April, 2021
Case kindly provided and prepared by:
Drs. Federica Turchi and Antonio Ciardella
Case modified for presentation by Braden Burckhard, MD


Case kindly provided and prepared by:
Drs. Federica Turchi and Antonio Ciardella
Case modified for presentation by Braden Burckhard, MD

A 19 year-old male presented with blurred vision in his right eye for one week.
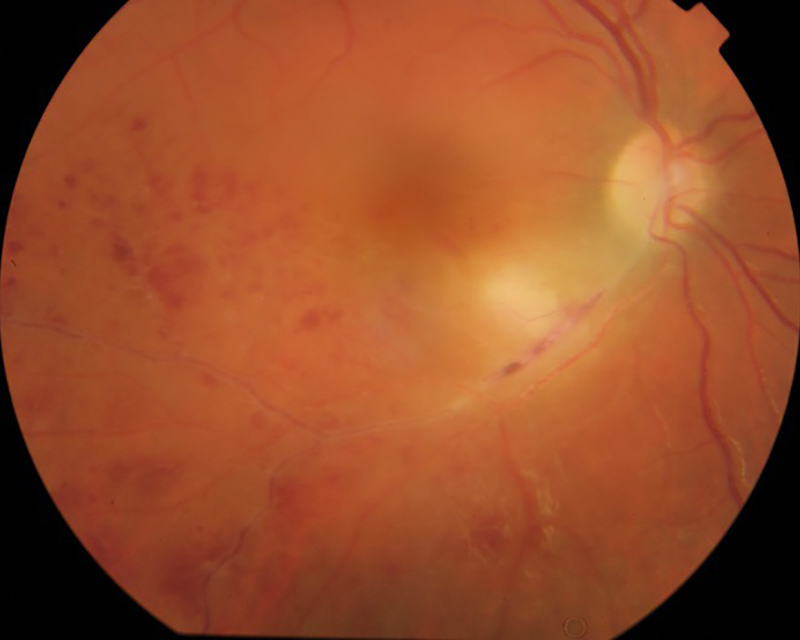
Figure 1A: Color photo of the right eye. Note the area of intense retinal whitening, and scattered retinal hemorrhages in the area of the branch retinal vein occlusion.

Figure 1A: Color photo of the uninvolved normal left eye.
The patient reported blurred vision and floaters beginning one week earlier. His past medical history is noteworthy for an atrioventricular septal defect which was repaired eleven years earlier. He is treated for hypertension. His past ocular history is unremarkable. The patient was born and raised in the Ukrainian countryside for several years, but otherwise his social history was non-contributory.
On examination, his best corrected Snellen visual acuity measured 20/200 in the right eye (OD) and 20/20 in the left eye (OS). His intraocular pressure was 12 mmHg in both eyes. Anterior segment examination showed a mild anterior uveitis OD and was unremarkable OS. The funduscopic examination of the right eye showed vitritis, with an area of intense retinal whitening associated with retinal hemorrhages distal consistent with an inferotemporal branch venous occlusion (Figure 1A). The left eye fundus exam was unremarkable (figure 1B). Spectral domain optical coherence tomography (SD-OCT) showed loss of the photoreceptor inner and outer segments in the macula of the right eye (Figure 2A) and an underlying choroiditis with localized thickening (Figure 2B). Hypofluorescence was noted in the zone of the vitritis and in the area of choroidal thickening on fluorescein angiography as well as delayed filling of the occluded inferotemporal vein, retinal hemorrhages, (Figures 3A-D) and late arteriolar leakage.
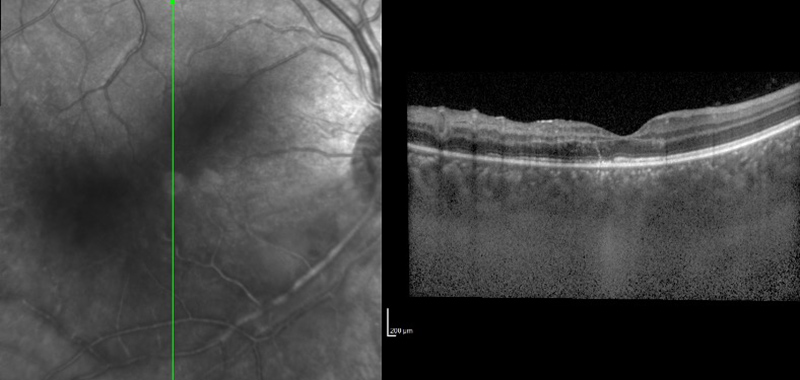
Figure 2A: SD-OCT of the right macula. Note the disruption of the outer retina and photoreceptors.
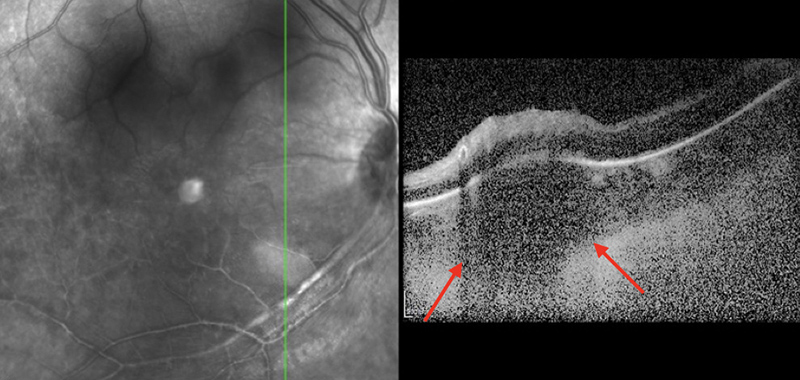
Figure 2B: SD-OCT of the right eye. A vertical scan through the area of retinitis shows a discrete area of chroidal thickening (red arrows) and an overlying area of retinal hyperreflectivity due to the retintis.
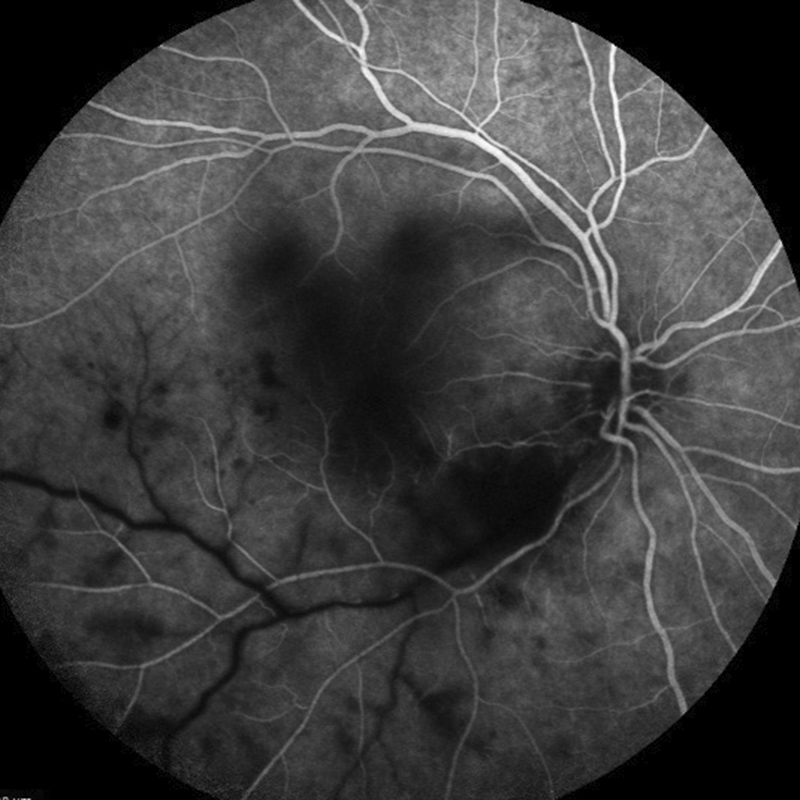
Figure 3A: Flourescein angiogram of the right eye arteriovenous phase. Note the area of hypofluorescence along the inferotemporal arcade in the area of retinitis as well as the delayed filling of the inferotemporal vein.
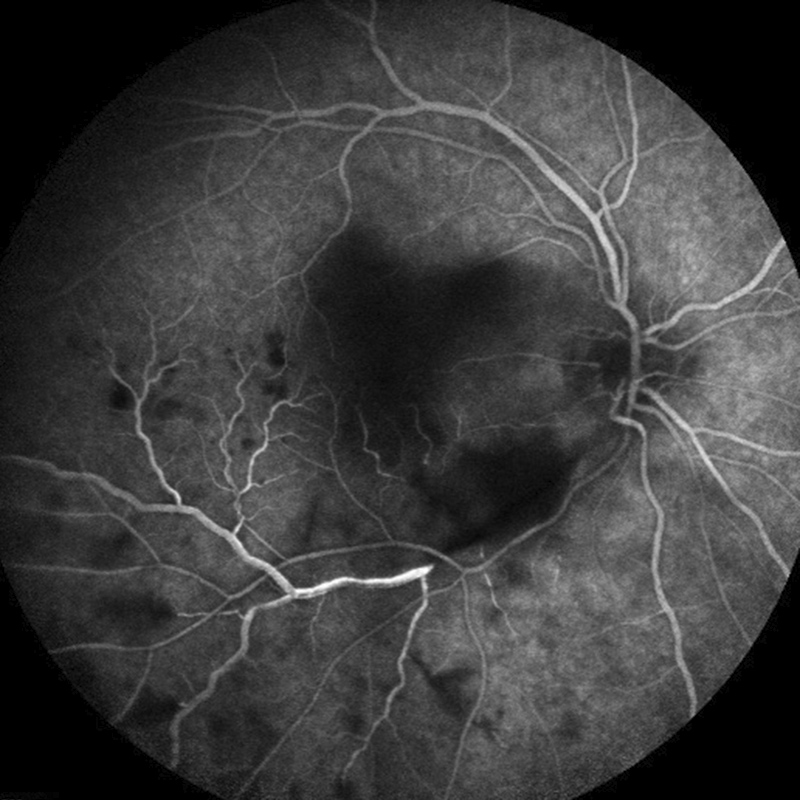
Figure 3B: Flourescein angiogram of the right eye late arteriovenous phase. Note the area of hypofluorescence along the inferotemporal arcade in the area of retinitis.
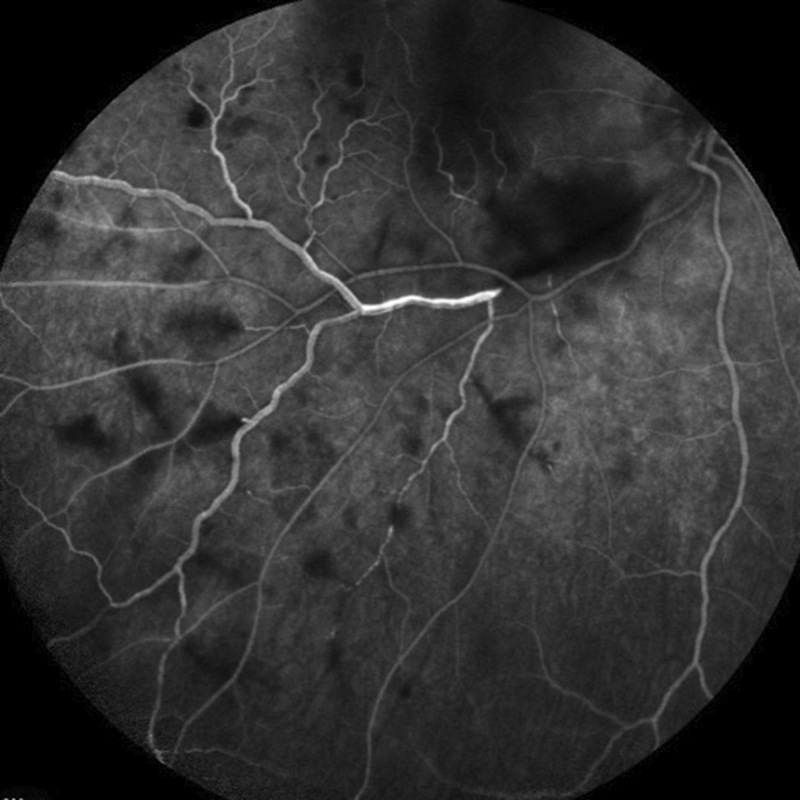
Figure 3C: Flourescein angiogram of the right eye arteriovenous phase. There is staining of the vein and scattered areas of hypofluorescence are present due to retinal hemorrhages.
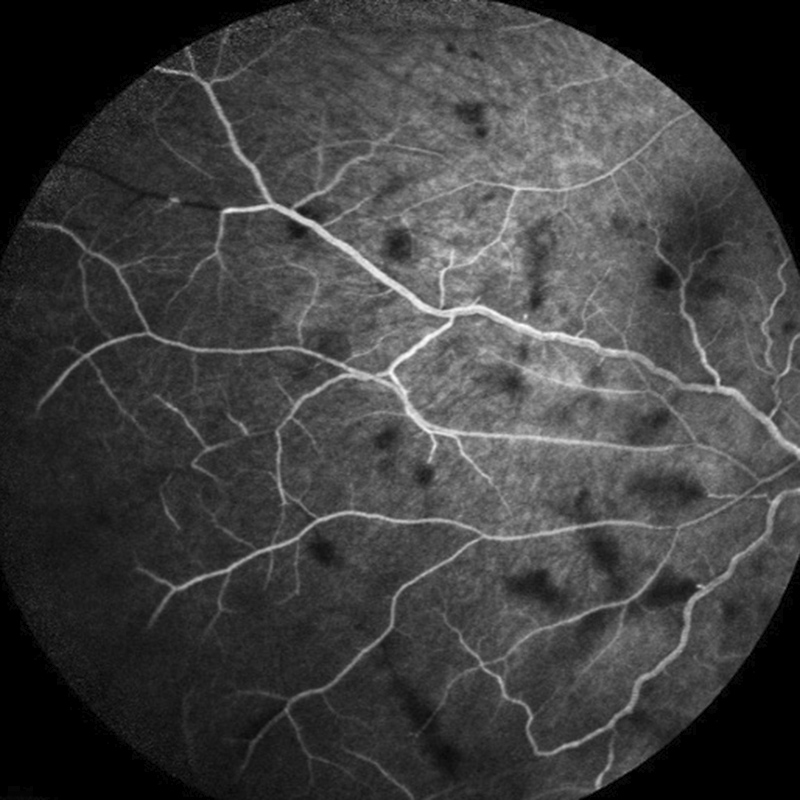
Figure 3D: Flourescein angiogram of the right eye arteriovenous phase. Scattered areas of hypofluorescence are present due to retinal hemorrhages.
Differential Diagnosis
Additional History, Diagnosis and Patient Course
The patient underwent an extensive infectious, inflammatory, and autoimmune evaluation and a chest x-ray. The patient’s serum analysis returned positive only for CMV IgG and toxoplasma IgG. The seroprevalence of toxoplasma gondii infection in the general population is around 42%.1 However, due to the strong suspicion of toxoplasmic retinochoroiditis, the patient underwent a vitreous biopsy and received an intravitreal clindamycin (1 mg/0.1 mL) and dexamethasone (400 μg/0.1 mL) injection. The vitreous biopsy confirmed the diagnosis of toxoplasmosis.
Discussion
The diagnosis of ocular toxoplasmosis is based most often on the presence of characteristic clinical findings, which include focal retinochoroiditis, an adjacent or nearby retinochoroidal scar, and moderate to severe vitreous inflammation.2,3 However, a variety of less common, “atypical” presentations may be unfamiliar to clinicians such as punctate outer retinal toxoplasmosis, retinal vasculitis, retinal vascular occlusions, rhegmatogenous and serous retinal detachments, a unilateral pigmentary retinopathy mimicking retinitis pigmentosa and neuroretinitis.4
T. gondii may cross the vascular endothelium to access human retina by at least three routes: in leukocyte taxis; as a transmigrating tachyzoite; and after infecting endothelial cells. Once in the retina, tachyzoites are capable of migration through the retinal layers, giving them access to any retinal host cell. Although retinal neurons are relatively resistant to infection, tachyzoites readily infect human Müller glial cells, which span across the retina. T. gondii infects the retinal pigment epithelium, inducing a growth factor response that results in the characteristic clinical appearance caused by proliferation of neighboring uninfected cells.5
In our case, the patient also showed a peculiar sign of Kyrielies plaques, or segmental retinal periarteritis which appears as focal or segmental yellowish-white accumulations around retinal arteries, typically near or adjacent to an area of active retinal infection or inflammation (Figure 4A). They are described in different ocular infections but mostly in the toxoplasmosis retinochoroiditis. SD-OCT scans were performed along the segmental Kyrieleis arteritis and hyperreflectivity of the vessel wall was noted (Figure 4B). Kyrielies plaques are characterized by inflammatory involvement within the vessel wall, most likely originating from the endothelium.6

Figure 4A: Fundus photo of the right eye. There is intense retinitis and scattered retinal hemorrhages due to the branche vein occlusion. Note the whitish periarterial (Kyrieleis) plaques along the inferotemporal arteriole.
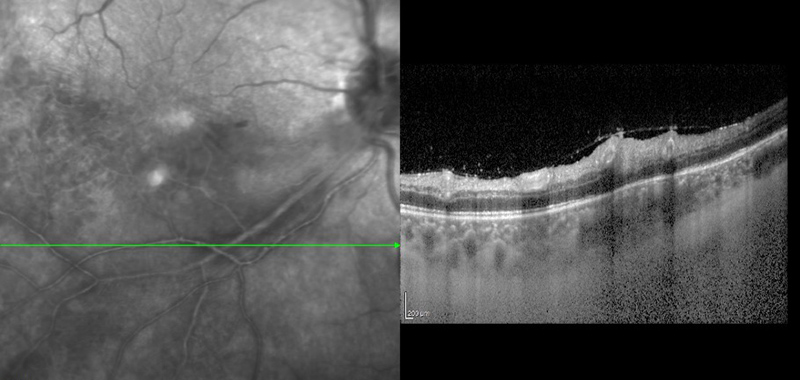
Figure 4B: SD-OCT scan of the right eye through the inferotemporal arcade. Hyper-reflectivity of the arterial wall can be seen in the area of the Kyrieleis plaques.
In the immunocompetent individual, toxoplasmic retinochoroiditis typically resolves over a period of 1 to 2 months. Given the benign natural history and the potential toxicity of antiparasitic medication, treatment of all comers with active infection would result in an unnecessarily high rate of drug-related morbidity. However, a majority of ophthalmologists will treat immunocompetent patients with active inflammation who have: reduced visual acuity; a lesion located within the temporal arcades or adjacent to the optic disc; and/or vitreous haze above grade 1+.2
Current medical options include classic therapy with pyrimethamine, sulfadiazine and systemic corticosteroid or an alternative with trimethoprim-sulfamethoxazole, which has been an increasingly more attractive option for reasons that include low cost, wide availability, and tolerability, although sulfonamide-related reactions may occur. Some studies have shown that patients with ocular toxoplasmosis that involves the macula or optic nerve, is adjacent to a large vessel, or is associated with severe vitritis have a faster resolution of their symptoms with intravitreal injection of clindamycin (1 mg/0.1mL) and dexamethasone (400 μg/0.1mL) than with systemic treatments.3 Therefore, this treatment option was selected in this patient’s care. Four months following intravitreal clindamycin and dexamethasone, as well as two serial aflibercept injections for macular edema, the visual acuity returned to 20/32. The area of retinits was resolved as was the area of choroidal thickening (Figures 5A and B).

Figure 5A:Color photo of the right eye 4 months after presentation. The area of retinitis has resolved, but peripheral features of the branch vein occlusion persist.
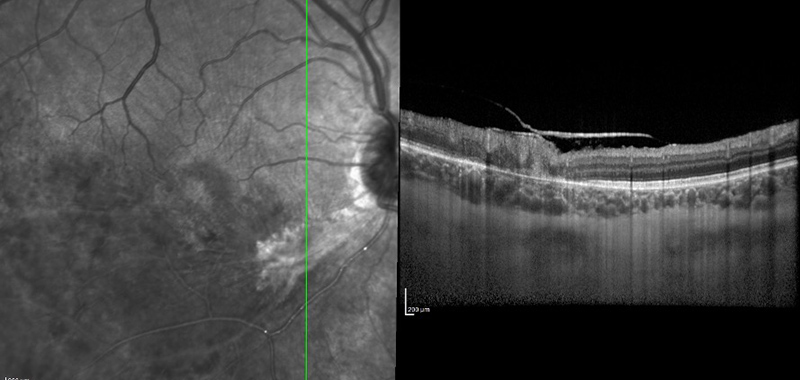
Figure 5B: SD-OCT of the right eye through the inferotemporal arcade. The area of choroidal thickening noted on presentation (Figure 2B) has resolved.