January, 2022
Presented by Braden Burckhard, MD


Presented by Braden Burckhard, MD

A 31-year-old Asian female presented with 3 weeks of blurred vision in the right eye.
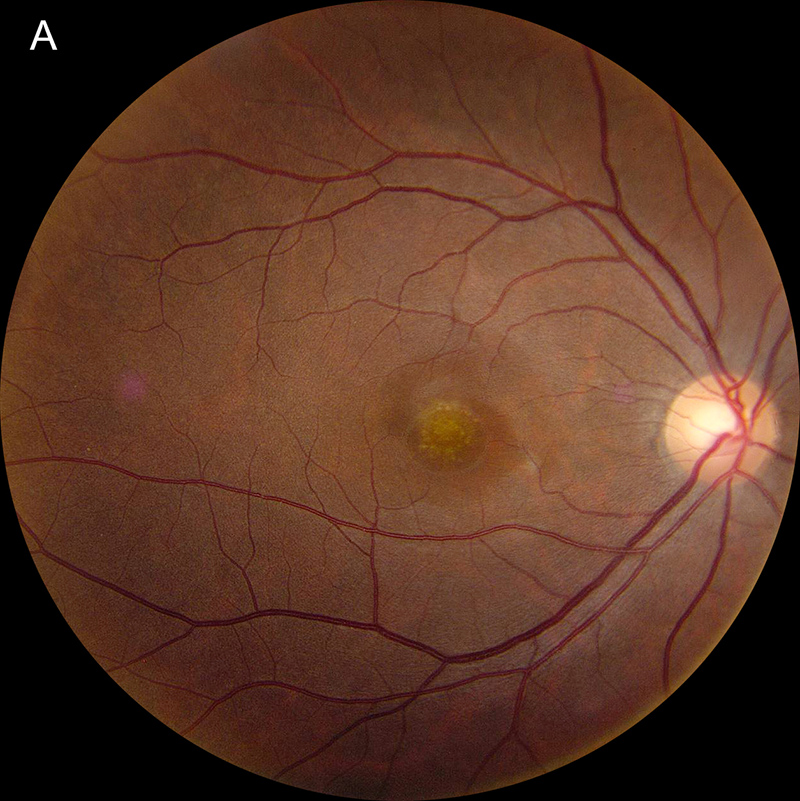
Figure 1A: Color photo of the right eye. Note the area of yellowish mottling of the RPE in the fovea.
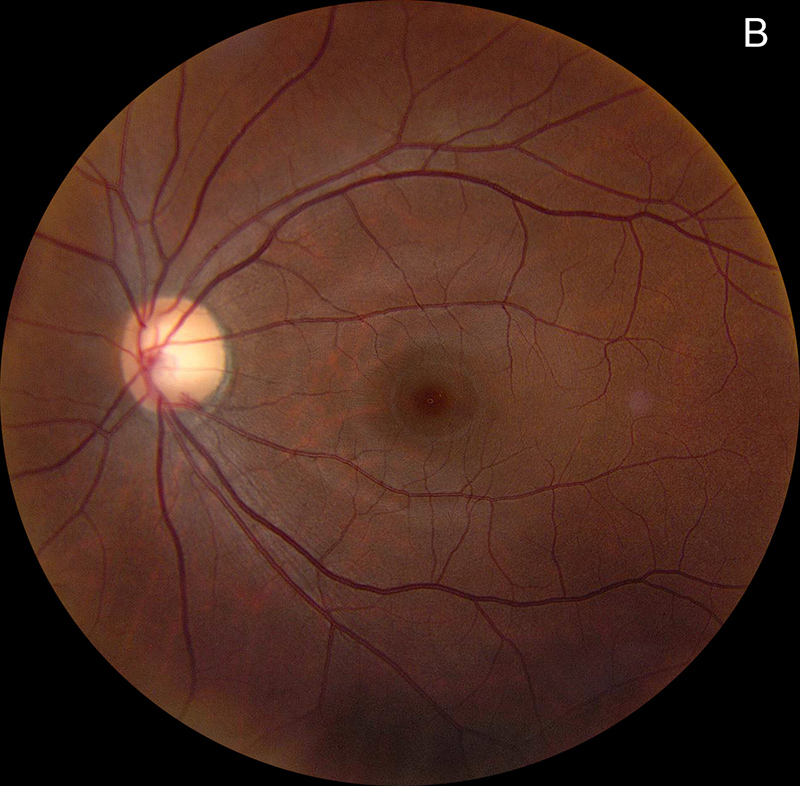
Figure 1B: Color photo of the left eye shows no abnormalities.
The patient noticed a central grey spot in her right eye vision for about 3 weeks duration which slowly progressed. She also described having associated intermittent flashes of light in this eye. She denied any significant past ocular history except for LASIK surgery over 5 years ago to correct her mild myopic refractive error. Her past medical history and family history were unremarkable. She denied smoking or alcohol use. Her review of systems was otherwise negative, with no recent upper respiratory symptoms, skin lesions, or rashes. There were also no young children in her household. She received a COVID-19 vaccine over 5 months prior to her initial presentation.
Her best corrected Snellen visual acuity measured 20/200 in the right eye (OD) and 20/16 in the left eye (OS). Her intraocular pressure was 12 mmHg in the right eye and 15 mmHg in the left eye. Anterior segment examination was unremarkable in both eyes. The funduscopic examination of the right eye showed punctate accumulation of yellow material at the fovea, with an adjacent spot of retinal whitening (Figure 1A). The left eye fundus examination showed no significant abnormalities (Figure 1B). Fundus autofluorescence (FAF) was unremarkable in both eyes (Figures 2A and B).
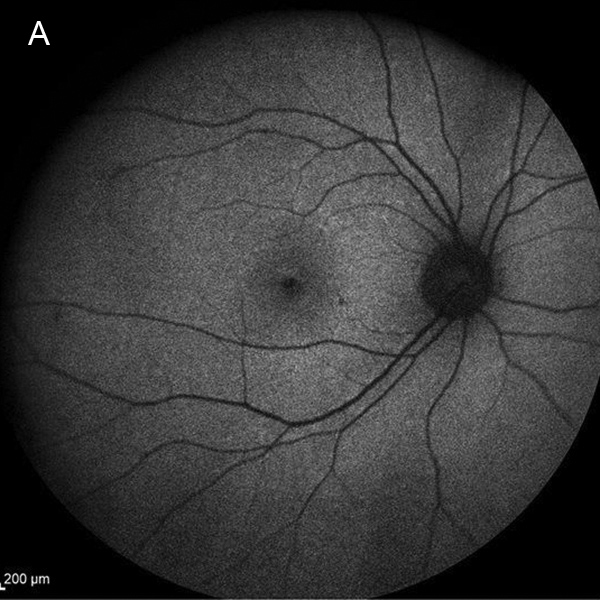
Figure 2A:Fundus autofluorescence of the right eye showed no abnormal fluorescence.
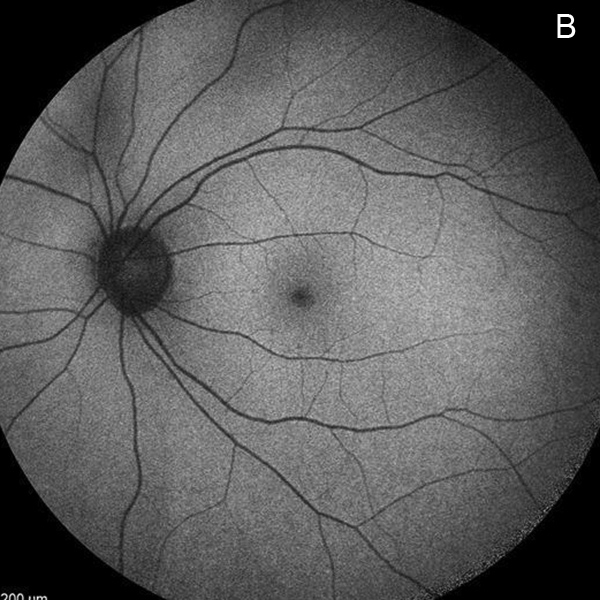
Figure 2B:Fundus autofluorescence of the left eye showed no abnormal fluorescence.
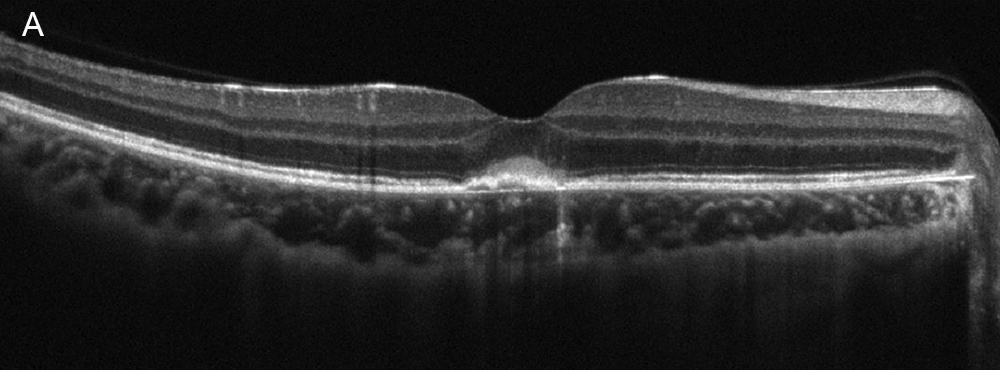
Figure 3A:Spectral-domain OCT of the right eye. Note the subretinal hyperreflective material under the fovea. There are also some increased reflectivity in the choroid.
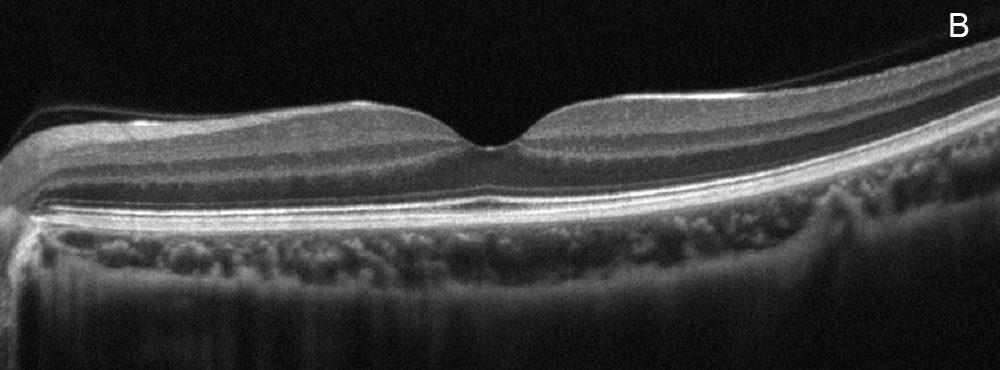
Figure 3B:Spectral-domain OCT of the left eye. This is a normal.
Spectral domain optical coherence tomography (SD-OCT) of the right eye demonstrated central RPE elevation with overlying hyperreflective material, in addition to increased choroidal reflectivity from transmission defects (Figure 3A). There was also slight thickening of the choroid in the right eye compared to the left eye. The left eye OCT showed normal retinal contour and architecture. (Figure 3B).
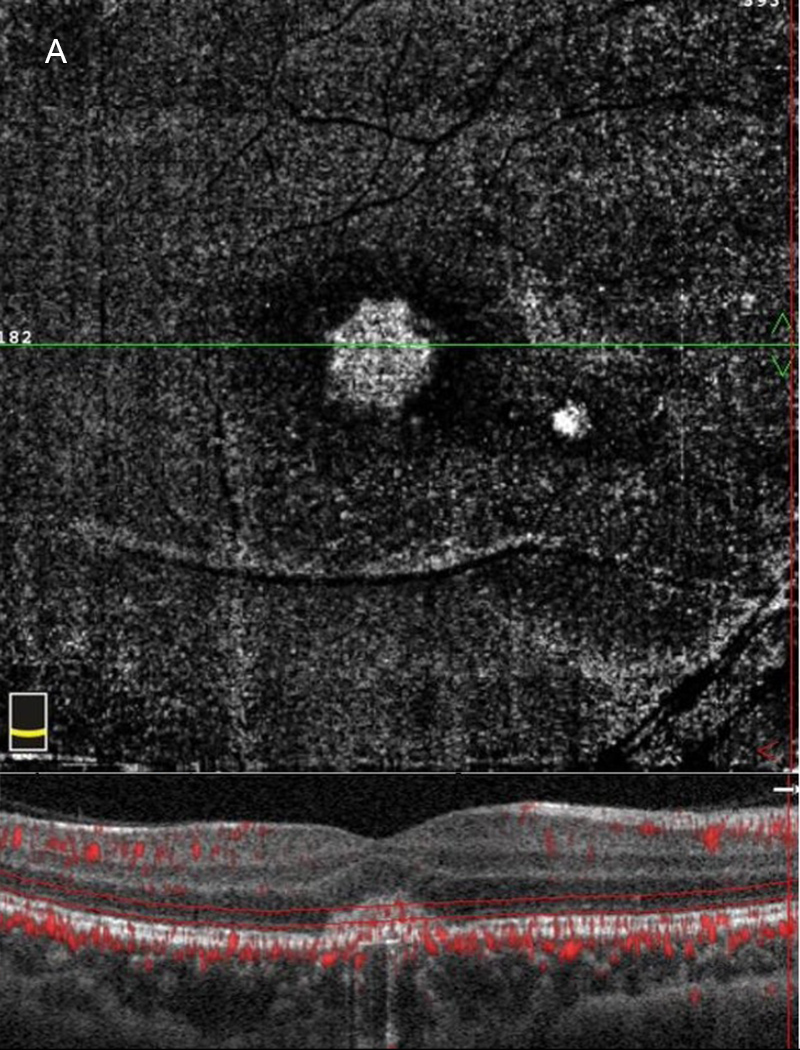
Figure 4A:SD-OCT En face view of the right eye at the photoreceptor level shows an increased signal centrally.
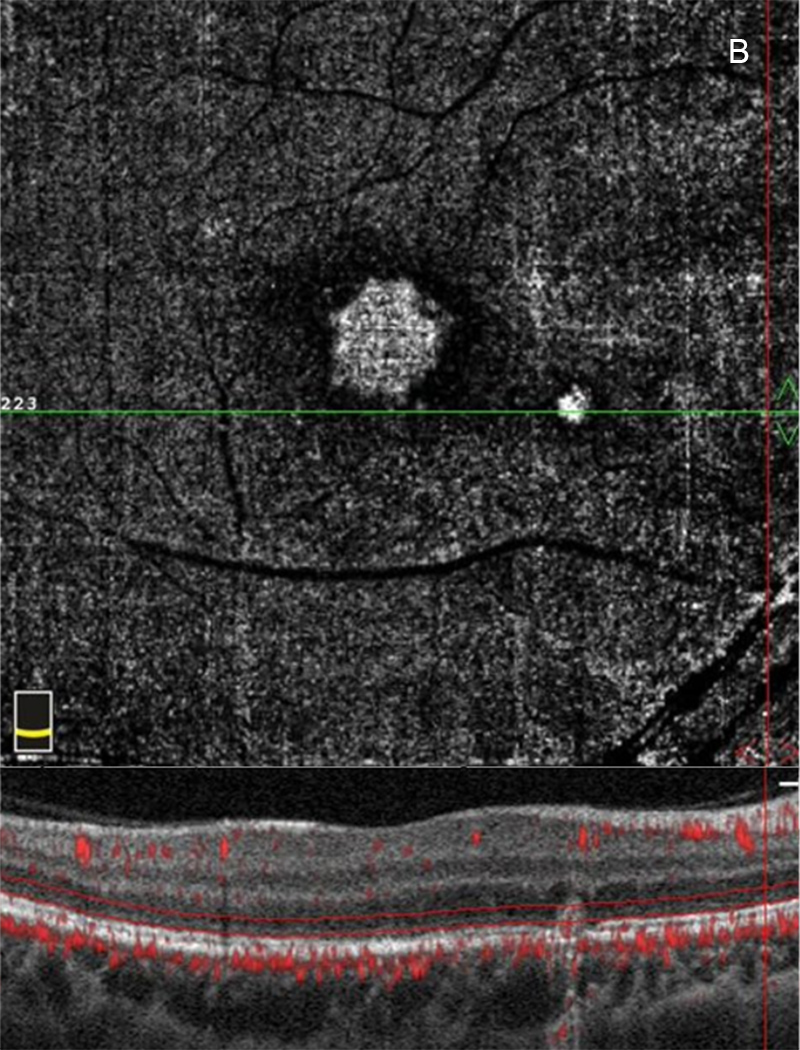
Figure 4B:SD-OCT En Face view of the right macula near the nasal lesion at the level of the photoreceptors shows an increased signal.
OCT-angiography (OCT-A) of the right eye showed two areas of increased reflectivity on the en-face images with the presence of outer retinal vasculature on the associated horizontal B-scans (Figures 4A and B). Fluorescein angiography (FA) revealed a ring-shaped pattern of hyperfluorescence at the fovea OD (Figure 5A) with an adjacent area of focal hyperfluorescence better appreciated in the later phase image (Figure 5B). The left eye FA was unremarkable.
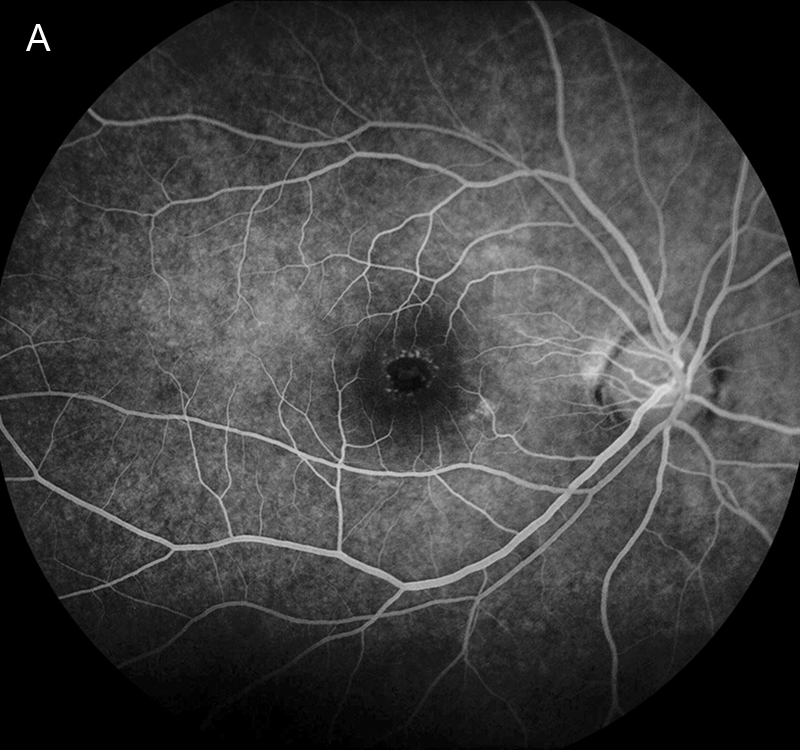
Figure 5A:Fluorescein angiogram of the right eye. Note the ring shaped area of hyperfluorescence in the fovea. There is a touch of icnreased fluorescence centered in the fovea. A bright area is seen inferonasal in the macula.
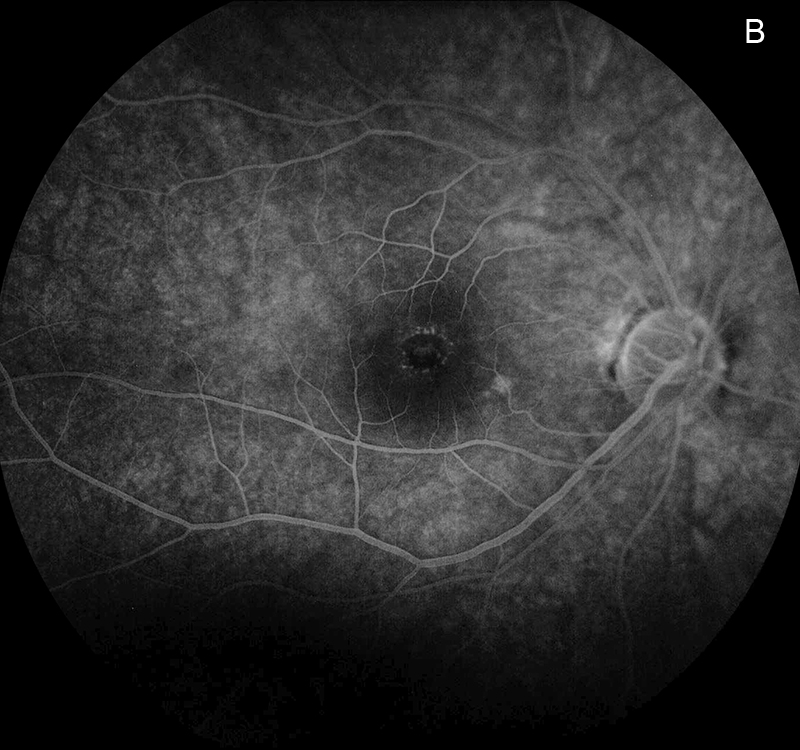
Figure 5B:Fluorescein angiogram of the right eye. No leakage is noted in the later phase of the angiogram.
Differential Diagnosis
Additional History and course
The patient was seen by another ophthalmologist 16 days before her initial presentation to our office. OCT of the right eye during that visit showed the presence of subretinal fluid adjacent to the area of hyper-reflectivity at the fovea (Figure 6A). The fluid had resolved 3 days before she was seen in our clinic (Figure 6B), without having undergone any type of intervention or treatment. Our initial impression was choroidal inflammation related to PIC, and the patient was started on 40 mg of oral prednisone. UAIM was also consider and Coxsackie virus testing was done, which later returned negative.
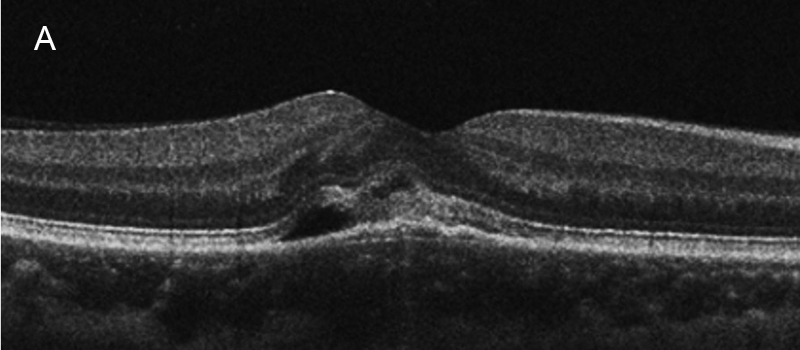
Figure 6A:SD-OCT of the right macula 16 days prior to presentation in our office. Note the subretinal fluid and hyperreflective material.
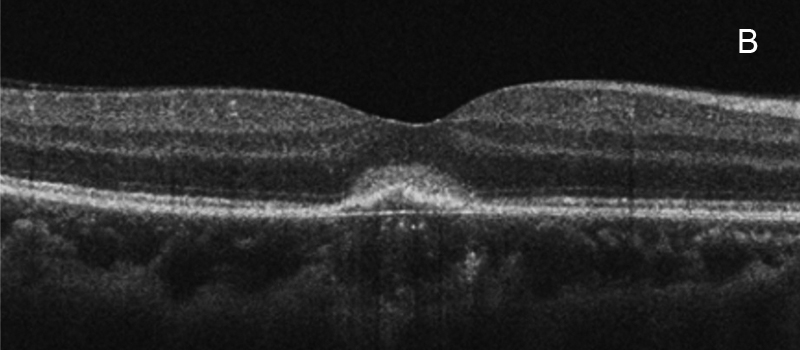
Figure 6B:SD-OCT of the right eye 3 days prior to presentation in our office. The subretinal fluid has resolved, but subretinal hyperreflective material is present.
The patient returned 2 weeks later with slight objective improvement in her visual acuity (20/125) and reduction in the abnormal foveal hyper-reflectivity (Figure 7). She was tapered to 30 mg of prednisone at this time and seen 2 weeks later with no significant change in her vision or OCT (Figure 8). Due to the lack of clinical improvement on steroids, she received an intravitreal injection of Avastin for possible occult CNVM and was tapered to 20 mg of prednisone.
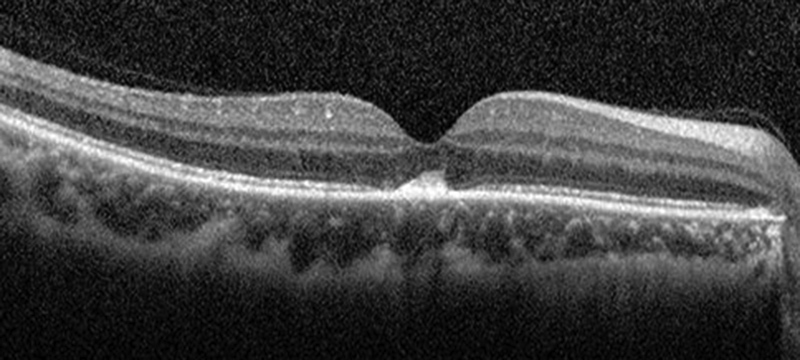
Figure 7:SD-OCT of the right eye 14 days after presentation. She was currently taking 40mg Prednisone at this time.
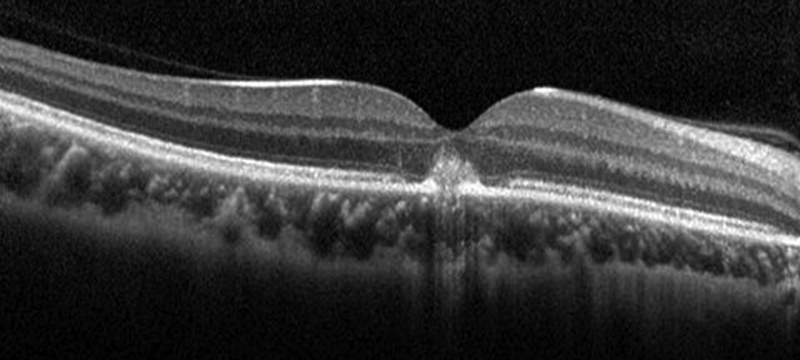
Figure 8:SD-OCT of the right eye 28 days after presentation. She was currently taking 30mg Prednisone. Because of no improvement in her vision, she was given an intravitreal Avastin injection.
We continued to taper the steroids and her clinical course remained unchanged, with only mild improvement in OCT and acuity (20/80) by the 3-month follow up visit (Figure 9). Her fundus exam showed improvement in the yellow material located at the fovea (Figure 10). Her steroids have now been discontinued and she will be returning for continued monitoring and additional anti-VEGF therapy.
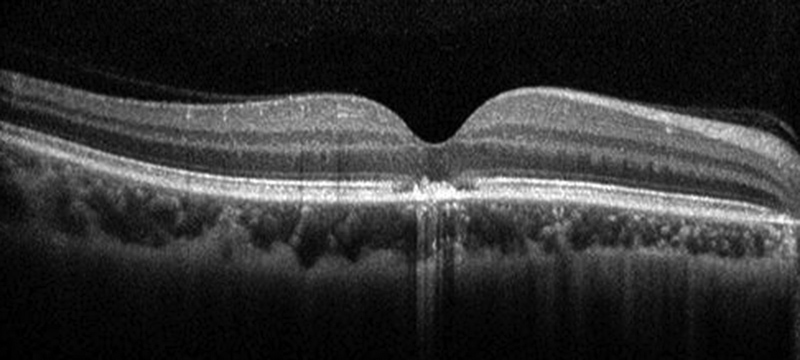
Figure 9: SD-OCT of the right eye 3 months after presentation. She was currently taking 5mg Prednisone and had received an intravitreal Avastin 9 weeks earlier.

Figure 10: Color photo of the right eye. Note the improvement in the yellowish appearancee.
Discussion
This case was presented at the Yannuzzi Rounds hosted by the International Retinal Imaging Society in December of 2021 with discussion focused on the diagnosis of PIC vs UAIM. Throughout the discussion various points were made favoring both diagnoses, however, a majority of the expert panelists felt the ancillary testing and clinical course was more consistent with PIC. Unilateral findings in a young woman may be found with either diagnosis, but our patient was a myope with choroidal thickening in the affected eye, favoring the diagnosis of PIC. The patient’s OCT showed RPE thickening and a neurosensory retinal detachment which is commonly seen in UAIM, however the presence of RPE separation from Bruch’s membrane was felt to be more consistent with PIC. There was also hyper-reflective material under the RPE that likely represented inflammatory debris from PIC. One of the strongest arguments of the discussion involved the presence of a second lesion that was noted at the nasal macula, which is typical for PIC, but not for UAIM. Despite having negative Coxsackie lab results, UAIM was still high on our differential, as it may be caused by a number of different viruses. However, our patient did not demonstrate any upper respiratory or prodromal symptoms prior to her initial presentation.
The patient’s OCT-A images created discussion about presence of choroidal neovascularization (CNV), and if there was actual true flow from CNV membranes overlying the RPE versus pseudo-flow. There was a possible break in the RPE noted on one of the OCT images which could have allowed for neovascularization (Figure 11).
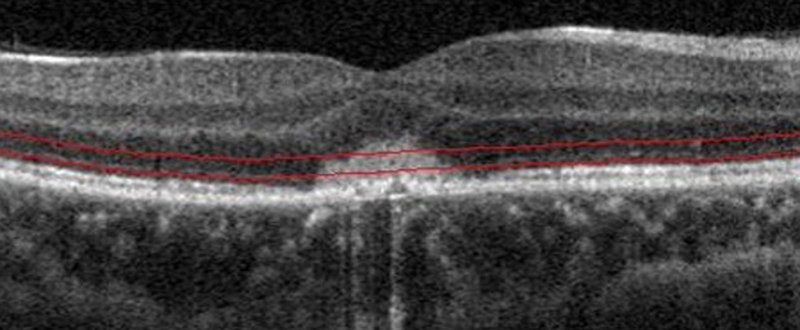
Figure 11: OCT of the right eye. Note the apparent small defect in the RPE.
CNV can occur in both UAIM and PIC but does not usually occur until the very late phases in UAIM, but may appear sooner in PIC if there is an inflammatory break in the RPE/Bruch’s membrane. Because there was no definite evidence of CNV when we first saw the patient, we treated her with oral steroids alone. We held anti-VEGF treatment at that time in order to see the patient’s response to monotherapy. Her symptoms and exam did not worsen over time, but Avastin was later administered due to lack of improvement with the steroids alone. She did demonstrate a slight subjective and objective improvement after receiving the Avastin, which further complemented our suspicion for CNV associated with PIC. Our plan is to continue monitoring this patient with OCT-A and treat with anti-VEGF therapy on an as needed basis.