July, 2020
Presented by Caleg Ng, MD


Presented by Caleg Ng, MD

A 63-year-old Caucasian female patient is referred for evaluation of persistent floaters and photopsias in the left eye.

Figure 1A: Wide-field color photo of the right eye. No lesions are present.

Figure 1A: Wide-field color photo of the left eye. Note the multiple creamy lesions scattered nasally and superiorly.
Our patient reported that she had received an epidural corticosteroid injection for treatment of sciatic pain four months earlier. She noted onset of floaters and photopsias several days later. Her past medical history included treatment for lichen psoriasis managed with topical corticosteroid cream and colon cancer treated with colectomy 24 years ago. She had undergone three cesarean sections and a total abdominal hysterectomy 18 years prior for a bleeding uterine cyst. Her only prescription medication was estradiol. Family history was remarkable for cutaneous malignant melanoma in her mother and multiple myeloma in her father. Her social history was insignificant.
Her best corrected Snellen visual acuity measured 20/20 right eye (OD) and 20/20 left eye (OS). No afferent pupillary defect was noted, confrontational visual fields were full, and intraocular pressures were 10 mmHg OD and 13 mmHg OS. Anterior segment examination was unremarkable in the right eye, but we noted the presence of rare cells in the anterior chamber of the left eye. The posterior segment of the right eye was normal (Figure 1A). In the left eye, 1+ cells in the anterior vitreous were noted. Examination of the retina showed creamy, placoid lesions in the superior and nasal mid-periphery (Figure 1B). Fundus autofluorescence imaging was normal in the right eye and showed mild increased autofluorescence of the creamy pale lesions (Figures 2A and B). Fluorescein angiography was normal in the right eye and showed mild leakage in the area of the creamy lesions as well as some mild perivascular leakage (Figures 3A and B). Indocyanine angiography of the right eye was normal, but showed hypocyanescence of the lesions in the left eye (Figures 4A and B). Enhanced depth spectral domain optical coherence tomography of the lesions revealed normal retinal architecture with a thickened choroid and loss of normal choroidal vascular pattern. (Figures 5A and B).
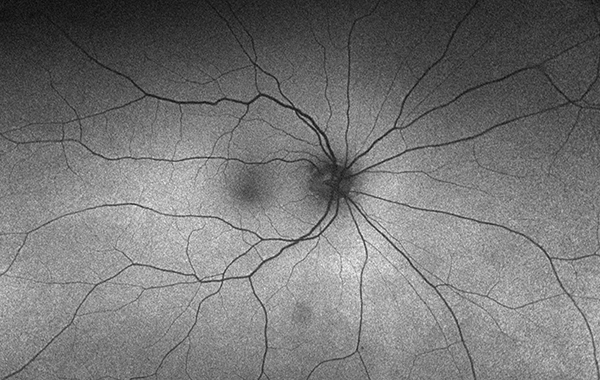
Figure 2A: Wide-field fundus autofluorescence of the right eye. No abnormal autofluorescence is present.
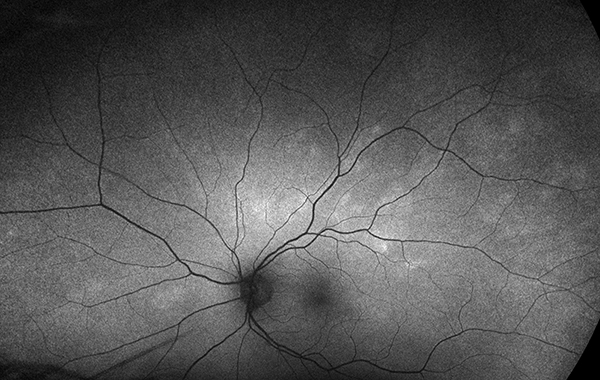
Figure 2B: Wide-field fundus autofluorescence of the left eye. Mild increased autofluorescence is noted in the areas of the creamy lesions.
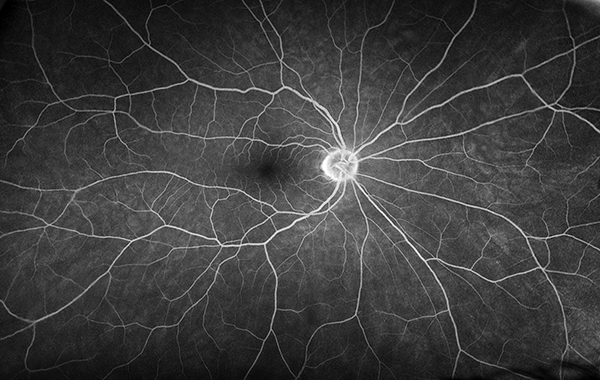
Figure 3A: Wide-field fluorescein angiography of the right eye showed a normal study.
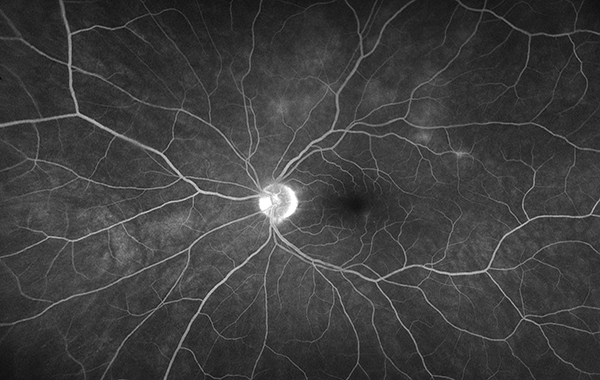
Figure 3B: Wide-field fluorescein angiography of the left eye showed mild leakage in the areas of the creamy lesions and mild vasculitis.
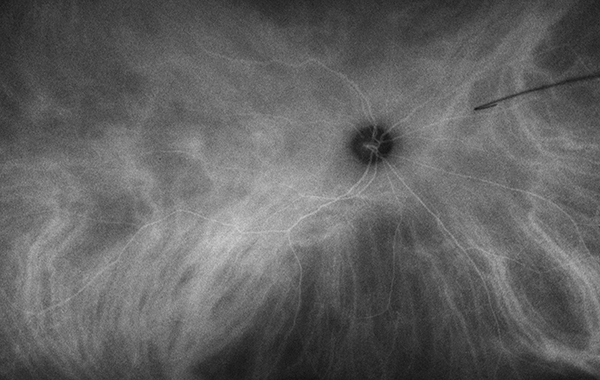
Figure 5A: Wide-field indocyanine angiography of the right eye showed a normal study.
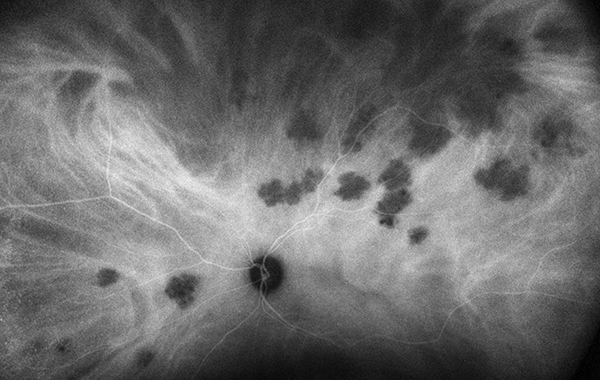
Figure 4B: Wide-field indocyanine angiography of the left eye. Note that the areas of the creamy lesions are hypocyanescent.
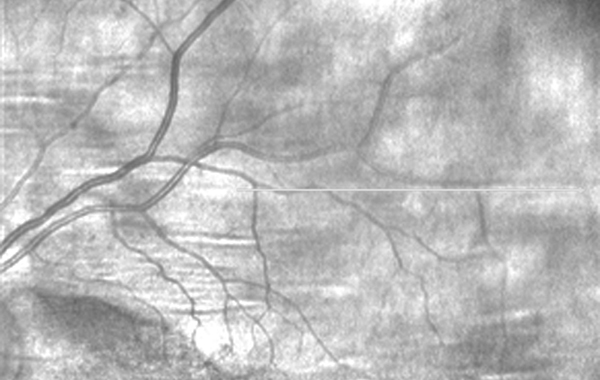
Figure 4A: OCT scan image showing area of scan (Figure 5B) along superotemporal arcade.
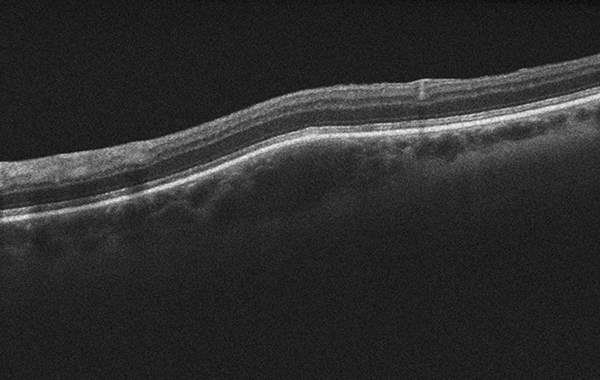
Figure 5B: OCT scan of lesion showing elevation and deep choroidal involvement. No overlying subretinal fluid is present.
Differential Diagnosis
Choroidal lymphoma, sarcoidosis, miliary tuberculosis, choroidal metastasis
Additional History and Diagnosis
Lab testing including CBC, metabolic panel, SPEP, ESR, ANA, Lysozyme, ACE, VDRL, and quantiferon gold were unremarkable. A full body PET CT scan revealed extensive, relatively symmetric hypermetabolic lymphadenopathy in the bilateral mediastinum and bilateral hila. Hypermetabolic lymph nodes were also present in the bilateral lower neck. Our patient’s diagnosis was narrowed down to sarcoidosis or lymphoma. A needle core biopsy of a cervical lymph node revealed fibrous tissue with epithelioid histiocytes and multinucleated giant cells, consistent with non-necrotizing granuloma formations; there were minimal lymphocytes. Grocott’s methenamine silver and acid-fast bacilli staining did not reveal fungal and acid-fast positive organisms, respectively. Immunostain for CK AE1/3 returned negative, making metastatic carcinoma highly unlikely. Patient was given the diagnosis of definite ocular sarcoidosis. We recommended observation of the choroidal lesions given the patient's preserved visual acuity. The lesions spontaneously became more and more faint and completely resolved by five months.
Discussion
Sarcoidosis is a chronic inflammatory disease of uncertain etiology that affects multiple organ systems. While patients of any race or age can be affected, sarcoidosis most frequently occurs during the third to fifth decades of life and has been shown to have significantly higher prevalence in Scandinavian, African American, and Irish populations.1,2 The frequency of ocular involvement in various cohorts has varied from as low as 10% to 70%.1-3 A large series based in the United States found that 11.8% of patients with biopsy proven sarcoidosis also possessed ocular signs at 10 months of follow up.4
Sarcoidosis has been called the great imitator for its diverse profile of possible ocular manifestations.1-3 The 1st International Workshop on Ocular Sarcoidosis met in Tokyo in 2006 to define the diagnostic criteria for ocular sarcoidosis.5 Seven ocular clinical signs (Table 1), five diagnostic tests (Table 2), and diagnostic labels based on various combinations of signs and tests (Table 3) were outlined. Presence of non-caseating granulomas on biopsy of lymph nodes, conjunctiva, salivary glands, or lacrimal glands is the only way to diagnose definite ocular sarcoidosis.6-8 Of note, a high frequency of anterior uveitis (70-75%) has been reported in studies where a majority of patients were black.2 In contrast, posterior uveitis was more commonly observed in white patients (65%-83%), especially elderly female.2 Vision loss from ocular sarcoidosis is typically caused by cataract, glaucoma, and cystoid macular edema.2,3 Sarcoid lesions generally respond well to topical, periocular, or systemic corticosteroid treatment, but occasionally steroid-sparing immunosuppressive medications are needed.2,3
Table 1: Clinical Signs of Ocular Sarcoidosis5
Table 2: Diagnostic Tests in Suspected Ocular Sarcoidosis5
Table 3: Diagnostic Criteria for Ocular Sarcoidosis5