June, 2022
Presented by Malini Veerappan Pasricha, MD


Presented by Malini Veerappan Pasricha, MD

Brief Case Description
A 24-year-old Asian Indian man who is asymptomatic was referred for unusual bilateral retinal lesions.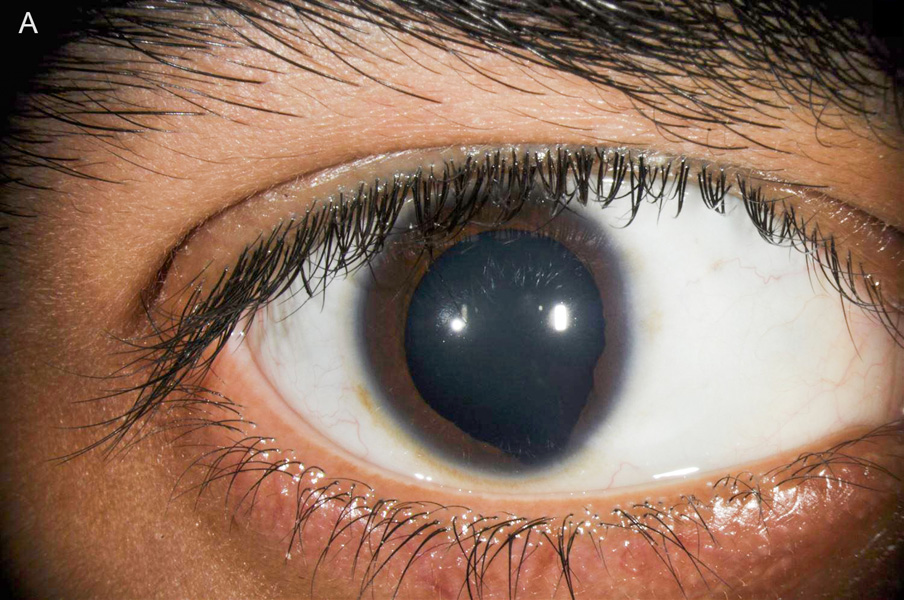
Figure 1A: External photo of the right eye. Note the inferonasal iris defect.
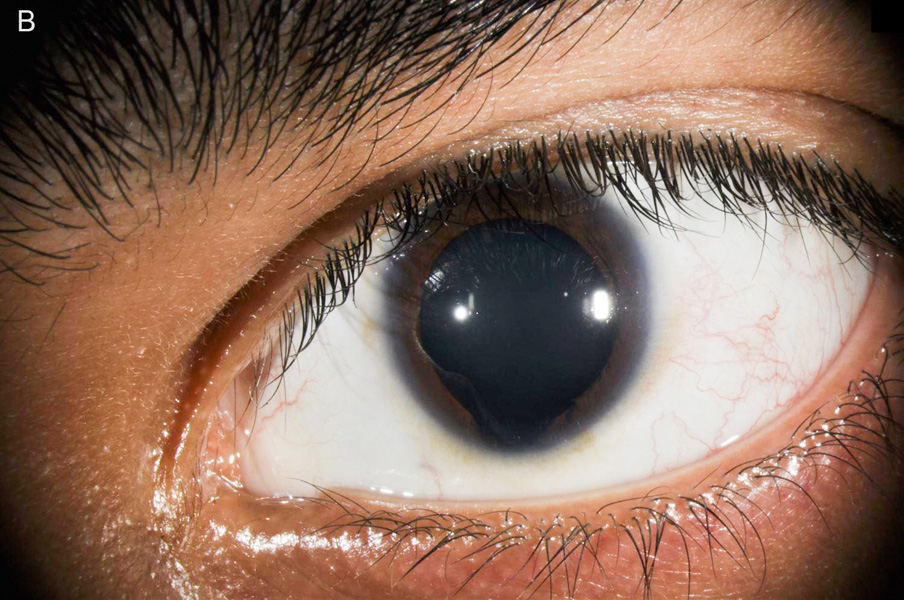
Figure 1B: External photo of the left eye. Note the inferonasal iris defect.
The patient had no acute visual complaints. He reported long-standing superotemporal visual field defects bilaterally. He denied blurry vision, flashes/floaters, metamorphopsia, and photophobia. His past ocular history was significant for high myopia. Family history is noncontributory. He is a current smoker. Review of systems was negative.
The patient’s best corrected Snellen visual acuity measured 20/32 in the right eye (OD) and 20/40 in the left eye (OS). Intraocular pressure was normal in both eyes. Anterior segment exam of the right and left eyes revealed an inferonasal iris defects (Figure 1A and 1B). Posterior segment of the right and left eyes revealed a large chorioretinal lesion involving the macula and the optic nerve (Figure 2A and 2B). Optical coherence tomography (OCT) of both eyes showed an inferior region of absent choroid, with overlying subretinal fluid and schisis-like changes (Figure 3A and 3B).
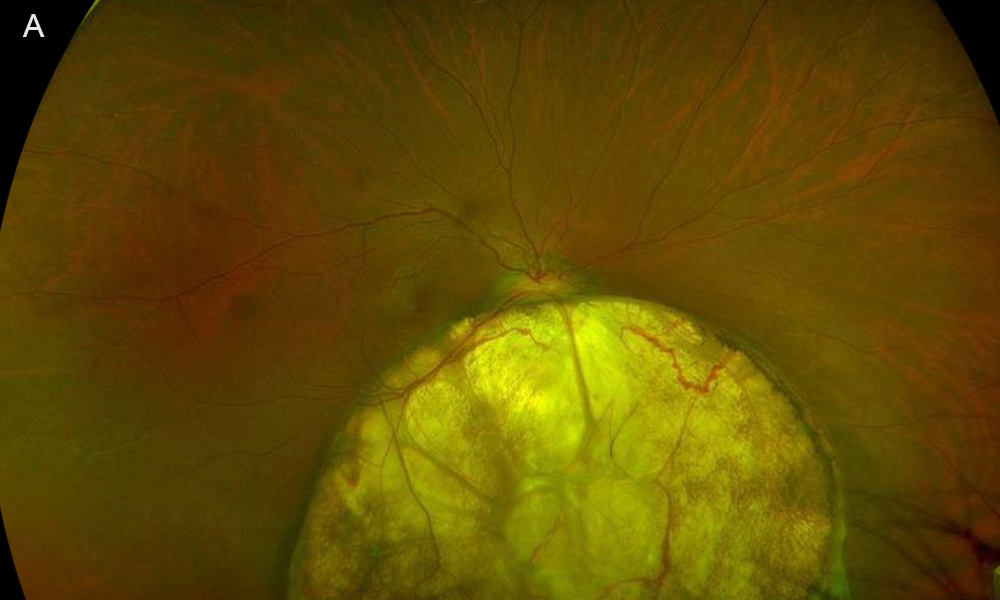
Figure 2A:Fundus photo of the right eye. Note the large circular yellowish lesion below the optic nerve.
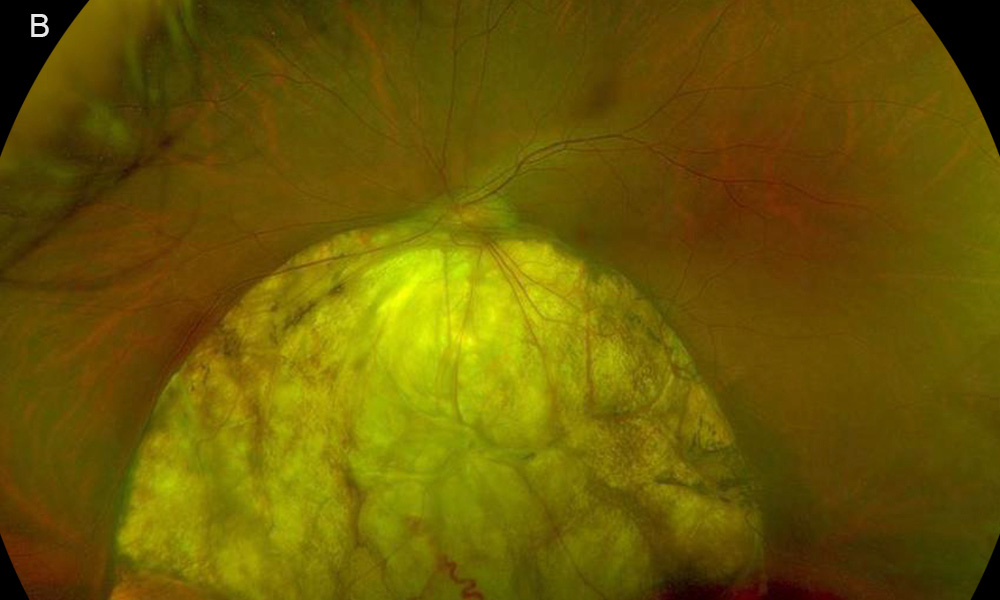
Figure 2B:Fundus photo of the left eye. Note a similar large circular yellowish lesion below the optic nerve.
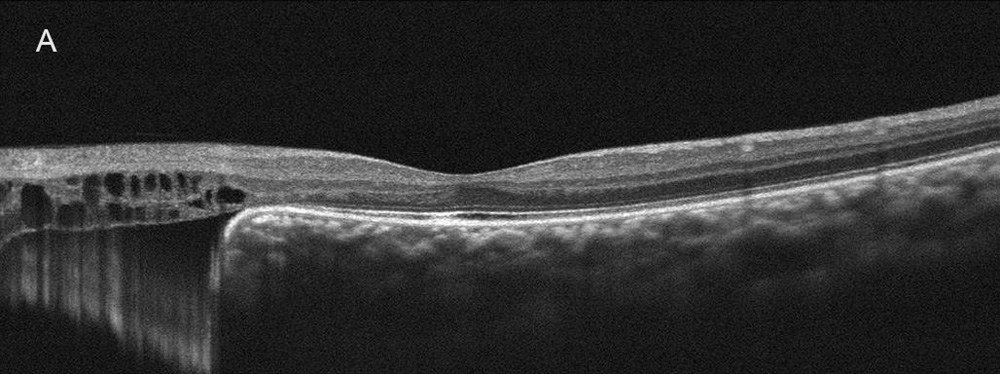
Figure 3A:OCT-SD of the right eye. Scan done vertically through the macula. Inferior to the macula there is absent RPE, bruch's membrane and defect in the choroid. There are retinal cystic changes overlying this area.
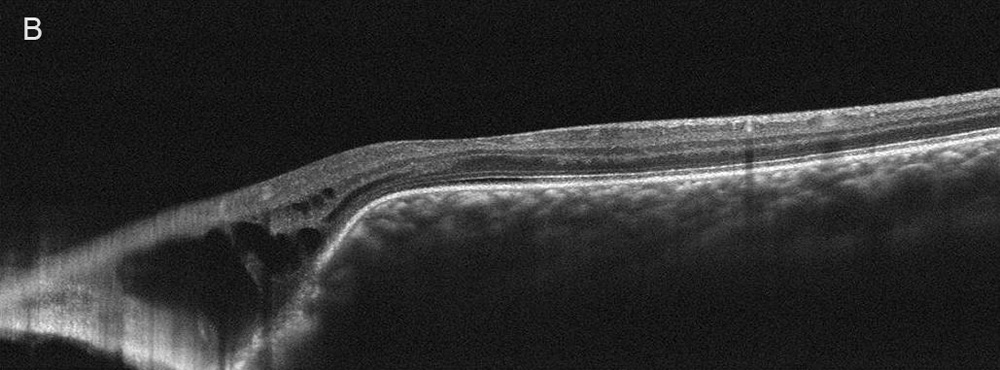
Figure 3B:OCT-SD of the left eye. Scan done vertically through the macula. Similar findings are present in this eye as was seen in the right eye. Inferior to the macula there is absent RPE, bruch's membrane and defect in the choroid. There are retinal cystic changes overlying this area.
Additional History
The patient grew up in India. He reported an uncomplicated birth history. He denied any history of ocular infections or trauma. There was no known family history of inherited ocular diseases, including tumors and colobomas. He reports being previously evaluated in India, though no intervention had been undertaken.
Differential Diagnosis
Diagnosis and Patient Course
The findings on the anterior and posterior segment exam are most consistent with colobomas of the iris, optic nerve, and retina/choroid. There is associated subretinal fluid and schisis overlying the coloboma. This can be due to a retinal break somewhere within or at the margin of the coloboma. The patient has been followed with serial imaging for the last 1.5 years, with no change in exam or symptoms.
Discussion
Prevalence of colobomas is about 2 to 14 per 100,000 births.1 Ocular colobomas arise due to incomplete closure of the optic fissure during the 5th-7th weeks of fetal life.2 They can occur in the iris, ciliary body, lens, retina, choroid and/or optic nerve. The typical location is inferonasal and the majority of eyes are affected bilaterally.1-4 Males and females are affected equally. Vision ranges from normal to no light perception based on the involvement of the optic nerve and macula.1-4 Colobomas can be associated with other ocular abnormalities such as cataract, glaucoma, nystagmus, and microphthalmia.1-4
Colobomas can occur sporadically or from a known genetic defect. If genetic, the most common inheritance pattern is autosomal dominant. Due to the highly variable expressivity, parents may be unknowingly affected.5 Targeted gene panel testing may be considered as part of the workup. Of note, the presence of a coloboma may be syndromic, and prompt systemic evaluation should be undertaken. A commonly associated syndrome is CHARGE (coloboma, heart defects, atresia choanae, growth retardation, genitourinary abnormalities, ear abnormalities).1-4
The appearance of a chorioretinal coloboma is white in color due to the lack of choroid, retina and retinal pigment epithelium and almost bare sclera showing through with only an overlying transparent intercalary membrane derived from undifferentiated neurosensory retina.6 Complications of chorioretinal colobomas include progressive retinal detachment beyond the coloboma and choroidal neovascularization, typically at the margin of the coloboma nearest to the fovea. The rates of retinal detachment are estimated between 23 and 42%.1-4 Interval monitoring for retinal detachment should be performed every 6 to 12 months with a dilated fundus exam.
Retinal detachment associated with colobomas are difficult to manage. Prophylactic laser photocoagulation may reduce the occurrence of retinal detachment.7-8 If a retinal detachment beyond the coloboma margin has occurred, it is likely due to a retinal break within or near the margin of the coloboma. Vitreoretinal traction, schisis, glial atrophy, and exudation from abnormal blood vessels also likely play an important role in these cases.1-4 Successful repair of the detachment can be accomplished by vitrectomy, intravitreal gas or silicone oil, and endolaser treatment along the edge of the coloboma.9-12 Numerous studies have shown that silicone oil tamponade is more effective than gas in reducing the risk of recurrent detachment.9-12