February, 2021
Presented by Braden Burckhard, MD


Presented by Braden Burckhard, MD

A 53-year-old Caucasian male presented with 2 days of vision loss in the right eye.

Figure 1A: Color photo of the right eye. Note the faint yellowish area in the macula. The optic nerve and vessels appear normal.
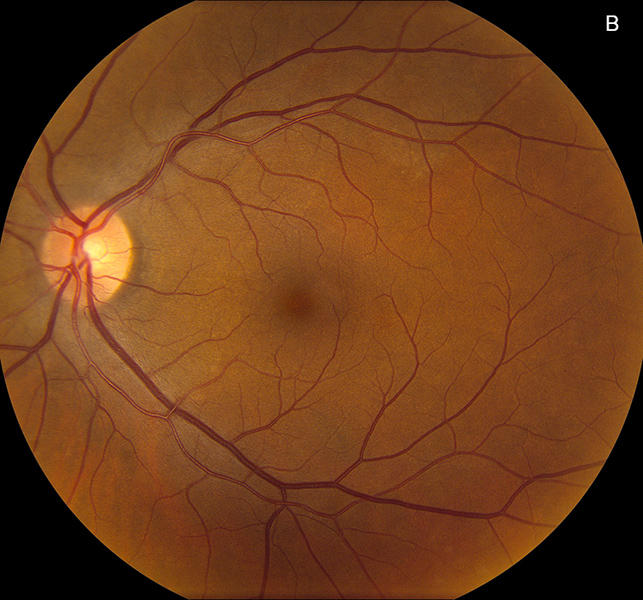
Figure 1B: Color photo of the left eye. Note the subtle yellowish area in the nasal macula and along the arcade. The optic nerve and vessels appear normal.
The patient noticed sudden onset vision changes that began 2 days ago. He describes the presence of a “gray streak of paint” in the center of his vision in the right eye only. He also noted intermittent flashes of light in both eyes on extreme gaze positions. He denied any significant past ocular history. His past medical history includes type 2 diabetes for which he takes sitagliptin and metformin. His family history is unremarkable. He denied smoking or alcohol use. There was no history of recent travel to outside countries. His review of systems was otherwise negative.
His best corrected Snellen visual acuity measured 20/250 in the right eye (OD) and 20/32 in the left eye (OS). His intraocular pressure was 10 mmHg in the right eye and 12 mmHg in the eye. Confrontational visual field testing was unremarkable. Anterior segment examination was unremarkable in both eyes. The funduscopic examination of the right eye showed subtle yellow discoloration and granularity of the RPE/choroid in the peripapillary region and macula (Figure 1A). Similar findings were noted in the in the peripapillary region of the left eye, as well as along the superotemporal arcade (Figure 1B). Fundus autofluorescence scans of both eyes showed hyperautofluoresence primarily in a peripapillary distribution though areas were noted in the nasal mid periphery of the right eye, and temporally in the left eye (Figures 2A and B). Spectral domain optical coherence tomography (SD-OCT) demonstrated disruption of the IS/OS junction and interdigitation zone at the fovea and parafoveal region OD, with similar findings at the nasal macula OS (Figures 3A and B). Fluorescein angiography (FA) showed patchy, mixed, hypo- and hyperfluorescence in the early phase (Not shown), with subtle peripapillary late staining (Figures 4A and B.
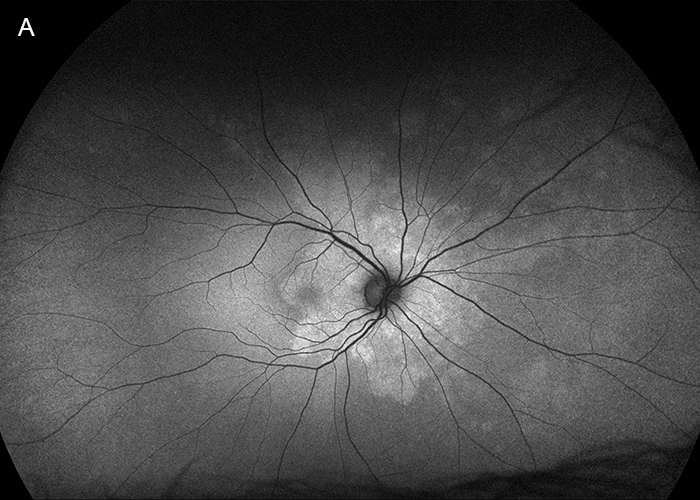
Figure 2A: Fundus autofluorescence right eye. Hyperautofluorescence is noted surrounding the optic nerve, with more faint areas in the nasal retina.

Figure 2B: Fundus autofluorescence left eye. Hyperautofluorescence is noted surrounding the optic nerve, with other areas noted temporally.
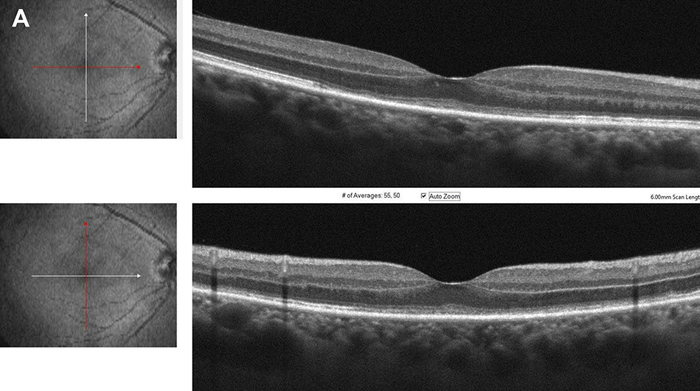
Figure 3A: Spectral domain OCT right eye, horizontal and vertical scans through the macula. Note the disruption of the photoreceptor layer.
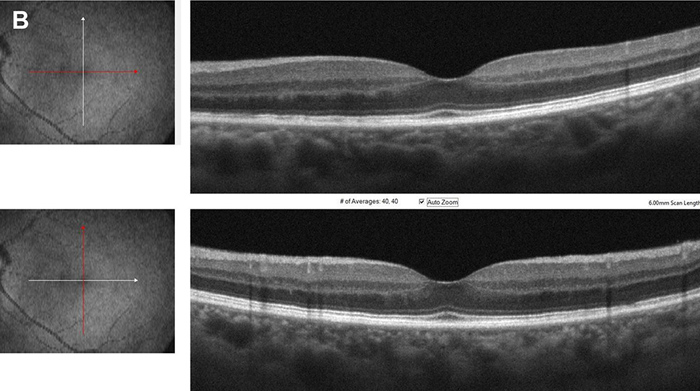
Figure 3B: Spectral domain OCT left eye, horizontal and vertical scans through the macula. Note the disruption of the photoreceptor layer.
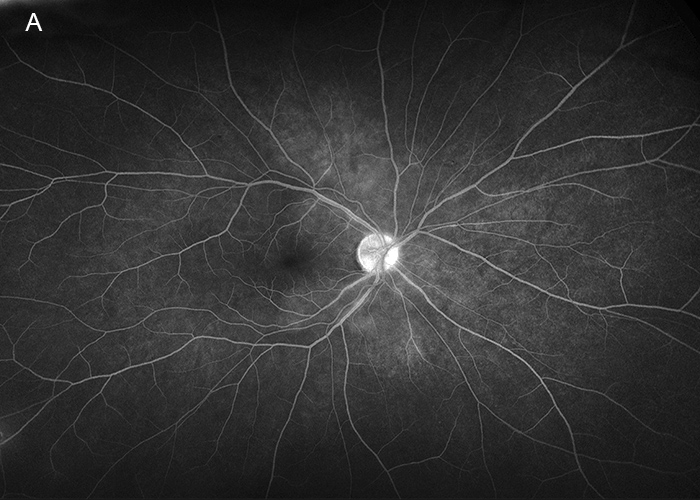
Figure 4A: Wide-field fluorescein angiogram of the right eye. Subtle hyperfluorescence is noted in the peripapillary area.
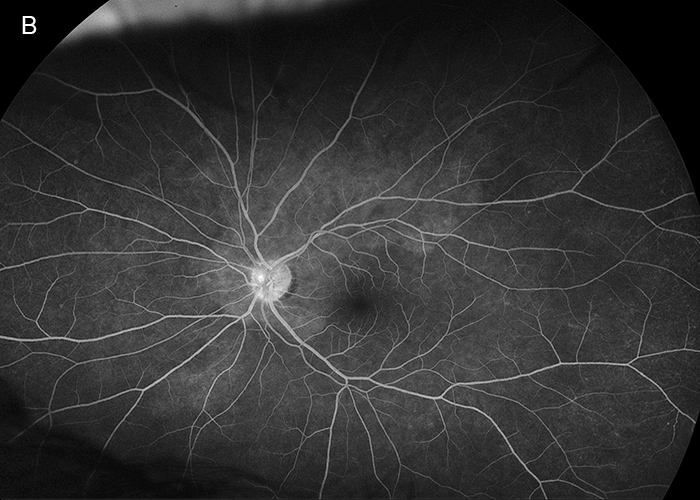
Figure 4B: Wide-field fluorescein angiogram of the left eye. Subtle hyperfluorescence is noted in the peripapillary area.
Differential Diagnosis
Additional History, Diagnosis, and Patient Course
Upon further questioning, the patient reported a history of HIV diagnosed 6 years prior and having unprotected sexual contact with other men. He denied any previous history of syphilis but had contracted other STI’s in the past which were successfully treated. He denied having any current rashes or neurological symptoms. Based on his presentation and imaging results, the following labs and testing were obtained: ESR, CRP, CBC, CMP, RPR, QuantiFERON-TB gold, CXR, and CD4 count. These results showed an elevated ESR of 66 (0-20 mm/hr), reactive RPR, and reactive FTA-ABS, consistent with a diagnosis of syphilis. His absolute CD4 count was within normal limits at 837 (490-1740 cmm). The patient’s primary care provider was contacted, and treatment was immediately initiated with intravenous penicillin G for a planned 14 day course. The patient returned in one week and his symptoms had nearly resolved, with improvement of his visual acuity to 20/40 OD and 20/20 OS (previously 20/250 and 20/32). The patient was seen again in 2 weeks, with further improvement in the right eye acuity to 20/32. The patient’s OCT showed substantial improvement of the outer retina architecture in the right eye (Figures 5A and B). Fundus autofluorescence showed a reduction in the areas of hyperautofluorescence (Figures 6A and B).
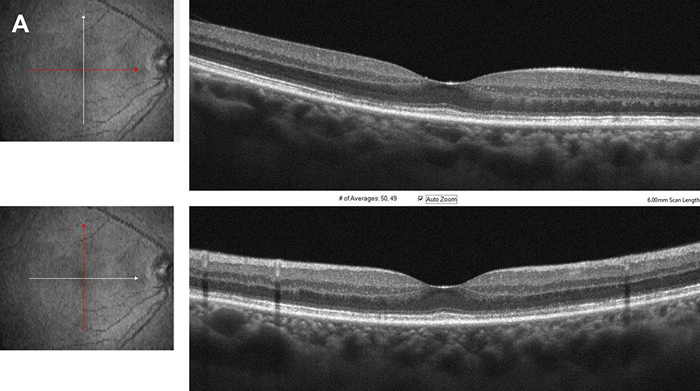
Figure 5A: Spectral domain OCT right eye, horizontal and vertical scans through the macula. There has been a marked improvement in the photoreceptor layer.
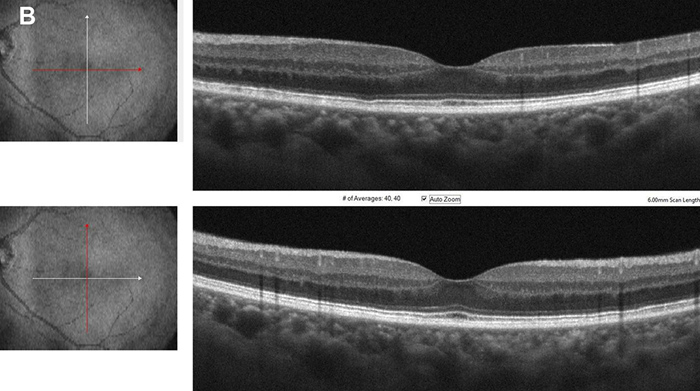
Figure 5B: Spectral domain OCT left eye, horizontal and vertical scans through the macula. There has been a marked improvement in the photoreceptor layer.
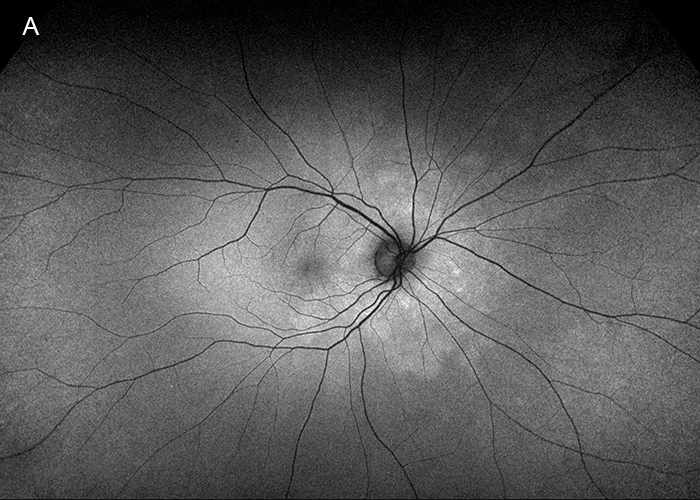
Figure 6A: Fundus autofluorescence right eye. The peripapillary area of hyperautofluorescence is less prominent.
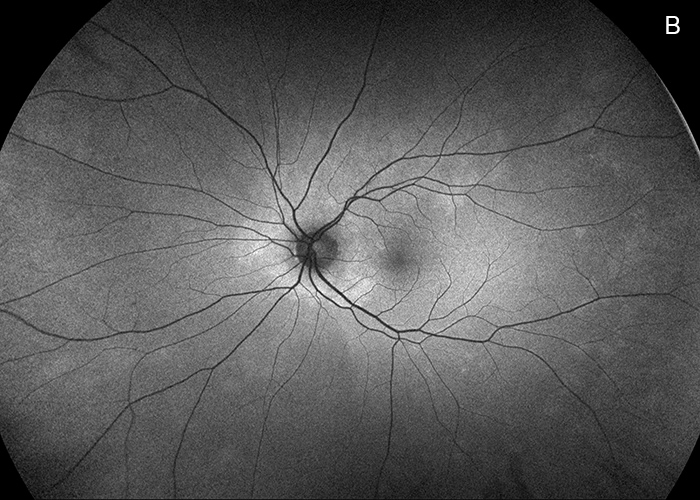
Figure 6B: Fundus autofluorescence left eye. The peripapillary area of hyperautofluorescence is less prominent.
Discussion
The incidence rate of syphilis continues to grow yearly in the United States. Between 2017 and 2018, the incidence grew 14.4%.1 Worldwide, there are an estimated 6-7 million new cases annually, with higher rates in men who have sex with men and those who are coinfected with HIV.2
Syphilis should be considered in the differential diagnosis for any unexplained ocular inflammation, especially when in patients who are HIV positive. In addition to uveitis, patients may present with placoid, yellowish, outer retinal lesions typically found in the macula or juxtapapillary region. These findings were initially described by de Souza et all in 19893 and later termed acute syphilitic posterior placoid chorioretinitis (ASPPC) by Gass in 1990.4 The lesions likely arise from active inflammation at the level of the choriocapillaris–pigment epithelial–retinal photoreceptor complex.4 On early-phase FA, the lesions are typically hypofluorescent or mildly hyperfluorescent, with scattered hypofluorescent spots often described as leopard spotting.4 Hyperfluorescence of the lesions usually increases in later phases of the FA. Hyperautofluorescence has been previously described, correlating to the areas of chorioretinal involvement.5 The placoid lesions may be accompanied by variable amount of vitreous inflammation and may be associated with superficial hemorrhages, retinal vasculitis, disc edema, and subretinal fluid.6 In a case series by Eandi et al, 9 of 16 (56%) patients with ASPPC had bilateral involvement.7
The SD-OCT findings through acute syphilitic posterior placoid chorioretinitis have previously been reported8 and our patient had similar findings, with loss of detail of the photoreceptor IS/OS junction and external limiting membrane.
ASPPC can occur independently of the immune status of the patient, however, it is more common in those affected with HIV, as seen in our patient.1 His ancillary testing demonstrated a process involving the retinal pigment epithelium/choroid complex with secondary insult to the photoreceptor IS/OS junction layer. The visual acuity, OCT, and FAF significantly improved after the patient completed two weeks of IV penicillin G therapy.