West Coast Retina
Case of the Month
Sept, 2015
Presented by Ananda Kalevar, MD
An 83 year-old man presents with recent onset of blurred vision in his right eye.

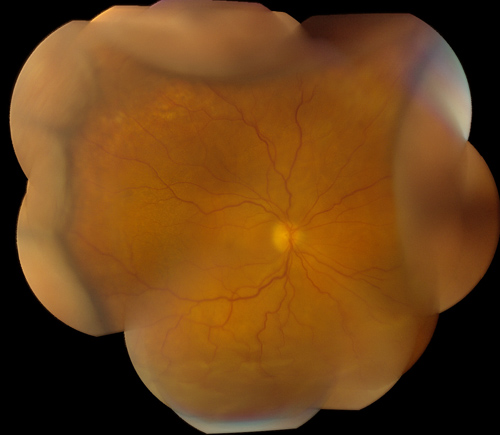
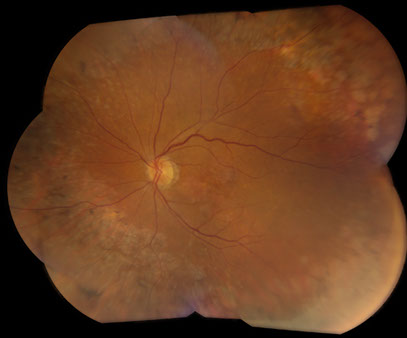
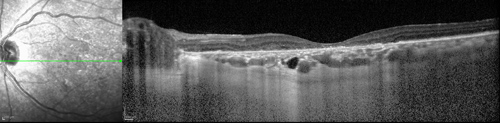
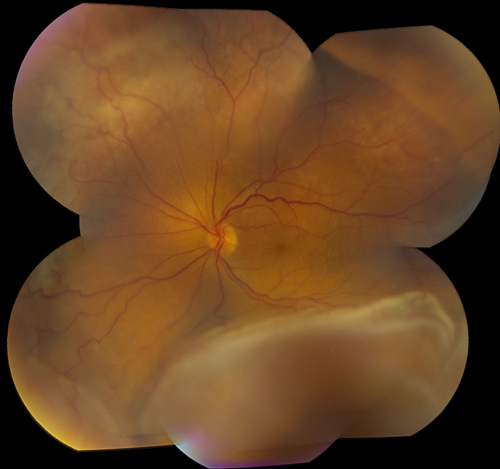
Figures 1 and 2: Color fundus photograph montages of the right and left eyes. Choroidal and retinal detachment is present in the right eye. Note the extensive retinal pigment epithelial changes in the left eye producing a ‘leopard-spot’ pigmentation.
Case History
An 83 year-old man presents with a two-month history of blurred vision in the right eye. His past ocular history was relevant for a serous choroidal detachment 8 years earlier in his left eye. He is pseudophakic bilaterally with a sensory exotropia in the left eye.
His medical history was relevant for chronic obstructive pulmonary disease and iron deficiency anemia. He was taking the following medications: ferrous sulfate, metoprolol, pantoprazole, spiriva, vitamin D, and simvastatin. The patient’s family and social history were non-contributory.
On examination, best-corrected visual acuity was 20/250 and hand motion in the right and left eye, respectively. Intraocular pressure was 12 and 11 in the right and left eye, respectively. The anterior segment examination was remarkable and revealed no inflammation. The posterior segment exam of the right eye showed peripheral choroidal detachment for 360° with an inferior serous retinal detachment (Figure 1). Examination of the left posterior segment demonstrated prominent 360° peripheral leopard-spot retinal hyperpigmentation (Figure 2). The OCT of the right eye showed subretinal and intraretinal fluid. The OCT of the left eye showed significant atrophy of the outer retinal layers, retinal pigment epithelium and choriocapillaris (Figure 3A and B). The B-scan ultrasound of the right eye demonstrated a serous choroidal detachment with an accompanying inferior retinal detachment (Figure 4). B-scan ultrasound of the left eye showed no evidence of choroidal or retinal detachment. Figure 5 shows the appearance of his left eye 8 years earlier.
Figures 3A and B: OCT-SD of the right and left eye. Subretinal and intraretinal fluid is present in the right eye, with an undulating thickening of the choroid. The left eye shows substantial atrophy of the outer retina, retinal pigment epithelium and choriocapillaris.
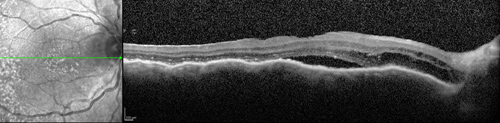
A
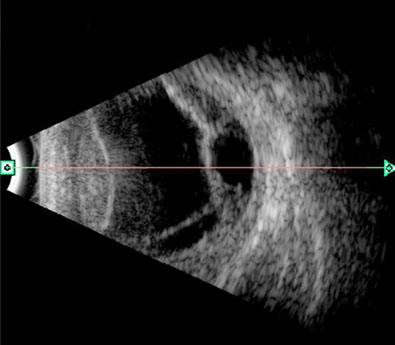
Figure 4: B-Scan ultrasound of the right eye. Serous choroidal and retinal detachment are present
Figure 5: Color montage of the left eye 8 years earlier. Note the choroidal and retinal detachment.
What is your Diagnosis?
B
Differential Diagnosis
This patient had a combined serous choroidal and retinal detachment in the right eye. The differential diagnosis is broad and includes: ocular hypotony (wound leak, retinal detachment, ciliary body dysfunction), dural arterio-venous fistula, malignant hypertension, inflammatory conditions (e.g. following laser or cryopexy, uveitis, idiopathic orbital inflammation), drugs, and neoplastic (lymphoproliferative disorders, bilateral diffuse uveal melanocytic proliferation).
Additional Case History
Two weeks after presentation, scleral windows (sclerectomy and sclerostomy superotemporally and inferotemporally) were done on the right eye. Abnormally thickened sclera was noted at the time of the procedure. No drainage of subretinal fluid was done. A similar procedure had been done on his left eye 8 years earlier.
Two weeks after the procedure on his right eye, vision improved to 20/63 and both the retinal and choroidal detachment had resolved (Figure 6). OCT of the right eye, the subretinal fluid had resolved, with only some mild intraretinal fluid noted (Figure 7).
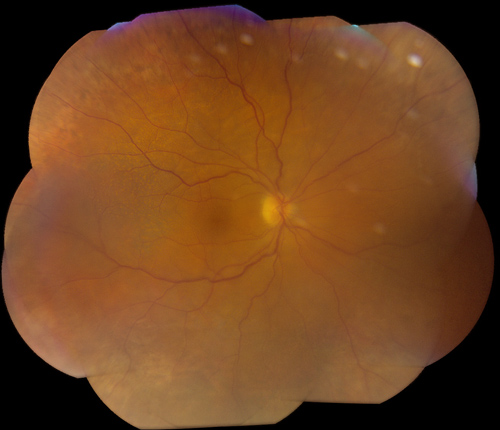
Figure 6: Color montage of the right eye 2 weeks following sclerectomy and scloerostomy procedure. The choroidal and retinal detachment have resolved.
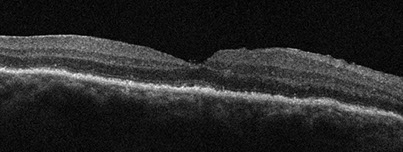
Figure 7: OCT-SD of the right eye 2 weeks following sclerectomy and scloerostomy procedure. The subretinal fluid and choroidal undulations have resolved. Mild intraretinal edema is present
Discussion
Spontaneous exudative detachment of the choroid was first described by Schepens and Brockhurst in 1963.1 In 1982, Gass and Jallow2 first used the term uveal effusion syndrome (UES) to describe an idiopathic serous detachment of the choroid, ciliary body and retina.
UES is a diagnosis of exclusion, with an extensive differential to consider. 2-6 It is a rare entity that is typically seen in middle-aged men. They may suffer from a chronic relapsing course. It is bilateral in up to 65% in published series. UES is classified into two categories; those patients with significant hypermetropia (nanophthalmos) and those without.3-6
Clinically UES patients present with painless vision loss which may be asymmetric. The most prevalent features of the patients are that they have significant choroidal elevation and subretinal fluid with significant secondary retinal pigment epithelial (RPE) damage. The retinal detachment is nonrhegmatogenous, dependant and shifts. The subretinal fluid has a high protein concentration. After resolution of the retinal detachment, spotty pigmentation can be seen that has been termed leopard-spots. Intraocular pressure is normal in UES patients and this is an important finding to exclude hypotony as the cause of choroidal detachment.3-6
The pathophysiology of the choroidal effusions is believed to be secondary to impaired scleral permeability and vortex vein compression. Histologic studies have shown that the collagen fibers of patients with UES have variable diameters, are arranged irregularly with abundant deposition of proteoglycans in the matrix between the bundles. This has been hypothesized as the cause of resistance to transscleral fluid outflow. Subsequently, the altered and thickened sclera may cause compression of the vortex vein producing choroidal venous congestion and fluid accumulation.3-6
There is one primary treatment option that is used for UES patients. It consists of a sclerectomy and sclerotomy (scleral window procedure). Sclerectomies are performed typically in two quadrants of the affected eye and under the scleral flap, a sclerotomy is performed to expose the choroid and promote fluid egress. Most eyes will show reattachment over the following 3-6 months. Some eyes require additional surgery to achieve resolution of the choroidal and retinal detachment. Unfortunately, even with successful surgery and anatomic success, chronic subfoveal RPE changes may limit visual prognosis. Vortex vein decompression, as originally described by Schepens and Brockhurst, has fallen out of favor due to greater risk of complications.3-6
Take Home Points
- Uveal effusion syndrome is a rare entity that occurs most commonly in middle-aged men. It is a diagnosis of exclusion.
- Uveal effusion syndrome is associated with thickened, abnormal scleral that is reasoned to cause reduced scleral permeability and vortex vein compression.
- Treatment consists of a scleral window procedure which has limited visual prognosis.
Want to Subscribe to Case of the Month?
References
- Schepens CL, Brockhurts RJ. Uveal effusion. I. Clinical picture. Arch Ophthalmol 1963; 70: 189-201.
- Gass JDM, Jallow S. Idiopathic serous detachment of the choroid, ciliary body, and retina (uveal effusion syndrome). Ophthalmology 1982; 89: 1018-32.
- Elagouz M, Stanescu-Segall D, Jackson T. Uveal effusion syndrome. Surv Ophthalmol 2010; 55: 134-145.
- Uyama M, Takahashi K, Kozaki J et al. Uveal effusion syndrome. Clinical features, surgical treatment, histologic examination of the sclera and pathophysiology. Ophthalmology 2000; 107: 441-449.
- Ryan S. Retina, 5th ed. 2013: 1306-1317.
- Agarwal A. Gass’ Atlas of Macula Diseases, 5th ed. Elsevier; 2012: 196-202.