Dec, 2020
Presented by Braden Burckhard, MD


Presented by Braden Burckhard, MD

A 71-year-old Caucasian male presented with 2 days of vision loss in the right eye
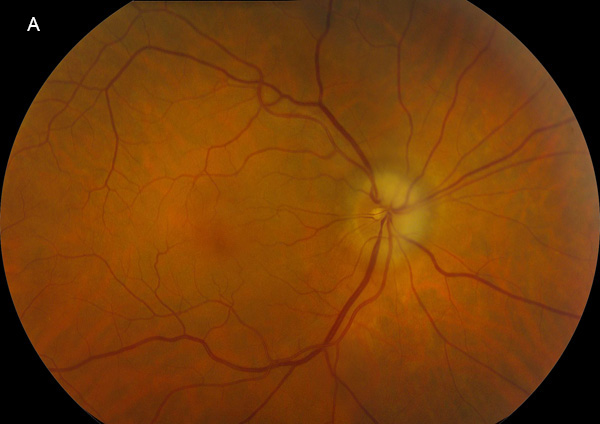
Figure 1A: Color photo of the right eye. Note the pale swelling of the optic nerve superiorly and nasally. Focal narrowing of the retina veins are noted over the nerve.

Figure 1B: Color photo of the left eye is unremarkable.
The patient noticed progressive loss of vision over the past 2 days that involved the inferior and temporal visual field of the right eye only. He stated the vision was “foggy” in these areas, but clear centrally. He denied any new flashes or floaters. However, he did endorse jaw pain and muscle spasms in his tongue that began one month prior. He stated he had lost 15 pounds during that time due to difficulties chewing. He also described having a persistent, severe headache and arthralgias. Upon further questioning, he also experienced pain and tenderness over the right scalp region. He denied any significant past ocular history. His past medical history includes hypercholesterolemia, hypertension, and anemia. He is currently taking lisinopril, rosuvastatin, aspirin, hydrochlorothiazide, and ezetimibe. His family history is unremarkable. He denied smoking but does have occasional alcohol use. The remainder of his review of systems was negative.
His best corrected Snellen visual acuity measured 20/25 in the right eye (OD) and 20/25 in the left eye (OS). His intraocular pressure was 13 mmHg in both eyes. Confrontational visual field testing revealed temporal and inferior field loss in the right eye. Anterior segment examination showed mild nuclear sclerosis in both eyes. The funduscopic examination of the right eye showed superior and nasal disc edema, and focal venous narrowing over the optic nerve (Figure 1A). Exam of the left retina was unremarkable (Figure 1B). Spectral domain optical coherence tomography (SD-OCT) demonstrated a normal appearance of the macula in both eyes. Fluorescein angiography (FA) showed delayed choroidal filling in the right eye and optic nerve staining. (Figures 2A-C). The left eye showed normal vascular filling (Figure 2D).
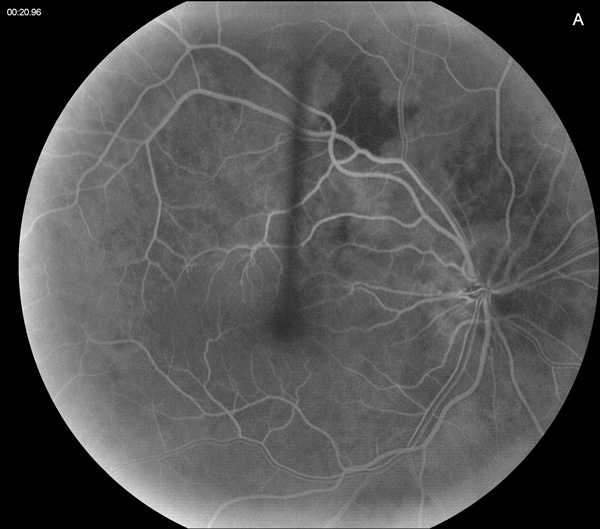
Figure 2A: Early phase fluorescein angiogram of the right eye. Note the areas of delayed choroidal filling.

Figure 2B: Mid-phase fluorescein angiogram of the right eye. The choroid shows complete filling.
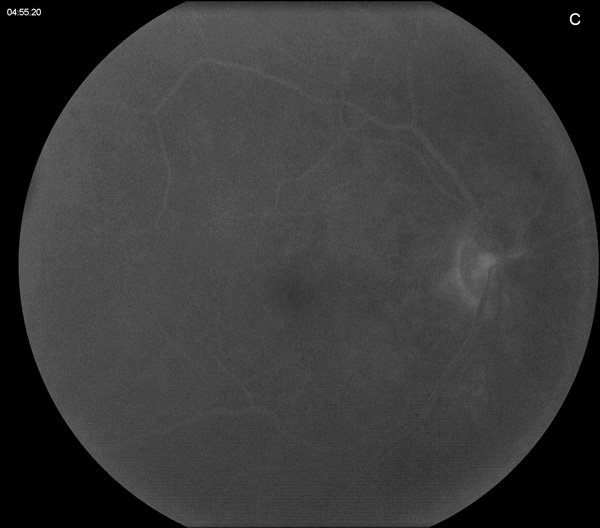
Figure 2C: Late phase fluorescein angiogram of the right eye. Mild staining of the optic nerve is present, with some blocked fluorescence nasally due to the optic nerve swelling.

Figure 2D: Mid-phase fluorescein angiogram of the left eye is unremarkable.
Differential Diagnosis
Additional History, Diagnosis and Patient Course
Due to the patient’s signs and symptoms, he was immediately started on 100 mg/day of oral prednisone and was sent for the following lab draws: erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and a complete blood count (CBC). The patient’s primary care provider was notified and management was coordinated with the Oculoplastics service to schedule a temporal artery biopsy the following day, due to strong suspicion for GCA.
Labs returned as the following: ESR: 29 mm/hr (0-30 mm/hr), CRP: 38 mg/L (0-10 mg/L), platelets: 547,000/mcL (150,000-400,000/mcL). The biopsy of the right temporal artery was positive for GCA, confirming the diagnosis of AAION (Figure 3A and B).
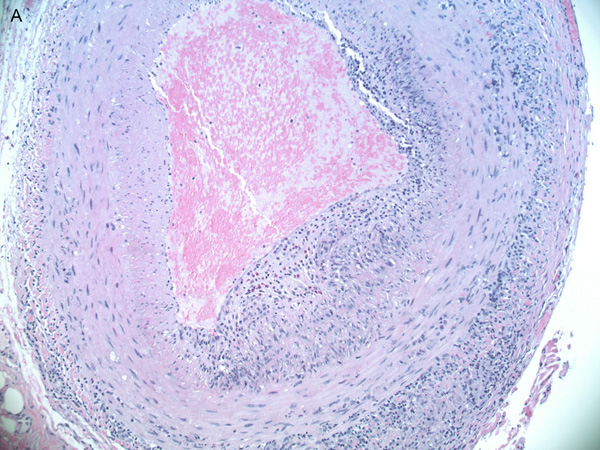
Figure 3A: Lower power histopathologic section of the temporal artery biopsy showing inflammation in all layers.
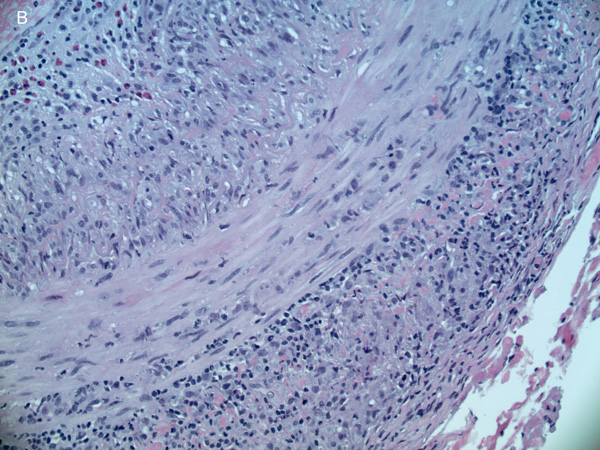
Figure 3B: Higher power view of the temporal artery biopsy showing lymphocytes, histiocytes and eosinophils in all layers.
The patient returned to our clinic 2 weeks later, still taking 100 mg of oral prednisone and tolerating the medication without significant side effects. Subjectively, the patient noticed slight worsening of his visual function in the right eye and his acuity had decreased to 20/50. His left eye remained asymptomatic, with stable acuity of 20/25. His IOP remained normal. The patient’s systemic symptoms had improved since starting oral steroids. He demonstrated a 2+ relative afferent pupillary defect OD. His anterior segment exam remained unchanged. His disc edema in the right eye had progressed to 360 degrees of involvement, with the presence of a flame hemorrhage over the temporal margin of the disc (Figure 4). The patient was continued on oral steroids and referred to rheumatology for co-management of his systemic therapy and consideration of transition to tocilizumab.

Figure 4: Color photo of the right eye 2 weeks after presentation. Note the increase in pale swelling of the optic nerve.
Discussion
Giant cell arteritis (GCA), also referred to as temporal arteritis, is a systemic, large vessel vasculitis that may cause ischemic optic neuropathy. This ischemic process is a result of inflammation and subsequent thrombosis of the posterior ciliary arteries (PCAs) that perfuse the optic nerve head and the choroid.1 When involving the anterior segment of the optic nerve, the ischemia is characterized as AAION. The most common ocular manifestations are outlined in Table 1.2
Table 1
Our patient presented with the classic systemic symptoms of GCA, including scalp tenderness, jaw claudication, headache, and arthralgias. He also had disc edema and decreased choroidal perfusion noted on fluorescein angiography. With this constellation of symptoms, he was immediately started on high-dose systemic steroids before lab results were obtained. Despite having elevated CRP and platelet levels, his ESR was normal. Conflicting lab results may lead to over- or undertreating of patients, especially when GCA is only mildly suspected. A recent meta-analysis studied the diagnostic accuracy of the lab tests, symptoms, and physical signs for suspected GCA.3 A positive likelihood ratio of more than 2.00 occurred for the following findings: temporal artery thickening, temporal artery loss of pulse, temporal tenderness, anterior ischemic optic neuropathy, ESR of greater than 60, 80, and 100 mm/h, and a platelet count of greater than 400 × 103 /μL.3 However, it is important to note that in this meta-analysis, no single feature was likely to shift pretest probability sufficiently to make further investigation of GCA unnecessary.
As an alternative to temporal artery biopsy, large vessel imaging has been used for the diagnosis of GCA, especially in cases where biopsy is not possible. In 2018, Duftner et al investigated ultrasound of the temporal arteries and MRI of cranial arteries, which yielded pooled sensitivities of 77% and 73%, respectively, compared with a clinical diagnosis of GCA.4 The mean sensitivity for a unilateral temporal artery biopsy has been found to be around 87%, and thus remains the gold standard for diagnosis.5
When there is strong suspicion for GCA, systemic steroids should be initiated immediately, with the goal of preventing loss of vision in the fellow eye or involvement of other systems. Left untreated, fellow eye involvement occurs in up to 95% of cases.1 Pre-existing sight loss can progress, despite initiation of glucocorticoid therapy, in approximately 10% of patients, usually within the first week of treatment.6 Intravenous, high-dose, pulse steroids have been suggested for GCA, however, Hayreh et al showed no differences in improvement in visual acuity when comparing patients who received intravenous glucocorticoids followed by oral therapy with patients who received only oral glucocorticoids (initial dose of 60-120 mg/day).7 Temporal artery biopsy should be performed within 1-2 weeks of starting steroids. Prolonged steroid therapy is often required, and relapses are common. Tocilizumab, an interleukin-6 inhibitor, has been proposed for the management of relapsing disease or for the substitution of long-term glucocorticoid therapy. In a randomized study, better control was achieved with Tocilizumab combined with a prednisone as compared with a Prednisone alone. In this study, a 26-week Prednisone taper combined with tocilizumab given weekly or other week, achieved disease control in 56% and 53% of cases as compared with only 14% of cases when treated for 26- or 52-weeks with Prednisone alone. 8