June, 2020. Case #132
Presented by Caleb Ng, MD
See Readers Comments below


Presented by Caleb Ng, MD
See Readers Comments below

A 37-year-old female referred for evaluation of left retinal lesion.

Figure 1A: Wide-field color photo of the right eye. Note the areas of myelinated nerve fibers.

Figure 1B: Wide-field color photo of the left eye. Note the vascular lesion in the inferotemporal periphery. Fibrosis is present overlying the area. The feeding vessels show some dilation and tortuoisity.
The patient noted a 1-week history of intermittent floaters and photopsias in the left eye. She was seen by a local optometrist who uncovered a left retinal lesion, and she was referred to our clinic for further diagnosis and management.
Our examination noted a best corrected visual acuity measured 20/16-1 right eye and 20/25 left eye. No afferent pupillary defect was noted, confrontational visual fields were full, and bilateral intraocular pressures were normal at 10 mmHg. Anterior segment exam of both eyes was unremarkable. The funduscopic examination of the right eye revealed myelinated nerve fiber in the inferonasal mid-periphery but was otherwise normal. Examination of the left posterior segment revealed multiple areas of mid-peripheral myelinated nerve fiber and a cluster of telangiectatic vessels with exudation and overlying fibrosis in the inferotemporal periphery. Retinal arteries and veins adjacent to the lesion appeared engorged and more tortuous (Figures 1A and B). Fluorescein angiography revealed early fill at the area of the lesion followed by diffuse leakage in the late phases (Figures 2A and B). Spectral domain optical coherence tomography of the macula was normal (Figure 3). No abnormal hyperautofluorescence was observed (Figure 4).

Figure 2A: Wide-field florescein angiogram of the left eye. Note the area of early hyperfluorescene of the vascular lesion.

Figure 1A: Wide-field florescein angiogram of the left eye. The vascular lesion is showing significant fluorescein leakage.
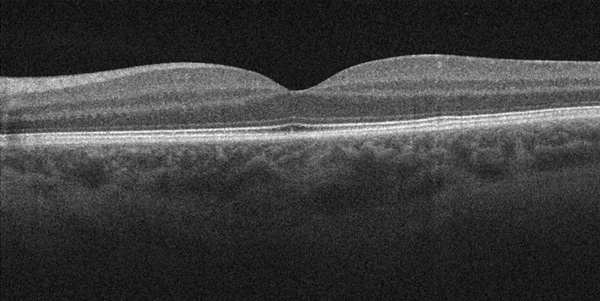
Figure 3: Spectral Domain OCT of the left macula. There is no epiretinal membrane nor macular edema complicating this vascular lesion.
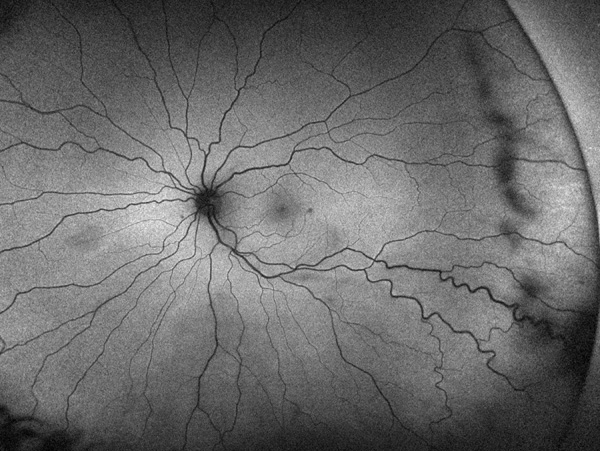
Figure 4: Wide-field autofluorescence of the left eye. There is no abnomral hyperfluorescence in the area of the vascular lesion.
Differential Diagnosis
Addtional History and Diagnosis/Treatment
Our patient had unremarkable medical, surgical, and social history; She denied family history of malignancy, early vision loss, and any occurrence of early and unexplained death. Given our patient’s age, lack of prominent feeder vessels to lesion, as well as benign ocular and family history, we diagnosed her with presumed idiopathic vasoproliferative tumor in the left eye. Patient received treatment with intravitreal ranibizumab 0.5 mg and will receive laser photocoagulation of lesion at a future date.
Discussion
Several clinical series of peripheral telangiectatic nodules were reported by several authors in the early 1980’s,1-3 and were named peripheral retinal acquired hemangioma by Shields et al.3 These lesions tended to be unilateral, located in the inferotemporal periphery, and associated with high incidence of macular pucker. In 1995, Shields and colleagues further expounded on the clinical manifestations of these lesions in a larger series, and suggested that the now more common name of vasoproliferative tumor (VPT).4
Vasoproliferative tumors occur more commonly as idiopathic lesions in (74-80%) of cases, but can also arise as sequelae of pre-existing ocular disease (20-26%), such as pars planitis, retinitis pigmentosa, toxoplasmosis, histoplasmosis, toxocariasis, history of retinal detachment repair, idiopathic peripheral vasculitis, Coats’ disease, retinopathy of prematurity, familial exudative vitreoretinopathy, and idiopathic choroiditis.4,5 These lesions can present at any age, but are most commonly observed in the third and fourth decades of life.4,5 VPT’s are generally yellow-red, ill-defined retinal masses with an overlying vascular network of fine telangiectatic vessels, and a mildly dilated afferent retinal artery and efferent retinal vein.5 Of note, there is an observed predilection of these lesions for the inferotemporal periphery (67%) close to the ora serrata (73%).5 It is important to differentiate these lesions from a retinal hemangioblastoma associated with von Hippel-Lindau disease. In our case, the lesion was isolated, and she had no family or personal history to indicate von Hippel-Lindau disease. Moreover, the lesion appeared more like a VPT lesion as compared with the appearance of VHL angiomas.
The most common associated findings in VPT lesions are sub- or intra-retinal exudation (70%), serous retinal detachment (56%), and dilated feeder vessels (57%). Patients with VPT should also be monitored for formation epiretinal membranes (20-30%) and onset of cystoid macular edema (20-30%) that can result in decreased visual acuity.4,5 Secondary VPT’s are more often bilateral (20% vs 4%), multiple (15% vs 5%), larger, occur at an earlier age, and have worse visual prognosis.5 VPT’s appear ultrasonographically dense and hyperfluorescent in the arterial, venous, and late phases of fluorescein angiography.5
Dr. Lee Jampol, Chicago, IL writes: ‘You only tell one side of the story. Many prominent pathologists like Grossnicklaus and Jakobiec believe these are reactive astroctyic proliferative tumors and not primarily vascular in nature.’
Reply: Dr. Jampol, as always, thank you for your interest and comments. We did not review the pathogenesis of these lesions in our case report. Indeed, there is disagreement as to the origin of these lesions. Histopathologic studies appear to indicate these lesions represent a reactive astrocytic proliferation.12-14 The debate arises from the predominant initial clinical appearance of a vascular lesion. Indeed, the management of these lesions is aimed at reducing this component to reduce exudation and inflammation. Ultimately, it is the pathologist that has the final word in this debate when close histologic examination is undertaken. For more details as to histopathologic studies, as well as for a discussion of the origin of these lesions (and terminology), the interested reader is directed to references 12 and the Letters to Editors (References 15 and 16. Thank you again Dr. Jampol.
Another reader from Saudi Arabia: ‘Thank you for your interesting case. Please why not VPT associated with MF (macular fibrosis) in patient with Straatsma Syndrome?’
Our Reply: Thank you for your comments. Straatsma syndrome consists of ipsilateral myopia, amblyopia, strabismus and myelinated nerve fibers. The etiology of myelinated nerve fibers is not clear. Our patient does indeed have myelinated nerve fibers. These appear to be an incidental finding and not part of a syndrome in this case.