August, 2021
Presented by Braden Burckhard, MD


Presented by Braden Burckhard, MD

A 58 year-old female presented with decreased vision in her right eye for a duration of 3 years.

Figure 1A: Color photo of the right eye. Note the optic nerve edema and the presence of an optociliary shunt vessel.
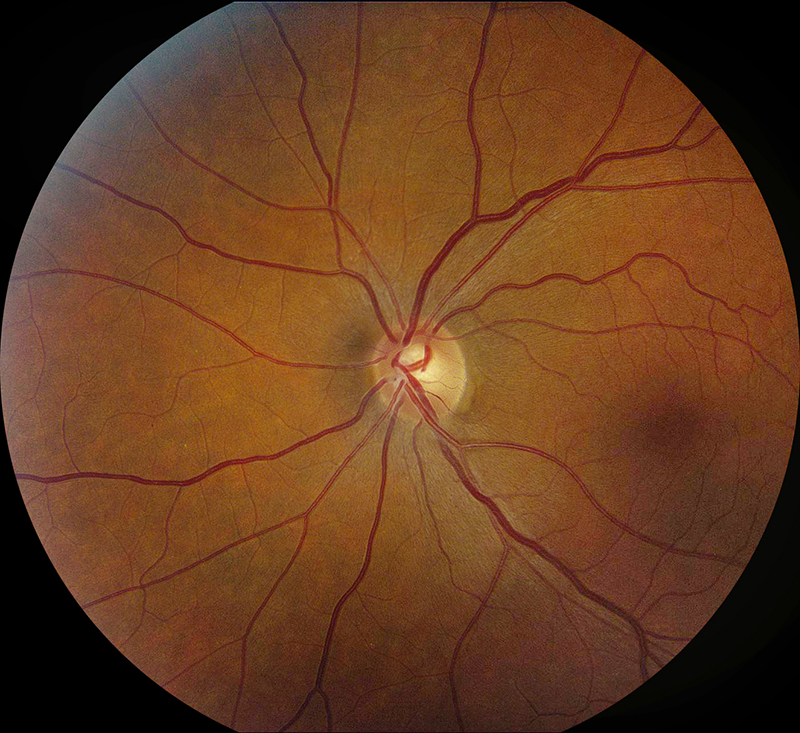
Figure 1B: Color photo of the left eye. The optic nerve is normal.
The patient first noticed visual symptoms about 3 years prior to her initial presentation. She described haziness of her peripheral vision that was mostly stable with slight worsening over the past year. She denied any ocular pain at rest or with eye movements, but she did note some discomfort to palpation. She was seen by an outside provider at the onset of her initial symptoms and was found to have a “swollen” optic nerve. Workup performed at that time was unremarkable, including MRI of the orbits and brain. Due to social circumstances, she was lost to follow up for the past year. Her past medical history and review of systems were otherwise unremarkable. She was not taking any prescription medications and has not used any illicit substances. Her past ocular history is unremarkable.
Her examination showed a Snellen visual acuity of 20/80 with pinhole to 20/40 in the right eye (OD) and 20/20 in the left eye (OS). Her intraocular pressure was 13 mmHg OD and 10 mmHg OS. Anterior segment examination was unremarkable OU. The funduscopic examination of the right eye showed mild disc edema with slight blurring of the margins. There were also optociliary shunt vessels present at the disc (figure 1A). The left eye fundus exam was unremarkable (figure 1B). Spectral domain optical coherence tomography (SD-OCT) showed normal retinal architecture in both eyes (Figures 2A and B). Red free imaging was performed but did not show any additional findings. A B-scan of the right eye was obtained showing elevation of the optic disc and increased signal along the optic nerve sheath (Figure 3).
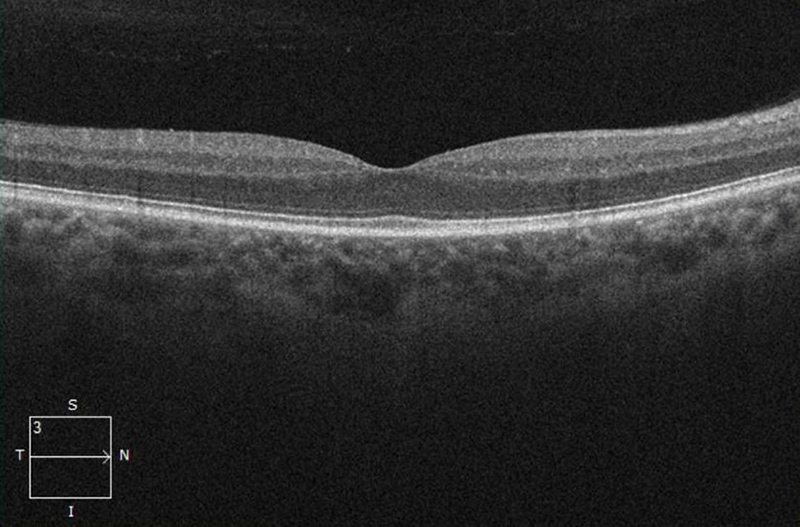
Figure 2A: OCT-SD scan of the the right macula. Some thinning of the nerve fiber layer appears to be present.
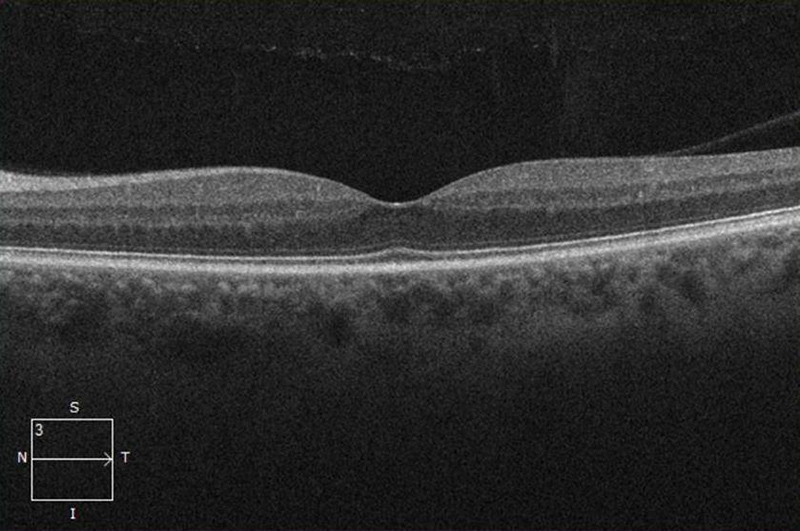
Figure 2B: OCT-SD scan of the left macula. The scan is unremarkable.
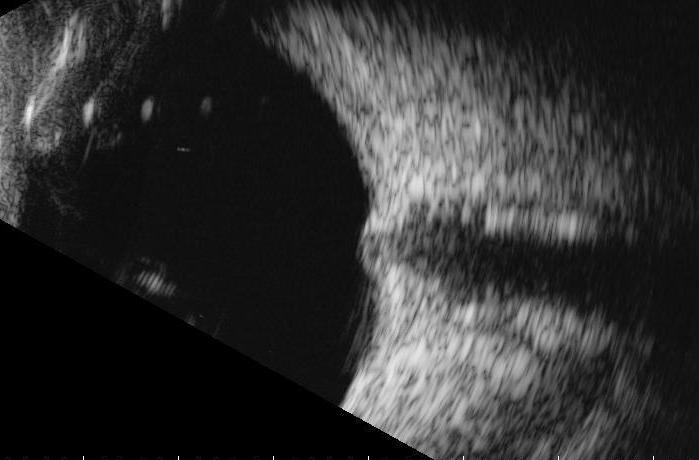
Figure 3: B-Scan of the right eye. The optic nerve shadow appears enlarged.
Additional History, Diagnosis and Patient Course
The patient’s fundus findings and B-scan prompted further referral with further evaluation by neuro-ophthalmology 8 days. With prolonged effort, her right eye acuity measured 20/20. Her left eye acuity was 20/30. Ishihara plates were 4/7 OD and 7/7 OS. Confrontational fields were depressed in the right eye compared to left eye. Her pupils were equal and reactive but she had a right relative afferent pupillary defect. Her fundus examination was unchanged. Humphrey 24-2 visual fields showed marked constriction OD and a normal field OS. OCT measurements of the RNFL thickness was 145 um OD and 97 um OS. Macular ganglion cell thickness was depressed on the right with an average GCC of 80 um OD and 101 um OS reflecting ganglion cell loss on the right.
Due to the presence of progressive visual loss, chronic optic disc edema with progressive atrophy, and the development of optociliary shunt vessels, the patient underwent repeat MRI testing. Her results revealed a contrast-enhancing lesion encasing her right optic nerve (Figures 4A and B). The appearance of the mass, combined with her clinical history and optic disc appearance, was consistent with the diagnosis of optic nerve sheath meningioma (ONSM). After discussing the risks and benefits of treatment versus observation, the patient chose to pursue radiation therapy and subsequent monitoring with neuro-ophthalmology.
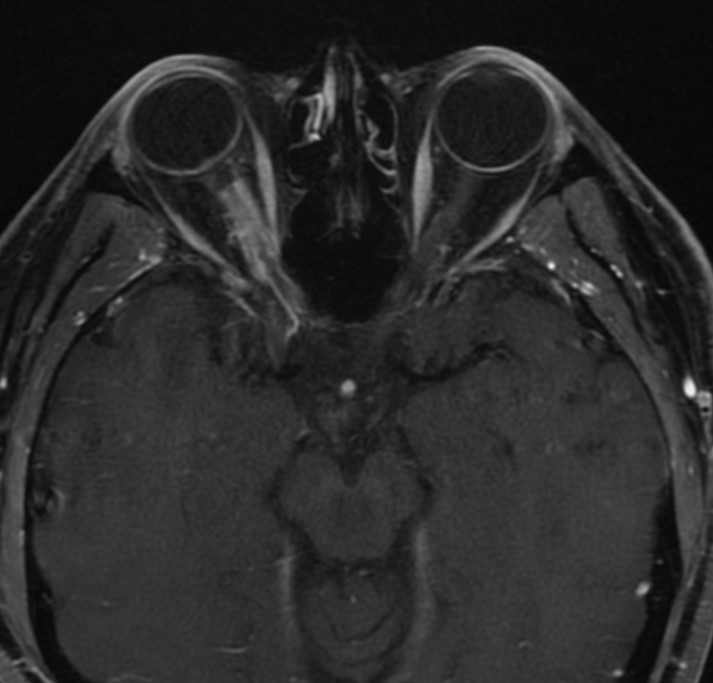
Figure 4A: MRI scan. Note the contrast enhancing right optic nerve lesion producing what has been described as the 'tram-track sign'
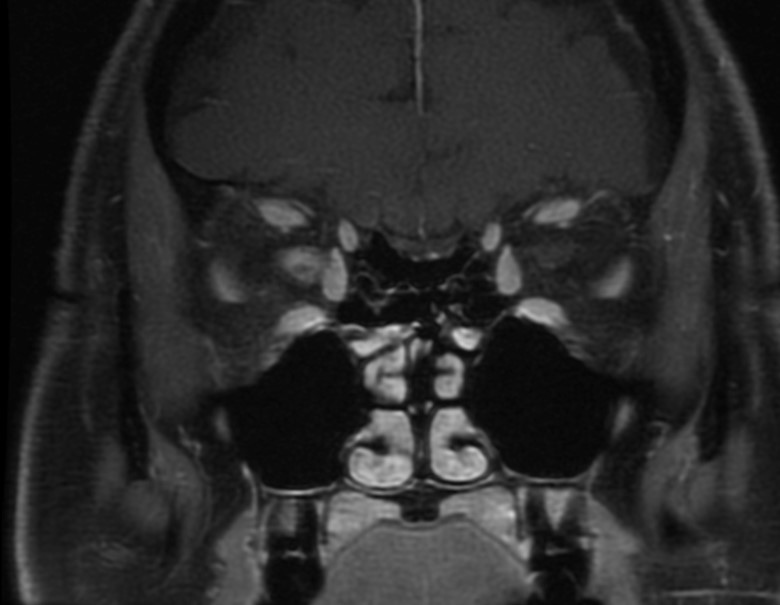
Figure 4B: MRI coronal scan. Note the contrast enhancing right optic nerve lesion producing a 'ring sign'.
Discussion
Optic nerve sheath meningiomas (ONSM) are the second-most common primary optic nerve tumors after gliomas.1 They originate from the optic nerve sheath as their name suggests, and primarily affect middle-aged adults.1 They account for one-third of all primary optic nerve tumors and most of these lesions are unilateral (95%).1,2 The incidence of ONSM is highest in adult women in the fourth or fifth decades of life, with women being three times more likely than men to be affected.3 ONSM can also occur in children but a review of cases by Dutton showed that only 4% of these tumors occurred in patients younger than 20 years.1 Although most are idiopathic, there is an association between ONSM and exposure from ionizing radiation, as well as neurofibromatosis type 2.2
Patients with ONSM typically present with the classical clinical triad: progressive, painless, monocular vision loss, optic atrophy, and optociliary shunt vessels.2 Diagnostic testing usually reveals reduced color vision, visual field loss, and an ipsilateral afferent pupillary defect. Neuroimaging with magnetic resonance imaging (MRI) is most commonly used to confirm the diagnosis. Contrast and fat suppression techniques are often utilized to improve visualization of the optic nerve. As seen in our patient’s MRI, the “tram track sign” and “ring sign” are highly indicative of a meningeal tumor. Biopsy of these lesions are rarely performed due to risk of injury to the optic nerve and the high diagnostic sensitivity of MRI when combined with clinical findings.
The most common management options for ONSM include observation, surgical excision, or radiation therapy. Turbin et al evaluated visual acuity outcomes in patients who underwent observation, surgical therapy, external beam radiation, or a combination of surgery and radiation. All groups had statistically similar initial visual acuities, but the only group showing no significant decrease in visual acuity belonged to patients receiving external beam radiation without surgery.4 Studies have shown stable or improved visual acuity in up to 95% of patients who receive intensity-modulated radiotherapy.2 Management with surgical intervention has become less popular due to risk of damage to the optic nerve and increased percentage of tumor progression post-operatively. A study by Sasano et al showed a 17.8% chance of tumor progression after treatment with microsurgery.5 Surgical excision, however, may play a role in patients with blind, painful eyes, with severe proptosis or cosmetic deformities. And although rare, patients with intracranial extension may benefit from combined surgical excision and radiation to successfully reduce tumor burden and prevent spread to the contralateral orbit.
Observation may be a favorable option in patients who are asymptomatic and have preserved visual function. However, these patients should be closely monitored with visual field and retinal nerve fiber thickness studies, in addition to repeated neuroimaging, in order to detect any early progression of disease. However, patients who demonstrate progressive loss of visual function should be considered for fractionated, stereotactic, intensity-modulated radiation therapy, as it is generally the most preferred therapy for symptomatic ONSM.6 Patients receiving radiation should be followed for adverse effects which include: radiation retinopathy, optic neuropathy, iritis, cataract formation, and hypopituitarism.7
Although ONSM is relatively benign in adults, pediatric ONSM has been shown to have an increased malignant potential. Due to a higher rate of intracranial spread, an increased rate of complications following radiotherapy, and lack of literature concerning radiotherapy in the pediatric population, studies suggest that surgical prevention be the primary treatment for children with ONSM.8-10
The prognosis of patients with ONSM is widely variable, depending on the degree of involvement/compression on the optic nerve and the rate of progression of the tumor. Presenting visual acuity is one of the only prognostic markers: patients presenting with decreased visual acuity have poorer visual outcomes. In patients treated with radiation, stable or improved vision post-treatment was seen in 92.3% of patients with good pre-treatment vision (best corrected visual acuity 6/18 or better), compared to only 61.5% of patients with poor pre-treatment vision (best corrected visual acuity 6/24 or worse).11