March, 2020
Presented by Michelle Peng, MD


Presented by Michelle Peng, MD

A 57-year-old African American woman presented with worsening blurred central vision in the left eye.
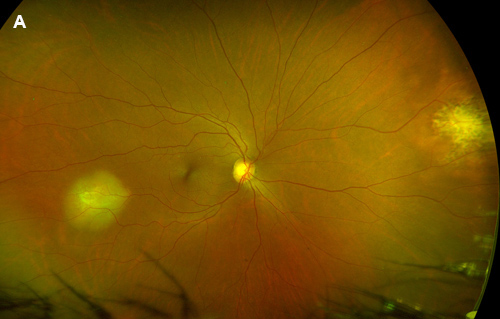
Figure 1A: Wide-field color photo of the right eye. Note the amelanotic lesions in the temporal and nasal periphery

Figure 1B: Color photo of the left eye. Note the amelanotic lesions just superior to the macula. Subretinal fluid is noted extending inferiorly
A 57-year-old woman presented with progressive blurring of her central vision in the left eye for the past year. On examination visual acuity was 20/25 in the right eye and 20/50 in the left eye. Her pupils were equal, round, and reactive with no afferent pupillary defect. Intraocular pressure and anterior segment examination in both eyes were unremarkable. Fundus examination in the right eye revealed two elevated amelanotic choroidal lesions in the periphery. The left eye had similar lesions within the macula (Figure 1A and B). Optical coherence tomography (OCT) through the lesions demonstrated hyperfluorescent subretinal material with adjacent subretinal fluid (Figure 2). Fluorescein angiography showed early mottled hyperfluorescence and late staining (Figure 3). Indocyanine green reflected hypofluorescence in the area of the lesions (Figure 4). Ultrasonography demonstrated a 2.2 – 2.3mm thickening of the posterior eye wall in these areas (not shown).
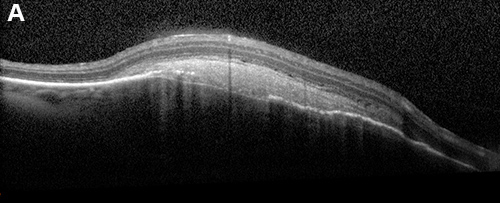
Figure 2A: OCT of the temporal lesion shows a choroidal lesion with overlying subretinal hyperreflective material
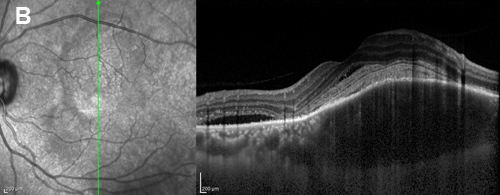
Figure 2B:OCT scan oriented vertically of the left macula lesion shows similar findings in addition to subretinal fluid at the inferior portion.
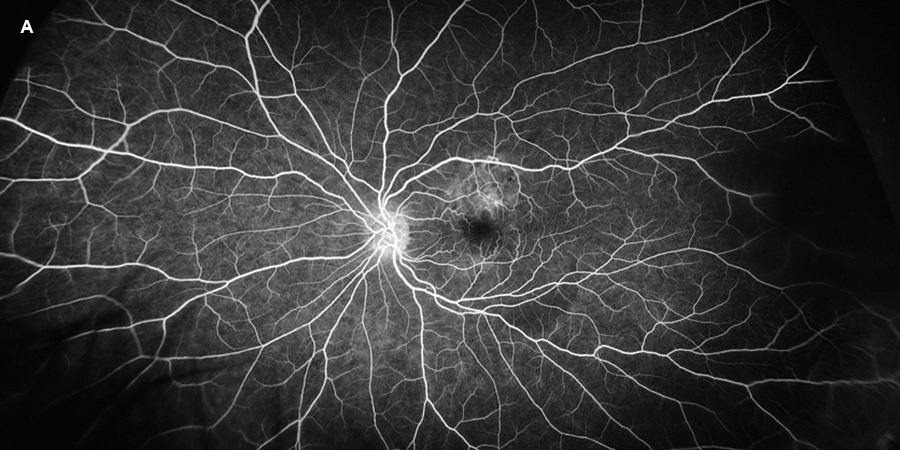
Figure 3A:Early phase fluorescein angiogram of the left eye. Mottled early fluorescence is noted.

Figure 3B:Mid-phase fluorescein angiogram of the left eye. The temporal lesion shows more intense fluorescence. The nasal lesion shows less fluorescence, consistent with the pigment clumping showing that this is likely an older lesion.

Figure 3C:Later phase fluorscein angiogram of the left eye. Note the leakage in from the lesion just superior to the macula.
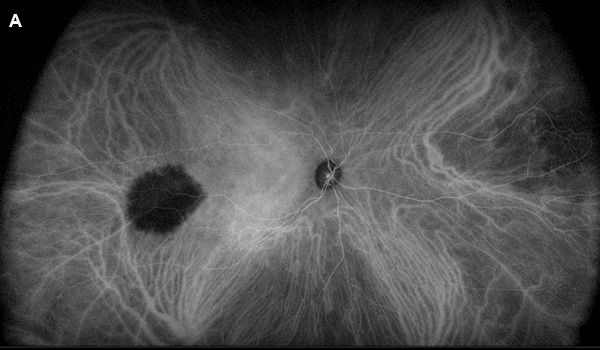
Figure 4A:Wide-field indocyanine angiogram of the right eye. Note that the choroidal lesions are hypofluorescent
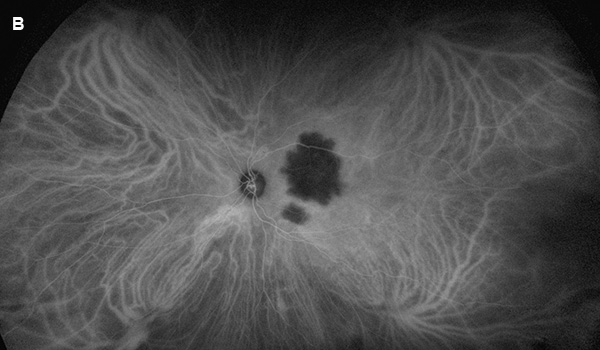
Figure 4B:Wide-field indocyanine angiogram of the left eye. Note that the choroidal lesion is hypofluorescent
Differential Diagnosis
Choroidal metastasis (carcinoma, tuberculoma), Granuloma, Amelanotic melanoma, choroidal osteoma, Multifocal choroiditis, Birdshot chorioretinitis
Upon further questioning patient had a history of hilar adenopathy that was diagnosed five years prior on a CT scan. Her condition has been observed since then. An updated PET scan showed hypermetabolic lymphadenopathy in the cervical, perihilar nodes. A lymph node biopsy is pending. Further laboratory testing included an unremarkable PPD and elevated angiotensin converting enzyme. Taken together, her ethnic background, ocular presentation, and lymphadenopathy strongly suggest a diagnosis of sarcoidosis. A subtenons triamcinolone injection was performed in the left eye which resulted in resolution of the subretinal fluid and improvement in subretinal material (Figures 5 and 6).
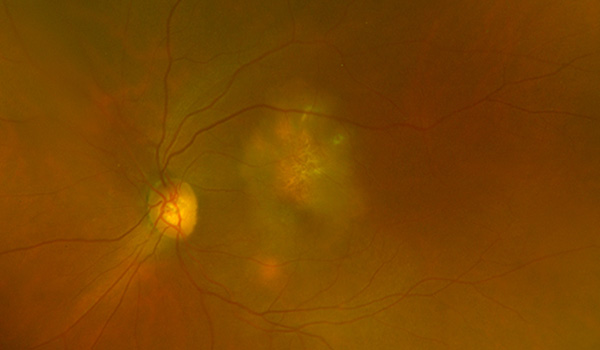
Figure 5:Color photograph of the left macula 3 weeks following a periocular triamcinolone injection. Note the resolution of the choroidal lesion and surround RPE changes.
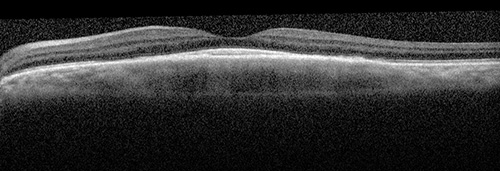
Figure 6:OCT scan shows resolution of the subretinal hyperreflective material and apparent resolution of the choroidal lesion.
Sarcoidosis is a condition of unknown etiology with systemic deposition of noncaseating granulomas that tend to affect the lungs and lymph nodes. Forty percent of patients develop ocular involvement, with anterior uveitis occurring more commonly than posterior uveitis.1 More specifically, funduscopic findings include perivenous exudation with candle wax dripping exudate, pre- and intra-vitreal white nodules in a “string of pearls”, superficial and deep retinal nodules, nodular papillitis, papilledema, optic neuritis, and white masses on the inner retina and optic nerve head.2-4 These lesions are all due to epithelioid cell proliferation. Focal granulomas may develop under the retinal pigment epithelium and within the choroid. These patients lose central vision due to a white choroidal mass in the paracentral vision such as in our patient.1
The finding of candle wax-dripping exudation with preretinal white exudates in the inferior fundus and nodular papillitis are strongly suggestive of sarcoidosis. Patients tend to have elevated angiotensin converting enzyme levels.5 Chest x-ray or CT scan often show hilar lymphadenopathy. Biopsy of the lymph nodes, conjunctiva, salivary gland, or lacrimal gland aids in confirming the diagnosis.6 Branch retinal vein occlusions, central retinal vein occlusions, capillary nonperfusion, retinal neovascularization, vitreous hemorrhage, and neovascularization of the disc may all occur as complications with retinal findings.7 Patients with choroidal involvement may develop subretinal neovascularization and macular detachment.8 Choroidal degeneration and subretinal fibrosis may occur.9 All sarcoid lesions respond to moderately high doses of corticosteroids, with steroid-sparing immunosuppressives required on occasion. More severe cases can also require treatment for multiple mechanism glaucoma and secondary cataract.1