June, 2021
Presented by Braden Burckhard, MD


Presented by Braden Burckhard, MD

A 19 year-old Asian-American female presented with a “blurry spot” in her left eye for 1 week.
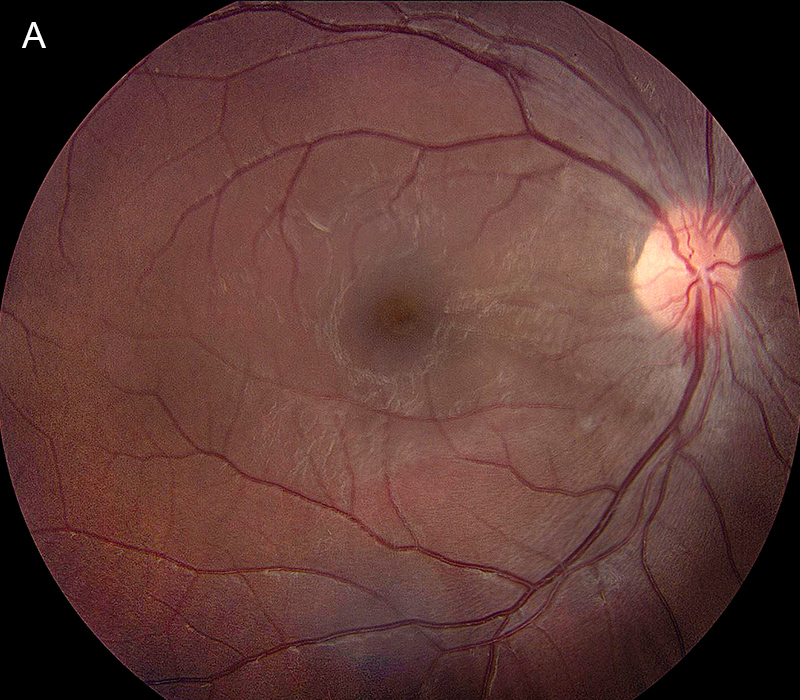
Figure 1A: Color photo of the right eye. Note the mild disc hyperemia, slight blurring of the disc margin and the retinal hemorrhage at the inferior margin of the nerve, and the superotemporal arcade.
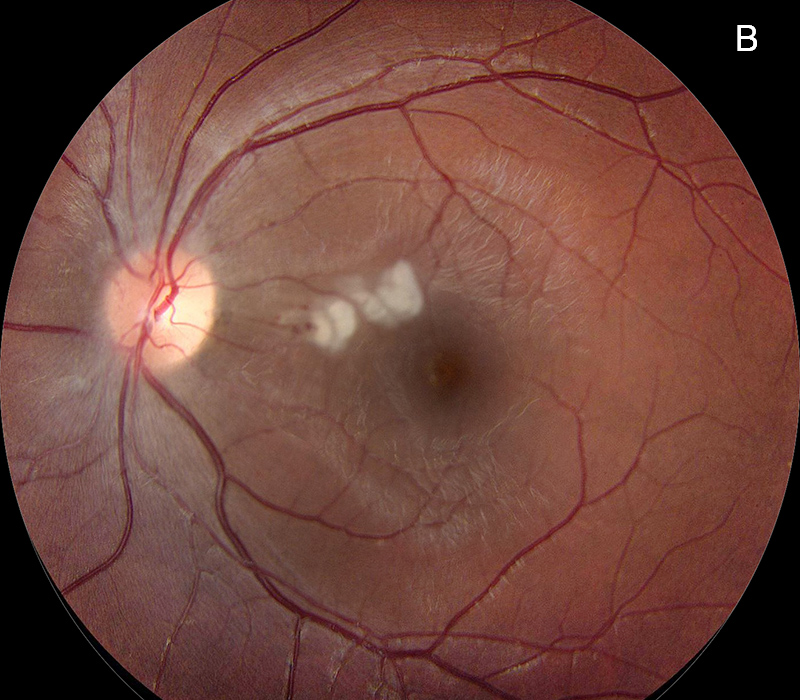
Figure 1B: Color photo of the left eye. Note the inner and deep retinal whitening superonasal to the fovea. There is a small retinal hemorrhage on the nasal side of the retinal whitening.
The patient first noticed a blind spot in her left eye 1 week earlier that remained stable. She also noted having a slight sensation of swelling over the left side of her face and around the eye. She also reported experiencing headaches and mild photophobia over the past 6 months. She denied owning any cats or having any recent exposure. She also denied hearing any “whooshing” noises or any other systemic symptoms. Her past medical history and review of systems were otherwise unremarkable. She was not taking any mediations and has not used any recreational drugs.
Her past ocular history is significant for having a “lazy eye” when she was younger but she could not recall which eye was affected. She denied having any subsequent, long-term vision loss.
Her best corrected Snellen visual acuity measured 20/25 in the right eye (OD) and 20/40 in the left eye (OS). Her intraocular pressures were normal. Anterior segment examination of both eyes was normal. Examination of the right eye showed mild disc hyperemia and slight blurring of the disc margin. There were small flame-shaped hemorrhages at the inferior disc margin and along the superotemporal arcade (Figure 1A). Examination of the left eye revealed mild blurring of the disc margin and inner-retinal whitening just superonasal to the fovea, with an adjacent dot hemorrhage (Figure 1B). Spectral domain optical coherence tomography (SD-OCT) showed exudates and mild nasal thickening in the right eye (Figure 2A). The left eye showed slight hyper-reflectivity in the outer retina of the nasal macula (Figure 2B). There was also both inner and outer retinal hyper-reflectivity corresponding to the white lesions noted on the fundus exam (Figure 2C). Both eyes demonstrated hyperfluorescence and leakage at the disc and peripapillary region (Figures 3A-D).
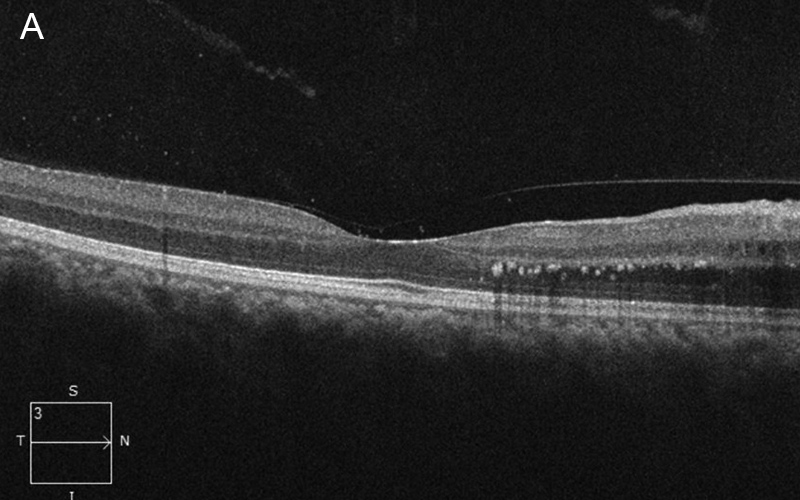
Figure 2A: Spectral domain OCT of the right eye. Note the nasal retinal thickening with deep retina hyperreflective spots.
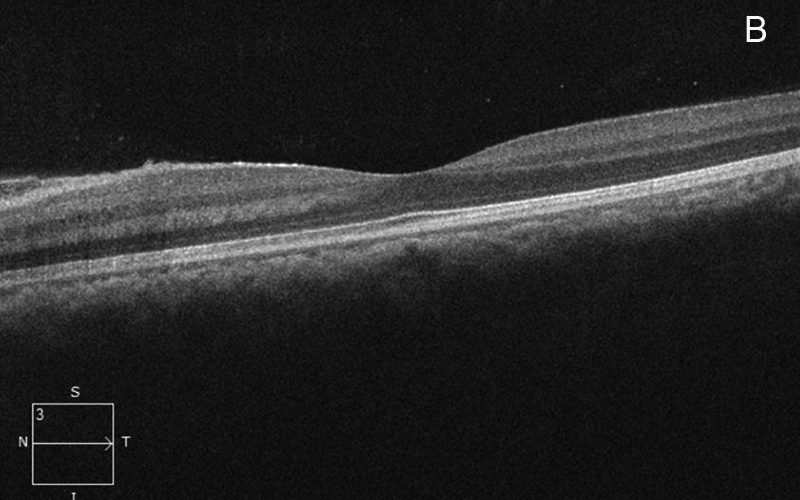
Figure 2B: Spectral domain OCT of the left eye. Note the outer retinal hyperreflective lesions nasal to the fovea.
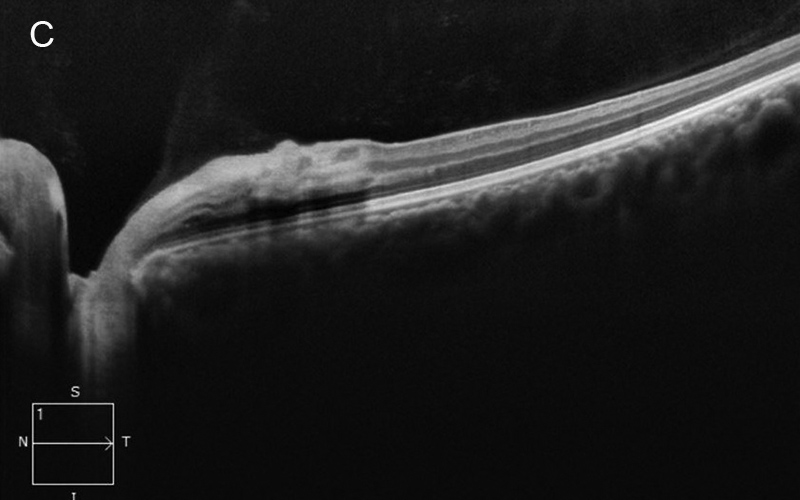
Figure 2C: Spectral domain OCT of the left eye. Note the intense hyperreflective areas corresponding the the retinal whitening noted on the color photos. Outer retina hyperreflective lesions are present nasal to the fovea, as seen in Figure 2B.
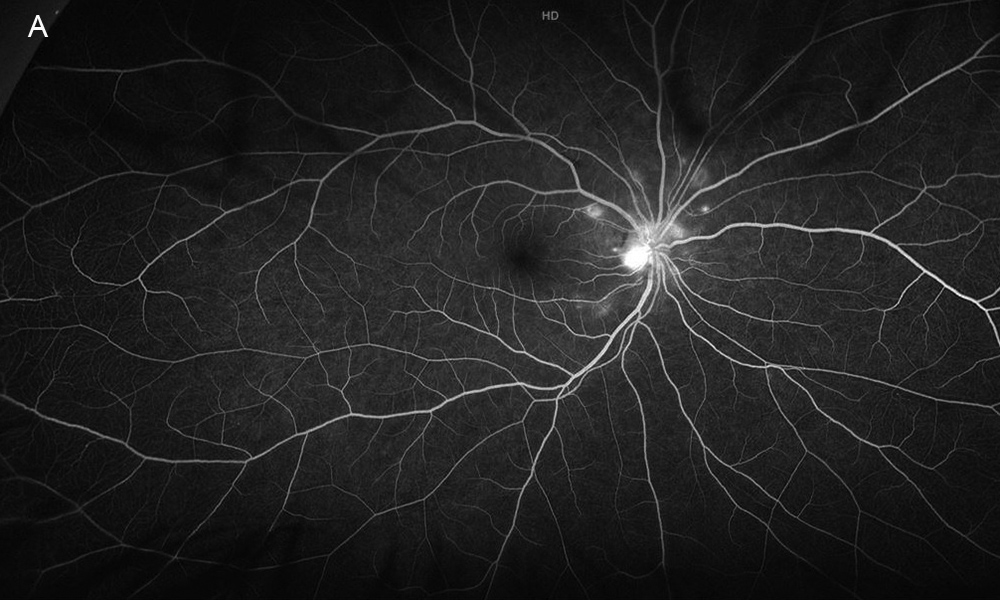
Figure 3A: Wide-field fluorescein angiogram of the right eye. Note the peripapillary areas of early hyperfluorescence.
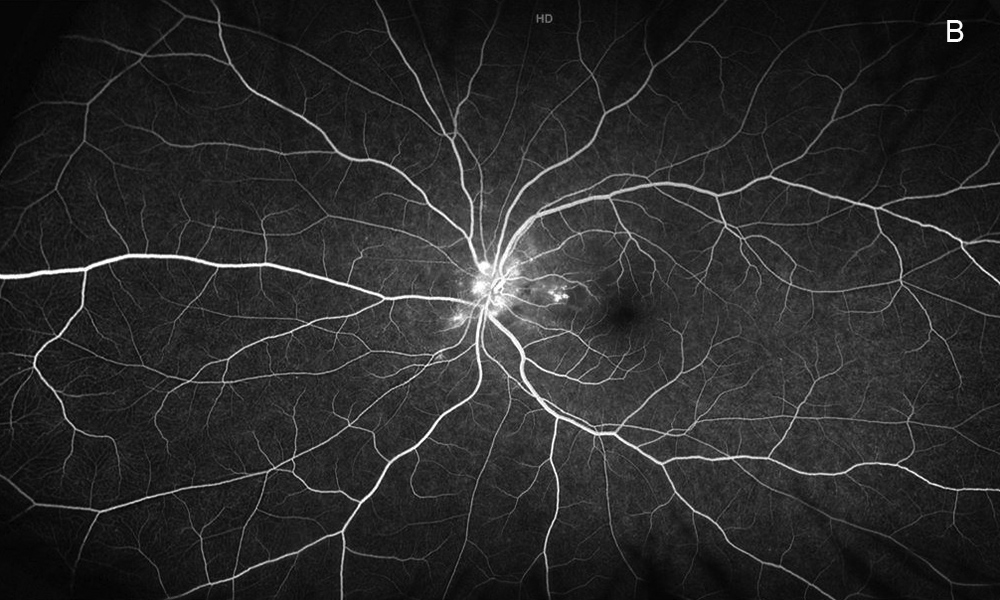
Figure 3B: Wide-field fluorescein angiogram of the left eye. Note the peripapillary areas of early hyperfluorescence as also seen in the right eye.
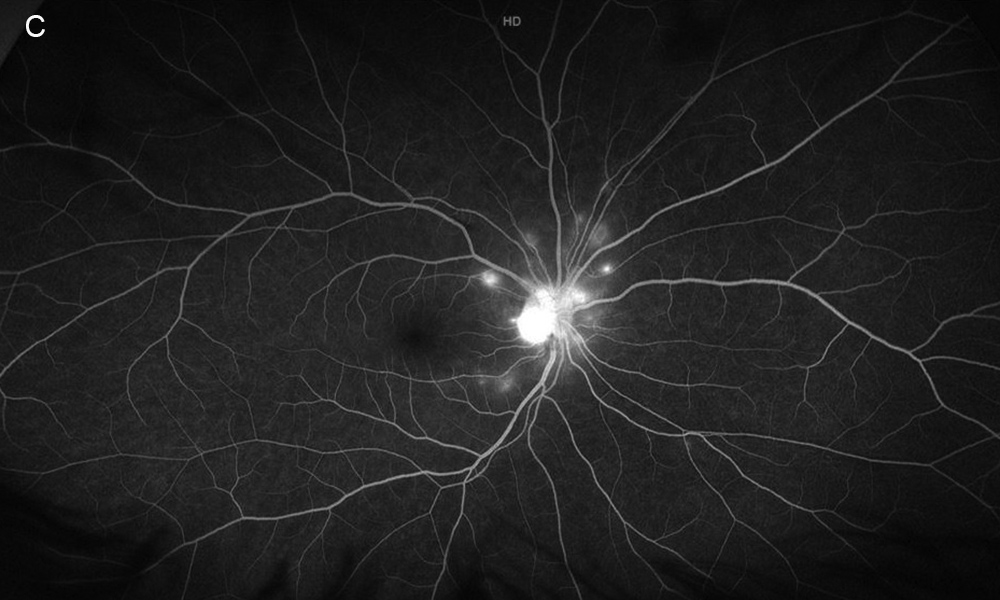
Figure 3C: Late-phase wide-field fluorescein angiogram of the right eye. Peripapllary leakage is present.
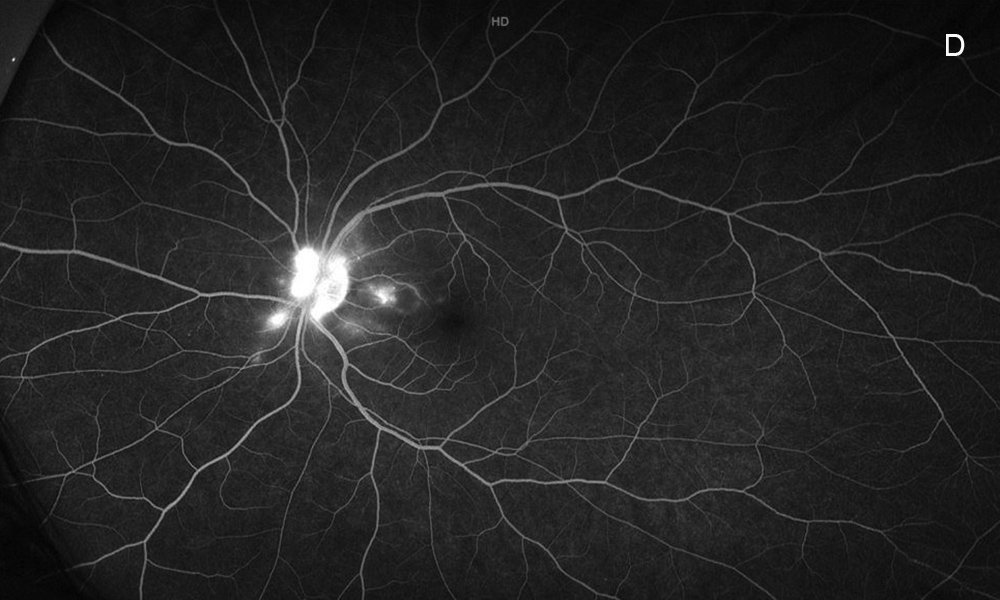
Figure 3D: Late-phase wide-field fluorescein angiogram of the left eye. Peripapllary leakage is present as well as optic nerve leakage.
Differential Diagnosis
Additional History and Patient Course
Due to suspicion for hypertensive retinopathy, the patient’s blood pressure was measured in the clinic and found to be 260/140 mmHg. The patient was diagnosed with hypertensive retinopathy and was referred to a nearby emergency department for further workup and management. She was seen 3 weeks later and her vision had improved to 20/25 in the left eye, with improvement of her subjective symptoms and her fundus examination (Figure 4). After her initial visit to the ED, she had been prescribed 10 mg of lisinopril daily. Her blood pressure at the follow-up visit measured 153/99 mmHg. The underlying cause of her hypertension had not yet been determined.
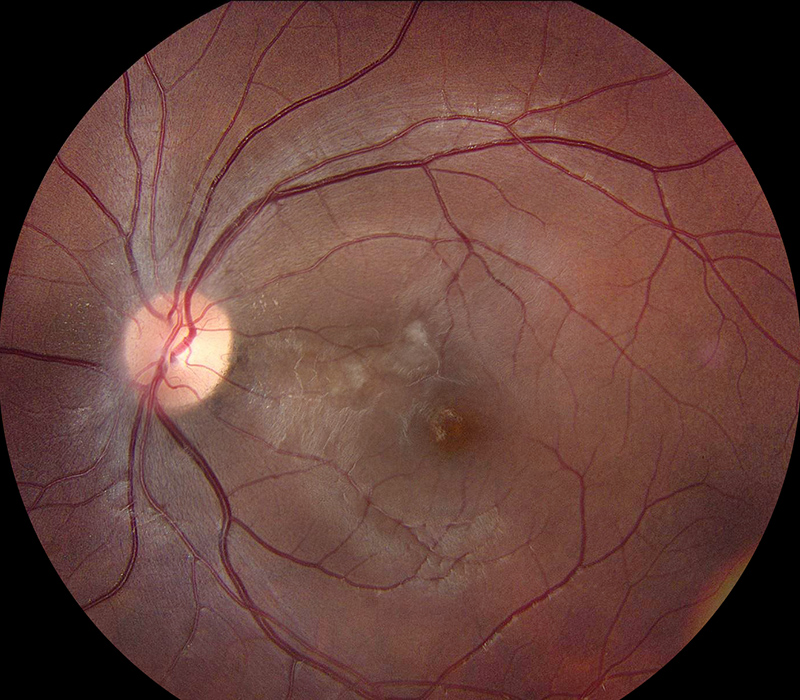
Figure 4: Color photo of the left eye 3 weeks after intial evaluation. Note the resolving area of retinal whitening and intraretinal exudate.
Discussion
Ocular structures particularly susceptible to hypertension include the retina, choroid, and optic nerve. Of these ocular manifestations, hypertensive retinopathy is the most common. The arteriosclerotic changes of hypertensive retinopathy are caused by chronically elevated blood pressure (BP), defined as systolic BP greater than 140 mmHg and diastolic BP greater than 90 mmHg.1 Hypertensive retinopathy may be divided into three different pathophysiologic phases: vasoconstrictive, sclerotic, and the exudative. The disease process has also been classified into four different stages:2
There are other classifications for hypertensive retinopathy, such as those described in the Keith-Wagener-Baker, Scheie, and Modified Scheie systems.
Early detection and management of hypertension is vital in order to prevent systemic complications, especially when a patient is in a hypertensive crisis, usually defined as a blood pressure greater than 180/120 mmHg.
Hypertensive crises are categorized as either hypertensive emergencies or urgencies depending on the degree of BP elevation and presence of end-organ damage. The primary goal of intervention in a hypertensive crisis is to safely reduce BP. Immediate reduction in BP is required only in patients with acute end-organ damage (ie, hypertensive emergency). This requires treatment with an intravenous antihypertensive agent, while severe HTN with no acute end-organ damage (ie, hypertensive urgency) is usually treated with oral antihypertensive agents.3
Our patient was sent to the emergency department immediately after recognition of a hypertensive crisis and she was promptly treated with intravenous antihypertensives follow by daily management with an oral agent. Both her subjective and objective exam improved by her 3-week follow up.