April, 2022
Presented by Malini Veerappan Pasricha, MD


Presented by Malini Veerappan Pasricha, MD

An 82-year-old Asian female presented with new onset blurry vision in her right eye.
Case HistoryThe patient has a history myopic degeneration more significantly in the right eye as compared with the left eye. The myopic degeneration had been stable for several years (Figure 1). She denies any flashes, floaters, or metamorphopsia. Her past medical and family history is significant for hypertension. She denies any trauma to the eye.
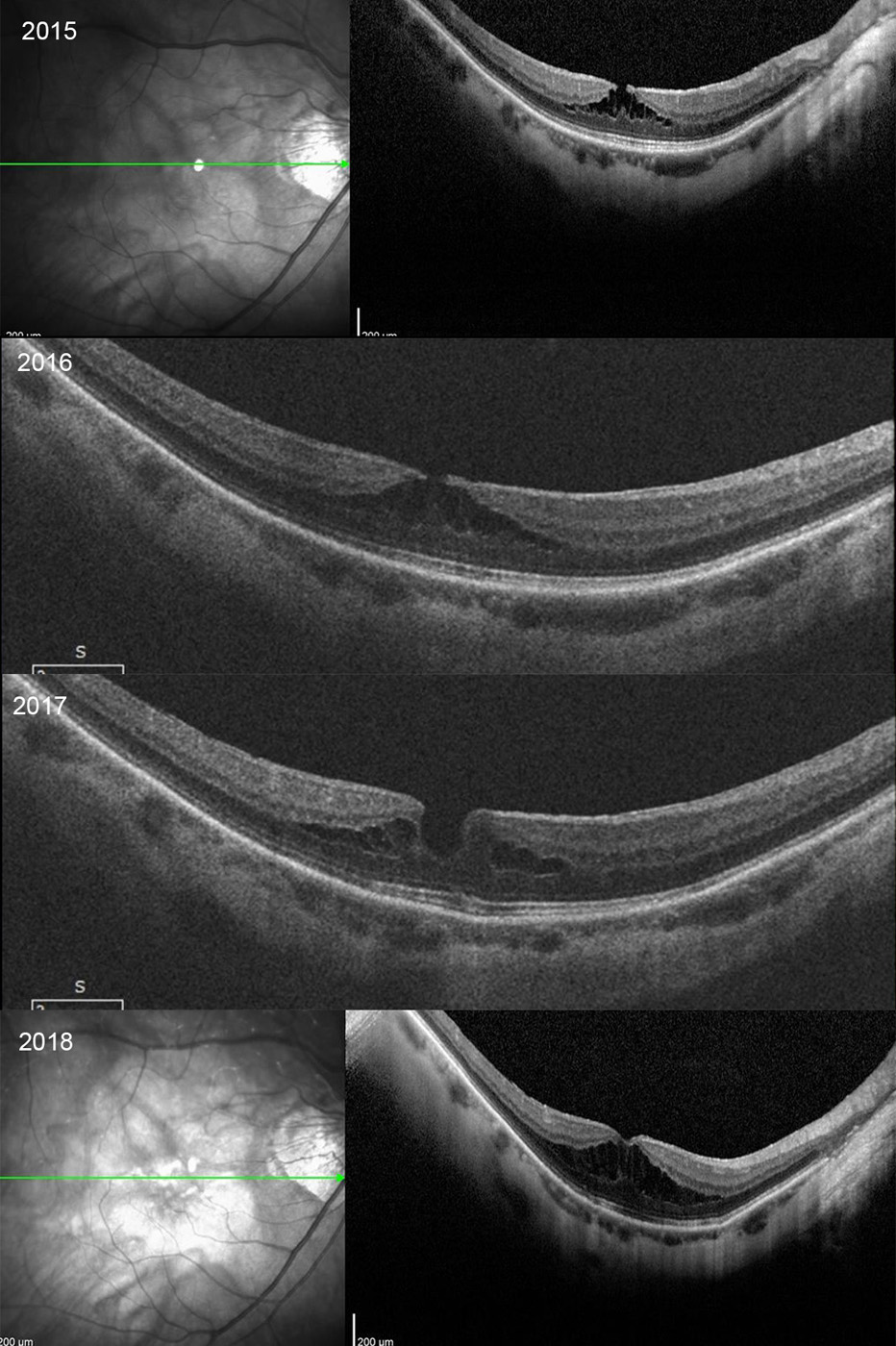
Figure 1: Serial SD-OCT scans from 2015 thru 2018. Myopic related macular schisis changes are present that show mostly stable findings.
Her best corrected Snellen visual acuity measured 20/100 in the right eye (OD) and 20/32 in the left eye (OS). The vision did not improve with pinhole. Her intraocular pressure was 13 mmHg OD and 12 mmHg OS. Anterior segment examination was unremarkable. The posterior examination of both eyes showed peripapillary atrophy, posterior staphyloma, lacquer cracks, lattice degeneration, and likely posterior vitreous detachment. There was no subretinal hemorrhage. Optical coherence tomography (OCT) of the right eye revealed a full thickness macular hole and macular detachment (Figure 2).
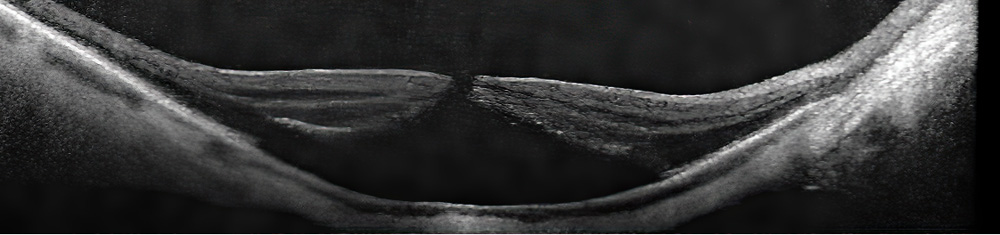
Figure 2: SD-OCT scan of the right macula at the time of presentation with reduced vision. Note the full-thickness macular hole with macular detachment.
The patient has a history of primary open angle glaucoma and has been pseudophakic for several years. Approximately 20 months earlier, she had been started on latanoprost by her glaucoma specialist. An OCT a few months following this, and a later OCT only two months prior to her recent reduction in vision, showed some worsening of the myopic schisis in the right eye (Figure 3). The left eye exam and imaging was stable.
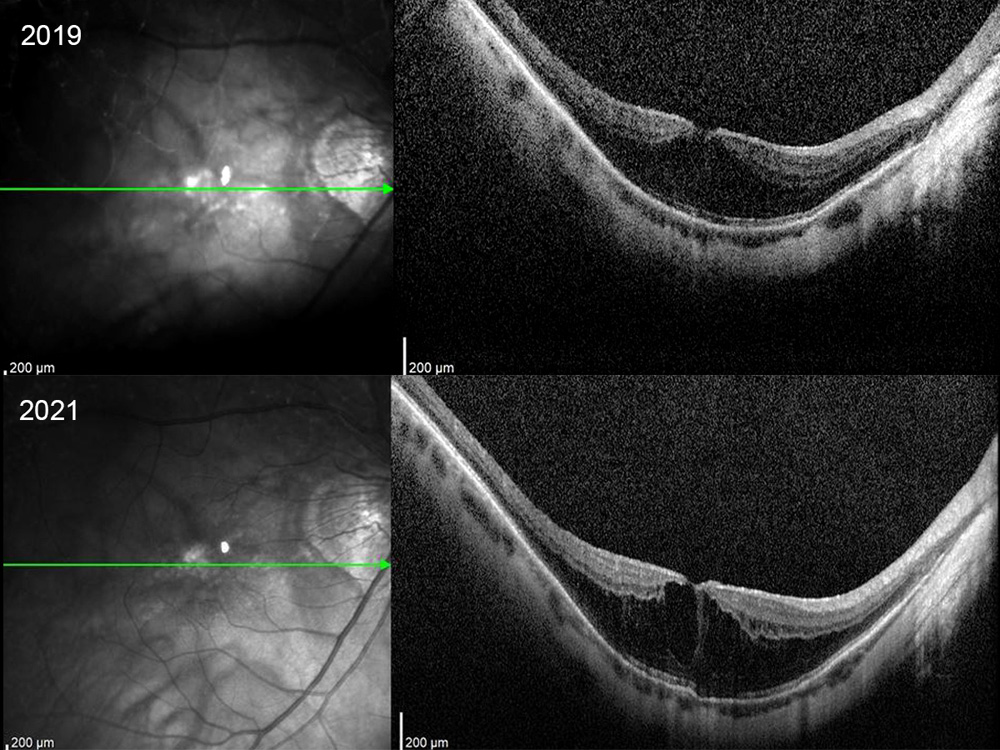
Figure 3: SD-OCT scan of the right macula 20 months and 2 months prior to the development of the macular hole. Note the progression in the myopic macular schisis.
Differential Diagnosis
The latanoprost was stopped in Aug 2021 at the time of her macular hole diagnosis. Two months after latanoprost was stopped, the patient’s macular hole closed, and the vision improved to 20/80. Over the following two months the subretinal fluid gradually resolved and the vision improved to 20/63 (Figure 4).
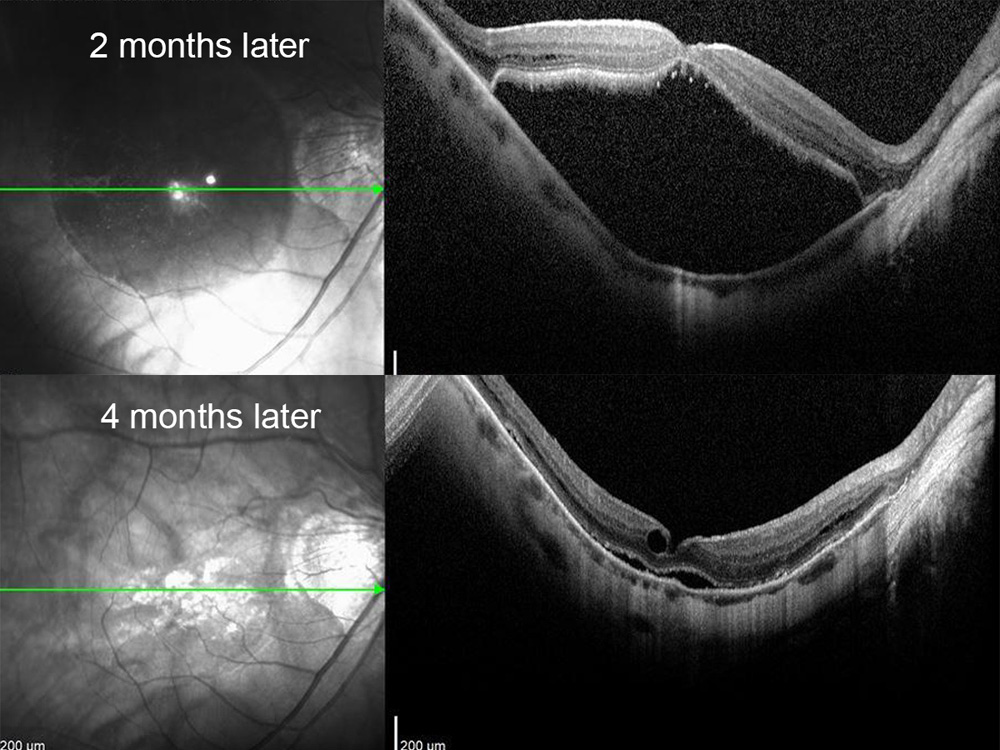
Figure 4: SD-OCT scan of the right macula 2 and 4 months after cessation of latanoprost. Note the resolution of the macular hole and macular detachment.
Did cessation of latanoprost have anything to do with this favorable outcome?
Latanoprost is a prostaglandin analogue. Prostaglandins are inflammatory mediators generated through the arachidonic acid cascade. They bind prostaglandin receptors on capillary endothelial cells and facilitate the opening of the tight junctions between those cells, which leads to increased vascular permeability and leakage.1
Prostaglandins can cause cystoid macular edema (CME) in pseudophakic eyes. Due to breakdown in the blood aqueous and blood retinal barrier - which can be caused by insults such as glaucoma, cataract surgery, chronic inflammation - prostaglandins gain access to the back of the eye where they cause leakage in the Henle fiber layer, resulting in CME.2 Several published cases have shown that exogenous prostaglandin analogues like latanoprost act in a similar manner.3-5
Latanoprost may have induced CME in our patient, causing worsening myopic schisis in 2019. This is debatable, since this could have also been the natural history of progressive myopic macular schisis. However, the timeline suggests that stopping the latanoprost may have decreased CME and influenced subsequent closure of the small macular hole.
The effect of topical therapy on full thickness macular holes is not a novel concept. In fact, topical therapy is often used to facilitate closure of smaller macular holes. Prior studies have shown successful anatomic closure of full thickness macular holes and improvement in visual acuity with topical non-steroidal anti-inflammatory,6,7 carbonic anhydrase inhibitors,8,9 and steroids.10,11 A study by Niffeneger et al used combinations of all three classes of drugs and demonstrated high closure rates (89%) of secondary full thickness macular holes over an average of 6 weeks, especially holes that were small and with CME.12