaging features of choroidal metastases in 14 eyes using EDI-OCT.3 Several distinguishing features of choroidal metastases include: irregular anterior tumor surface, choriocapillaris obliteration, choroidal shadowing, presence of subretinal fluid, and preservation of the inner retinal layers.3
When a metastatic lesion to the choroid is a possible diagnostic consideration, a thorough medical history and systemic evaluation should be undertaken to assess for the presence of a primary malignancy. In females, the most common primary source is from breast carcinoma (68%); in males, it is lung carcinoma (40%). Typically, metastases from breast carcinoma occur in the setting of a known primary tumor while in lung carcinoma, the presentation of choroidal metastases frequently precedes the diagnosis of the primary lung tumor.4
In a study by Shields et al, the clinical features, treatment, and outcome of uveal metastases from lung cancer were evaluated.5 A total of 229 eyes of 194 patients had uveal metastases originating from primary lung cancer. The diagnosis of lung cancer preceded that of the uveal metastasis in 109 patients (56%), while 85 patients (44%) had the metastasis diagnosed initially which led to a systemic investigation and subsequent diagnosis of lung cancer. The vast majority of metastases per eye were to the choroid (214, 93%), while the ciliary body (8, 3%) and iris (16, 7%) were far less common. Ninety-seven eyes had subretinal fluid and follow-up data. Of these eyes, the subretinal fluid resolved completely in 47 (48%), resolved partially in 20 (21%), remained unchanged in 17 (18%), and increased in 13 (13%).
Treatment options for eyes with metastatic lesions include: external beam radiation, plaque radiotherapy, systemic chemotherapy, observation, enucleation, or a combination of treatments. Shields et al reported tumor regression in 66%, stable lesions in 12% and progression in 15%. Overall prognosis for patients with uveal metastases from lung cancer is guarded. In this particular study, the mean life expectancy after detection of uveal metastases was 12 months.5
More recent treatment options for choroidal metastases from lung cancer include the use of intravitreal bevacizumab and oral erlotinib. Kim, et al reported a case of a 57-year-old woman with 2 choroidal metastases associated with a serous retinal detachment from non-small-cell lung carcinoma to her left eye.6 Treatment consisting of 3 intravitreal injections of bevacizumab with a 6-week interval between injections and oral erlotinib started 9 weeks after the first injection was initiated. The 2 metastases had completely disappeared and the retinal detachment had resolved one month after the third intravitreal bevacizumab injection. The oral erlotinib had been taken for 2 months at this point.6
Take Home Points
- Metastatic carcinoma to the choroid is a not uncommon complication of certain systemic carcinomas, most often lung carcinoma in males.
- A thorough medical history and systemic evaluation for a primary tumor are essential when metastatic carcinoma is suspected.
- Early diagnosis of the primary carcinoma can lead to prompt and effective treatment of both the primary tumor and choroidal metastasis.
Want to Subscribe to Case of the Month?
References
- Ferry AP, Font RL. Carcinoma metastatic to the eye and orbit. I. A clinicopathologic study of 227 cases. Arch Ophthalmology 1974;92:276-86.
- Gonvers M, Zografos L. Choroidal metastasis and rhegmatogenous retinal detachment. Retina. 1991;11:426-9.
- Al-Dahmash SA, Shields CL, Kaliki S, et al. Enhanced depth imaging optical coherence tomography of choroidal metastasis in 14 eyes. Retina. 2014;34:1588-93.
- Shields CL, Shields JA, Gross NE, et al. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104:1265-76.
- Shah SU, Mashayekhi A, Shields CL, et al. Uveal metastasis from lung cancer: clinical features, treatment, and outcome in 194 patients. Ophthalmology. 2014;121:352-7.
- Kim SW, Kim MJ, Huh K, et al. Complete regression of choroidal metastasis secondary to non-small-cell lung cancer with intravitreal bevacizumab and oral erlotinib combination therapy. Ophthalmologica. 2009;223:411-3.