Feb, 2023
Presented by Malini Veerappan Pasricha, MD


Presented by Malini Veerappan Pasricha, MD

A 68-year-old woman is referred for evaluation of peripapillary lesion in her left eye.

Figure 1A: Color photo of the right eye. The disc and macula are normal.

Figure 1A: Color photo of the left eye. Note the yellowish-orange peripapillary lesion from about 2:00 to 8:00.
The patient had no visual complaints. She denied any flashes, floaters, scotoma, pain, or headaches. Her past ocular history was significant for myopia (-3.00 D right eye, -5.00 D left eye), age-related cataracts, and low risk glaucoma suspect. Medical history was significant for breast cancer, skin cancer (squamous, basal, and melanoma), and hypothyroidism. Surgical history was significant for left mastectomy. Her medications are anastrozole and ebemaceclib (chemotherapy for metastatic breast cancer) and levothyroxine. Family history was significant for retinal detachment in her father. No known allergies. She denies use of tobacco or illicit substances. Review of systems was negative.
The patient’s best corrected Snellen visual acuity measured 20/40 OD and 20/200 OS. Of note, she wears soft contact lenses and is corrected for monovision (right eye distance, left eye near). Intraocular pressures were normal. Anterior segment exam was age-appropriate. Examination of the right eye was unremarkable (Figure 1A). Examination of the left eye showed a yellowish-orange peripapillary lesion from 2:00 to 8:00 o’clock. An anomalous disc with a focal area of apparent atrophy was noted with the inferotemporal vein appearing to dip in and out of this area.
Differential Diagnosis
Additional history and Testing
The OCT and FA of the right eye was normal. The FA of the left eye shows faint hyperfluorescence around the optic nerve but no leakage (Figures 2A and B). The horizontal and vertical OCT scans of the left eye showed a choroidal hyporeflective area with some outward bowing of the sclera corresponding to the peripapillary lesion (Figures 3A and 2B, respectively).
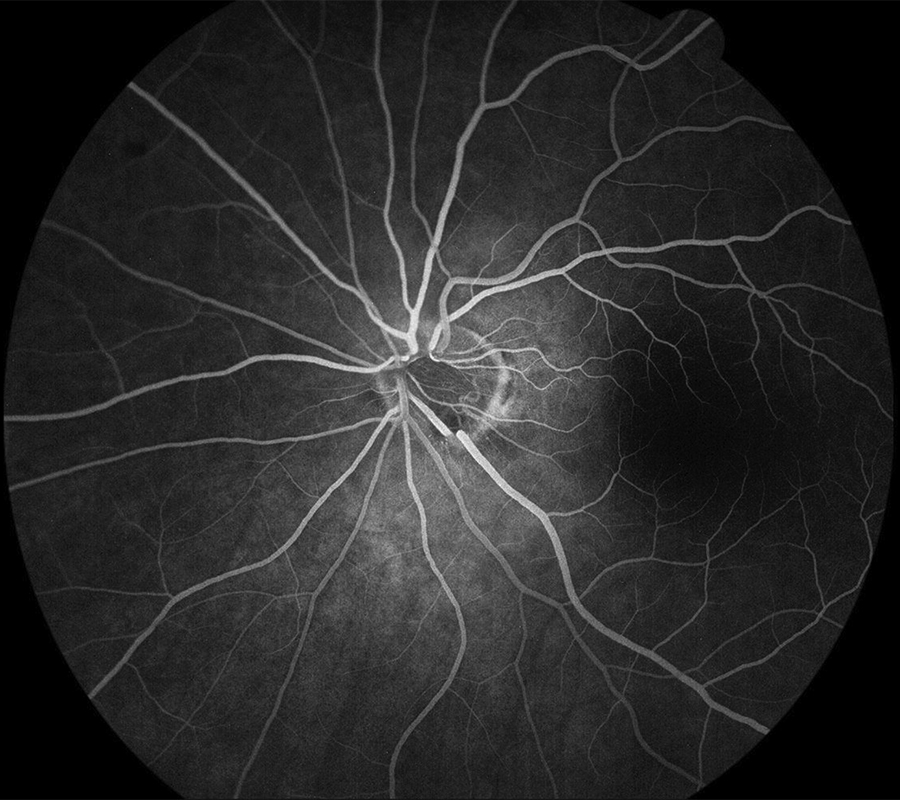
Figure 2A: Early-phase fluorescein angiogram of the left eye. Mild increased fluorescence is seen in the area of the lesion without leakage.
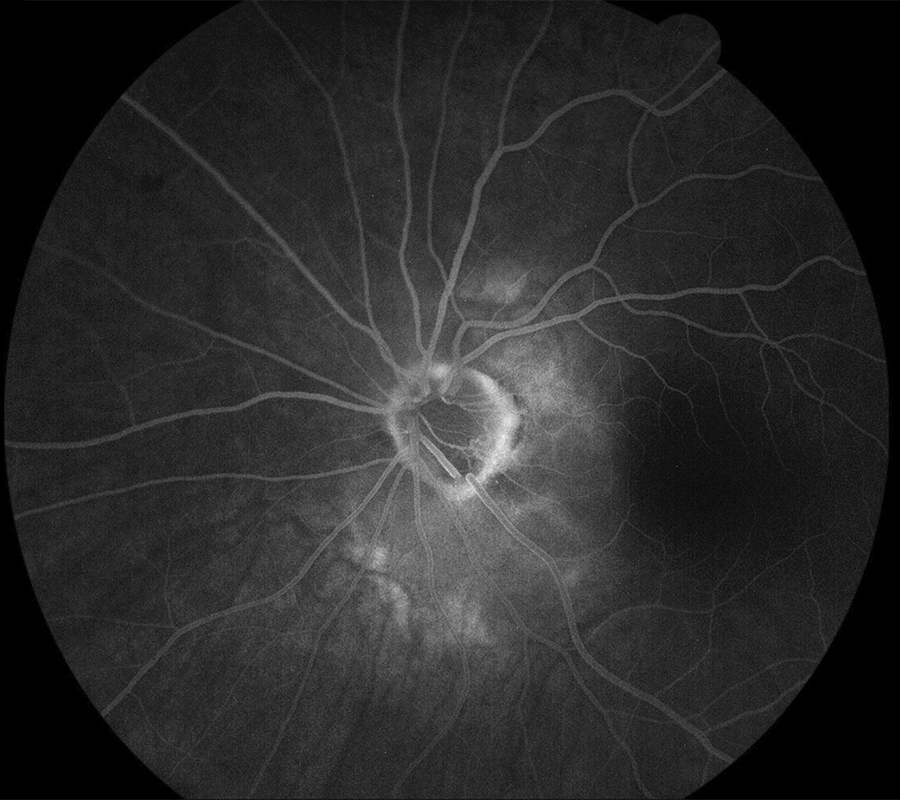
Figure 2B: Late-phase fluorescein angiogram of the left eye. Mild late staining is seen in the corresponding to the peripapillary lesion.
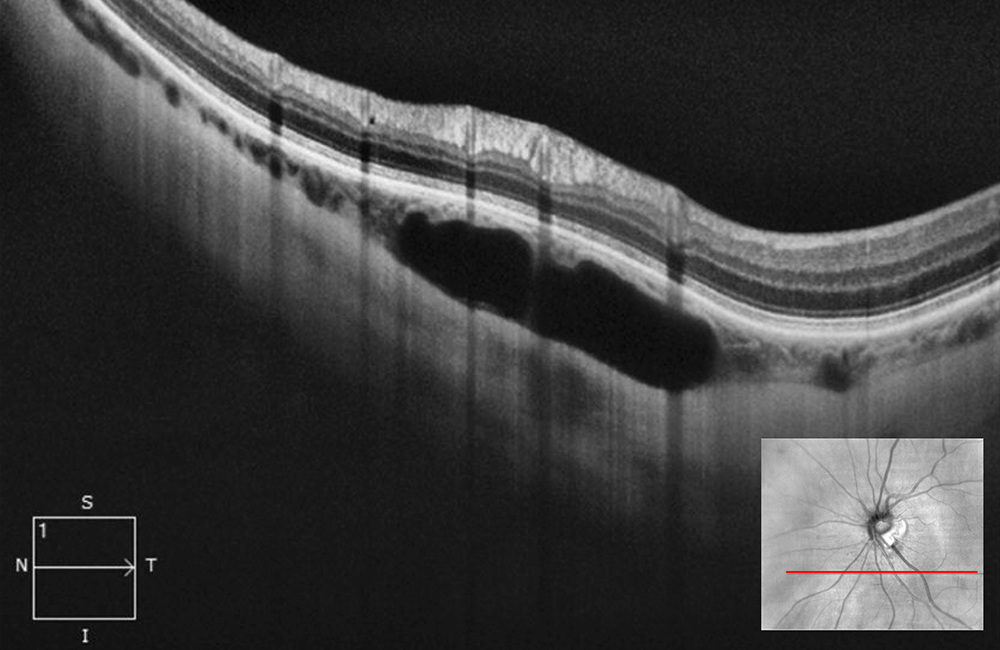
Figure 3A: Horizontal OCT-SD scan just below the optic nerve through the lesion in the left eye. Note the hyporeflective area with some slight outward bowing of the posterior sclera.
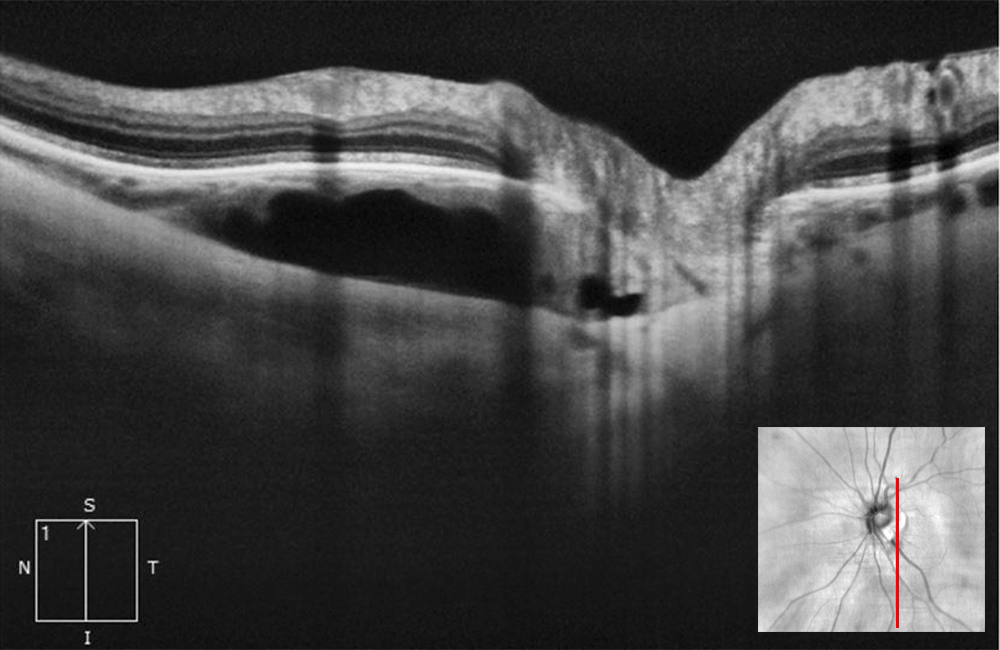
Figure 3A: Vertical OCT-SD scan just below the optic nerve through the lesion in the left eye. Note the hyporeflective area with some slight outward bowing of the posterior sclera.
Diagnosis
The history of myopia, and findings on fluorescein angiography and choroidal hyporeflectivity noted on OCT scans confirms a diagnosis of choroidal cavitation.
Discussion
Peripapillary intrachoroidal cavitation (PICC) is a focal choroidal defect usually found in the inferior border of the peripapillary conus in myopic eyes. In 2003, Freund et al identified and termed this lesion as peripapillary detachment in high myopia, based on clinical and early-stage OCT findings.1 With newer generation OCT imaging demonstrating choroidal cavitation under a normal plane of retina and RPE, the term has evolved to peripapillary intrachoroidal cavitation.2-6
The prevalence is estimated to be 2-5% in myopic eyes and 16-22% in highly myopic eyes.7-9 Apart from myopia, predisposing factors include older age and co-existence of myopia related retinal lesions (lacquer cracks, tessellated fundus, posterior staphyloma, patchy atrophy) and/or optic disc abnormalities (optic pit, tilted disc).10,11 The affected eye of our patient had a posterior staphyloma.
PICC in isolation is usually asymptomatic. On funduscopic exam, PICC appears as a well-defined yellow-orange lesion along the border of the myopic crescent.1,2 On OCT, PICC appears as an intrachoroidal hyporeflective area situated below a normal plane of RPE, often accompanied by choroidal thickening and an associated posterior bowing of the sclera.2,12 On OCTA, PICC has been shown to correspond to lower density of choroidal and choriocapillary vessels.13,14 On FA, PICC demonstrates early hypofluorescence and late hyperfluorescence consistent with staining.15 In our case, the area showed a bit increased fluorescence which appears to be due to an intact RPE/choriorcapillaris overlying the lesion as compared with many cases associated with RPE atrophy and loss of choriocapillaris. There have been reports of visual field defects associated with PICC.16
The exact pathogenesis of PICC is unclear. A hypothesis of congenital etiology (ie incomplete closure of the embryonic fissure) has been abandoned since PICC has not been described in children and has been found in locations other than the inferior border of the disc.1,2 An alternative hypothesis is that PICC is the result of choroidal retraction away from the optic disc border, following a break in the border tissue of Elshnig during staphyloma progression in myopic eyes.2 Additionally, stretching and disruption of the border tissue gives liquified vitreous a conduit into the choroid, creating a fluid pocket.5 Other studies have described PICC to occur as a consequence of mechanical bowing of the posterior sclera.12 PICC lesions are more common with higher degrees of myopia suggesting axial elongation as a contributing factor.
PICC is considered non-progressive and is typically not associated with vision changes over time.1 The visual prognosis of eyes with PICC is primarily related to their associated myopia and myopic complications. Given its asymptomatic and stable nature, no intervention is indicated. However, it is necessary to rule out other similar appearing funduscopic abnormalities, such as CNV, that do require treatment. There have been some case reports of PICC being associated with progressive retinoschisis, macular detachment, and macular holes. However, since these are also associated with pathologic myopia, it is difficult to determine the culpability of PICC.17-19