July, 2021
Presented by Malini Veerappan Pasricha, MD


Presented by Malini Veerappan Pasricha, MD

A 16-year-old Caucasian male presented with blurry vision in both eyes for the past 8 months.
.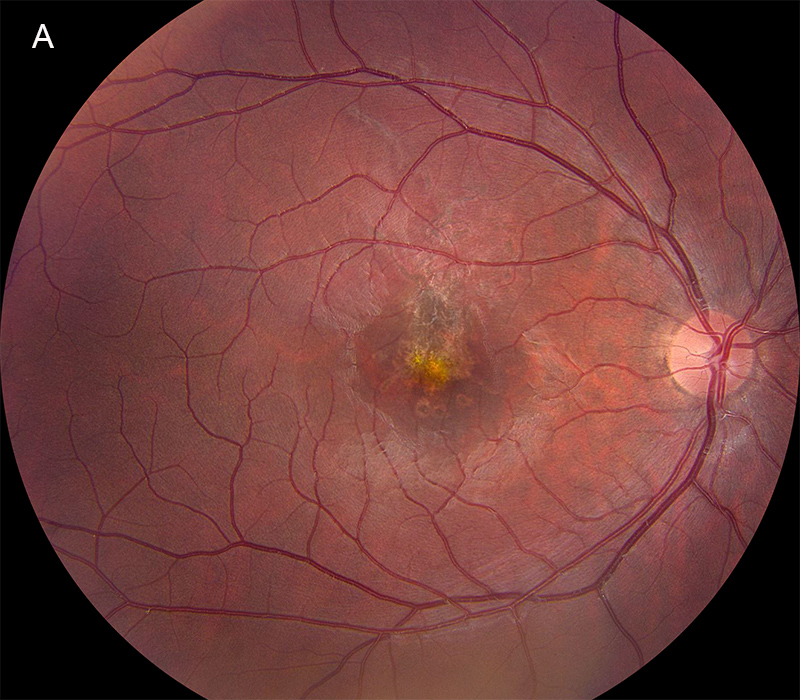
Figure 1A: Color photo of the right eye. Note the pigment disruption in the central macula extending superiorly. The retinal vessels and optic nerve are normal.
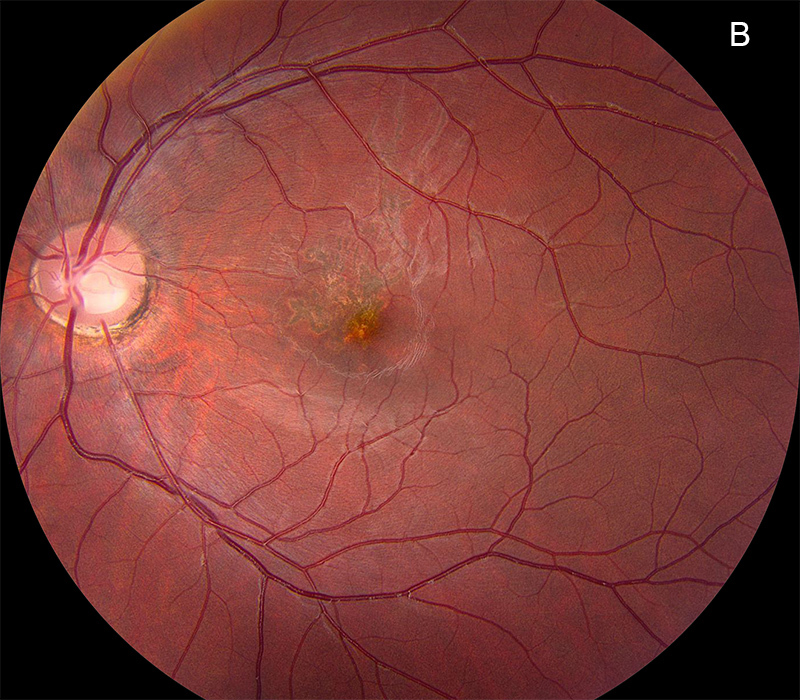
Figure 1B: Color photo of the left eye. There is a less prominent pigment disruption in the central macula extending superiorly.
The patient first noticed a decrease in vision 8 months ago. He described “black blobs” in his vision, that gradually coalesced over time. He denied any floaters or flashes. The patient also denied headaches, metamorphopsia, photophobia, and eye pain. He denied any ocular trauma. His past ocular and medical history were otherwise unremarkable. Family history was non-contributory. He was not taking any medications or using any illicit substances. Review of systems was negative.
On examination, his best corrected Snellen visual acuity measured 20/200 in the right eye (OD) and 20/160 in the left eye (OS). The vision did not improve with pinhole. His intraocular pressure was 13 mmHg OD and 9 mmHg OS. Anterior segment examination was unremarkable in both eyes (OU). The funduscopic examination of both eyes showed multiple well-demarcated gray lesions with surrounding white halos, ranging from curvilinear to punctate to confluent in shape (Figures 1A and B). These chorioretinal scars demonstrated mixed hyper- and hypo-autofluorescence on autofluorescence imaging (Figures 2A and B) and hyperreflectivity on near infrared-reflectance imaging (Figures 3A and B). Spectral domain optical coherence tomography (SD-OCT) showed retinal pigment epithelium (RPE) disruption and focal ellipsoid zone (EZ) and interdigitation zone (IZ) loss. Hyperreflective lesions extending anteriorly from the IZ towards the outer plexiform layers were also noted on SDOCT (Figures 3A and B). OCT-Angiography of both eyes showed closure of the choriocapillaris (Figures 4A and B).
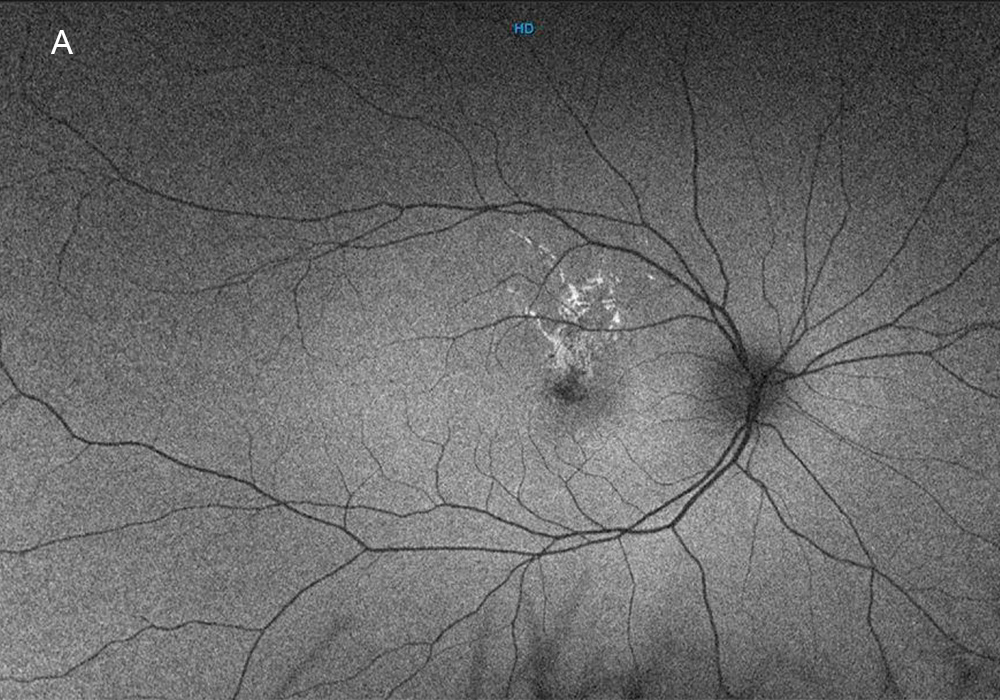
Figure 2A: Wide-angle autofluorescence image of the right eye. The lesions in the macula are mostly hyperautofluorescent.
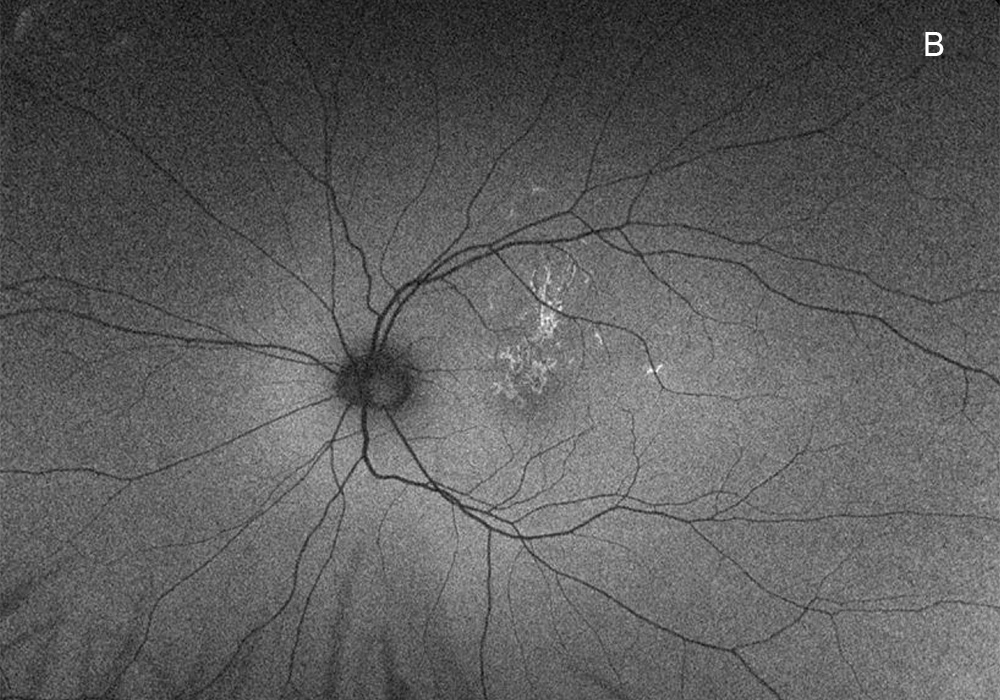
Figure 2B: Wide-angle autofluorescence image of the left eye. The lesions in the macula are mostly hyperautofluorescent.
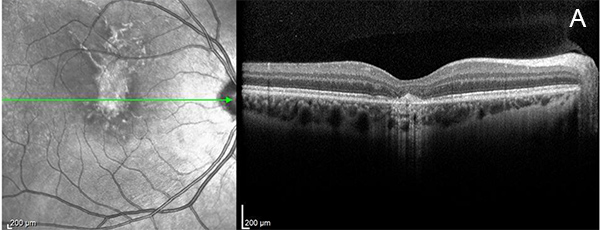
Figure 3A: Near infrared reflectance image and Spectral domain OCT of the right eye. Note hyperreflectie lesions on the near infrared image in and superior the the macula. The OCT scan shows disruption at the level of the RPE and outer retina.
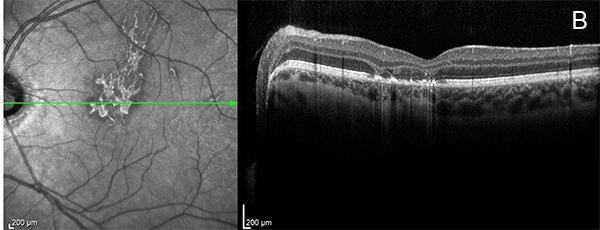
Figure 3B: Near infrared reflectance image and Spectral domain OCT of the left eye. Note hyperreflectie lesions on the near infrared image in and superior the the macula. The OCT scan shows disruption at the level of the RPE and outer retina.
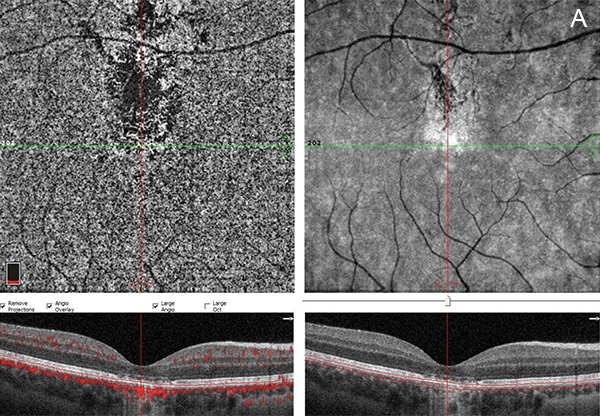
Figure 4A: OCT angiogram of the right eye at the level of the choriocapillaris. Note the closure in the area just superior to the central fovea.
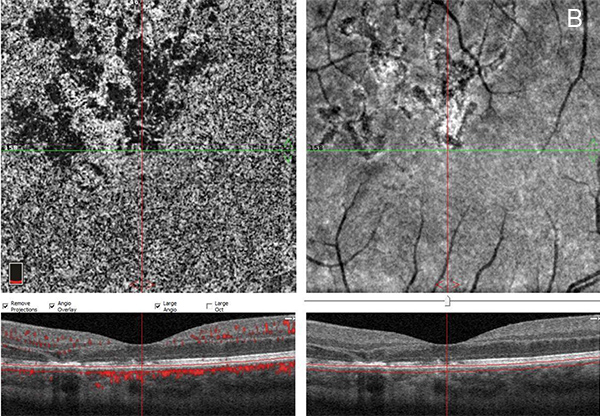
Figure 4B: OCT angiogram of the left eye showing significant closure of the choriocapillaris.
Differential Diagnosis
Additional History
The patient was asked if he owned a laser pointer. He denied, but mentioned that his 13-year-old stepbrother had one. Upon further questioning, the patient stated that he and his stepbrother had been playing with the laser pointer over the last few years – shining it against buildings, windows, and possibly mirrors. He denied sun-gazing or other prolonged light exposures.
Discussion
We describe an adolescent male who presented with paracentral blind spots that gradually became confluent over time. Given the history of laser pointer use and characteristic exam/imaging findings, handheld laser maculopathy is the most likely diagnosis
Powerful light sources, such as sunlight, lasers, and illumination from surgical microscopes, can cause retinal damage and associated vision loss. Handheld laser pointers in particular have become a growing public health concern over the last decade, as they are widely available to the public and relatively inexpensive, especially through the internet.1 While the Food and Drug Administration (FDA) and American National Standards Institute monitor the safety profiles of medical, research, and industrial lasers, handheld lasers for recreational purposes are poorly regulated.2 These lasers are often mislabeled with respect to their power output, and contain inadequate warnings about health hazards.3 A summary of laser classifications and risk of ocular hazard based on laser power output, as detailed in Occupational Safety and Health Administration (OSHA) technical manual, is shown in Table 1.4,5
Table 1
Occupational Safety and Health Administration (OSHA) Summary of Laser Classification and Risk of Ocular Hazard3,4
| Class | Power | Risk of Ocular Injury |
|---|---|---|
| I | 0.4 uW | No |
| IA | 40 uW | Yes if < 1000 sec of exposure |
| II | < 1 mW | Yes if < 0.25 sec of exposure |
| IIIA | 1-5 mW | Yes with any exposure |
| IIIB | 5-500 mW | Yes with any exposure |
| IV | > 500 mW | Yes with any exposure |
Understanding the spectrum of clinical and imaging findings of laser injuries can aid in accurate diagnosis and prompt intervention to confiscate the offending handheld laser. Anterior segment findings that may represent laser-induced injury are corneal punctate epitheliopathy and iris margin atrophy.6,7 However, posterior segment changes are a far more common manifestation of laser-induced ocular injury. Outer retinal abnormalities characterize this condition. Well-demarcated gray or yellow lesions in the macula correspond to the outer retinal phototoxic damage. On SD-OCT, RPE disruption and hypertrophy, and EZ loss are common.8 Bhavsar et al described pathognomonic hyperreflective outer retinal bands, projecting from the RPE or IZ/EZ to the outer plexiform layer. These hyperreflective columns appear to follow the path of photoreceptors and their associated axons (Henle fiber layer) when located close to the fovea.9,10 Peripheral retinal lesions are rare. With regard to timeline of retinal changes, the initial laser insult to the retina produces disorganized RPE changes, which progress over 1-2 weeks to well-demarcated gray or yellow streak lesions. In the following months, RPE and EZ remodeling and regeneration may occur, and lesions may become more confluent. Long-term clinical changes include RPE abnormalities, focal EZ loss, and persistent gray or yellow lesions with hyperpigmentation consistent with chorioretinal scarring.3,11 Previously reported complications of laser-induced retinal toxicity are choroidal neovascularization (CNV), subhyaloid or sub-internal limiting membrane hemorrhage, retinal hemorrhages, macular hole, macular edema, and epiretinal membrane (ERM) formation.12-14
The pathophysiology of laser pointer maculopathy is rooted in thermal damage. The handheld laser emits a large amount of photochemical energy, which the RPE is unable to absorb, resulting in a localized elevation in temperature. This causes free radical formation and tissue oxidation, protein denaturation, and consequent photoreceptor cell death.5 The extent of thermal damage depends on the wavelength, power, duration of exposure, and pupil size. Shorter wavelength, higher power, longer duration of exposure, and larger pupil size are all associated with greater retinal toxicity.2
In a recent review of 171 patients with a diagnosis of handheld laser maculopathy, male children and young adults were identified as the most commonly affected groups.2 Exposure behavior can be broadly categorized as unintentional vs. intentional. Unintentional injury occurs primarily in children, engaged in play behavior with their peers. This demographic is particularly vulnerable to online marketing strategies that portray lasers as toys, for example to burn holes into objects or start fires. Limited gaze redirection and blink reflex compared to adults, injury-prone anatomic features such as clear ocular media, and lack of awareness of the visual consequences of handheld lasers are all contributing factors to retinal injury in this demographic.2 Intentional injury, on the other hand, occurs primarily in young adults with psychiatric comorbidities and behavioral disorders. Attention deficit hyperactivity disorder was reported to be the most common comorbidity, followed by autism.15 History of self-harm, substance abuse, suicide attempts, adjustment disorder, and schizoid personality disorder were other reported comorbidities.2 Psychosocial stressors, such as the death of a loved one or family divorce, were also identified as risk factors. Intentional injury was often associated with more severe macular injury and vision loss.2
Patients with handheld laser maculopathy generally have a good prognosis unless there is significant foveal involvement. Once the diagnosis is suspected, the most important intervention is preventing further injury. First, educating the patient and family about the deleterious effects of handheld lasers is crucial. It is also important to confiscate the laser, or strongly recommend that it be discarded. Laser-induced retinal toxicity can be reported to the FDA to prompt investigation of the manufacturer.5 If intentional injury is suspected, referral to a psychiatrist is warranted. There is no evidence-based medical treatment for laser maculopathy. Oral corticosteroids have been prescribed anecdotally, but there is insufficient data to support their efficacy.8 Surgical treatment for laser-induced macular holes and ERM, as well as anti-vascular endothelial growth factor (anti-VEGF) treatment for CNV have been reported to be effective.5,16
Handheld laser maculopathy can be a difficult diagnosis, given affected patients may purposefully or inadvertently withhold information. The disease entity is often mistaken for posterior uveitis or macular dystrophies, causing patients to undergo extensive workup and delaying confiscation of the offending laser.2 Thus, it is important to recognize the characteristic clinical and imaging findings. In addition to physician intervention, changes are needed from a public health standpoint. Educating the general public and enhancing federal regulation of high-powered handheld lasers is critical to prevent further visual disability in vulnerable populations.1,17
Our patient was agreeable to discussing the laser pointer as the cause of his decreased vision, with his stepmom present. We strongly advised the family to discard the laser pointer. We are having him follow up in two months to evaluate for any new lesions.