March, 2022
Presented by Braden Burckhard, MD


Presented by Braden Burckhard, MD

A 27-year-old Tunisian male presented with blurred vision in the right eye for the past month.
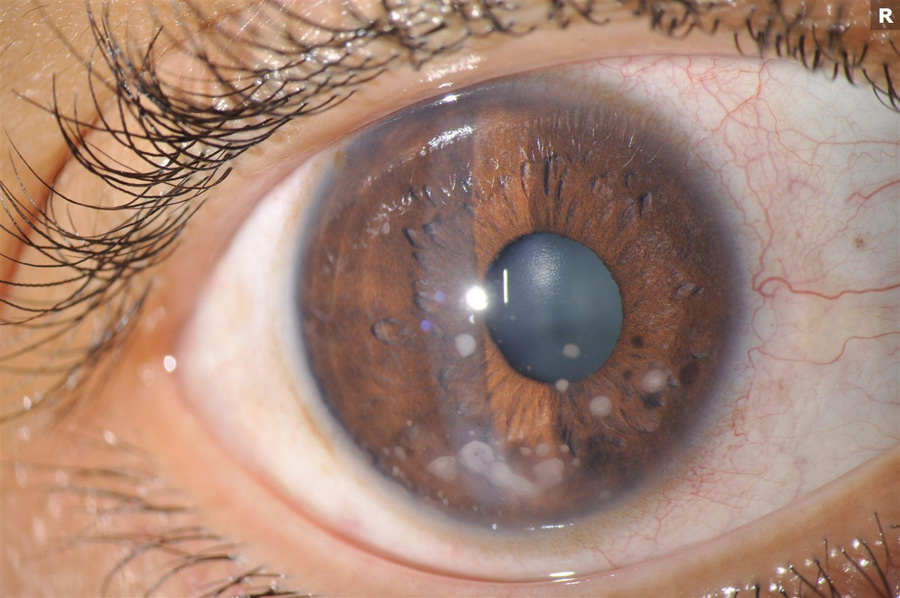
Figure 1A: External photo of the right eye. Note the numerous mutton-fat keratic preciptates (KP).
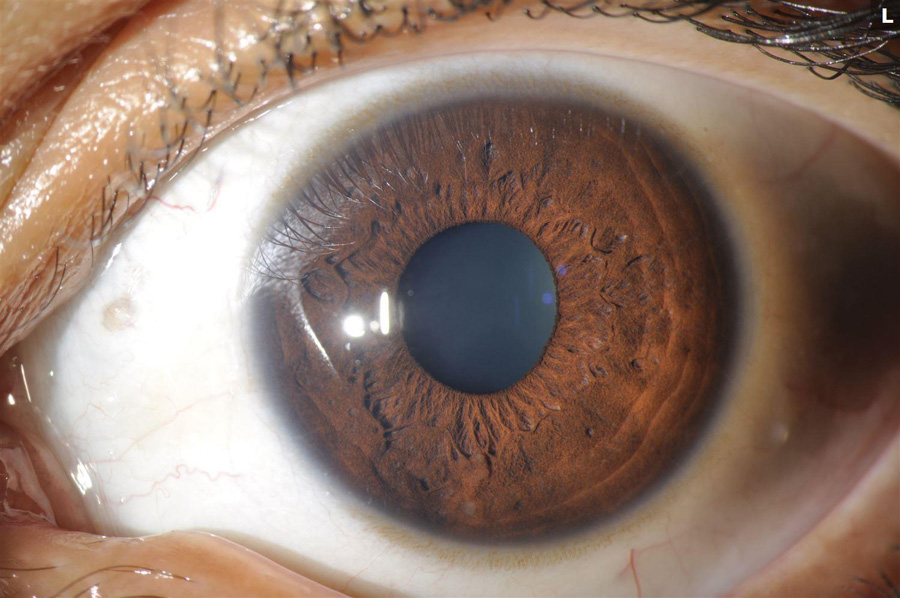
Figure 1B: External photo of the left eye. Less inflammation is present in this eye.
The patient first noticed redness and light sensitivity in both eyes about 3 months earlier. Two months after his initial symptoms, the central vision in the right eye became blurred. He denied having any distortion of images in the right eye or visual changes in his left eye. He had no significant past ocular history. His past medical history and family history were unremarkable. His review of systems was otherwise negative, with no recent upper respiratory symptoms or shortness of breath.
His best corrected Snellen visual acuity measured 20/32 in the right eye (OD) and 20/13 in the left eye (OS). The intraocular pressure was 7 mmHg in the right eye and 8 mmHg in the left eye. Anterior segment examination was remarkable for 2+ cell and granulomatous appearing mutton-fat keratic precipitates in the right eye and 1+ cell in the left eye (Figures 1A and B). There were trace vitreous cells present in both eyes. The funduscopic examination of the right eye showed mild disc hyperemia and edema, vertical striae over the macula, and a subretinal mass temporally with overlying hypopigmentation (Figure 2A). The left eye fundus examination had mild disc hyperemia and similar hypopigmented lesions in the temporal macula (Figure 2B). Fundus autofluorescence (FAF) showed hyperautofluorescence temporally in the right eye with overlying patchy hypoautofluorescence. The left eye FAF demonstrated trace hyperautofluorescence in the superotemporal macula (Figures 3A and B).

Figure 2A: Color photo of the right eye. Note the hyperemic disc, retinal folds in the macula and the elevated lesion in the with the gray-white surface overlying the elevated area in the temporal macula.

Figure 2B: Color photo of the left eye. Multiple areas of deep gray-white lesions of varied sized are seen in the temporal macula. There is some mild disc edema as well.

Figure 3A: Wide-field fundus autofluorescence of the right eye. Note the increased autofluorescence in the temporal macula and periphery.
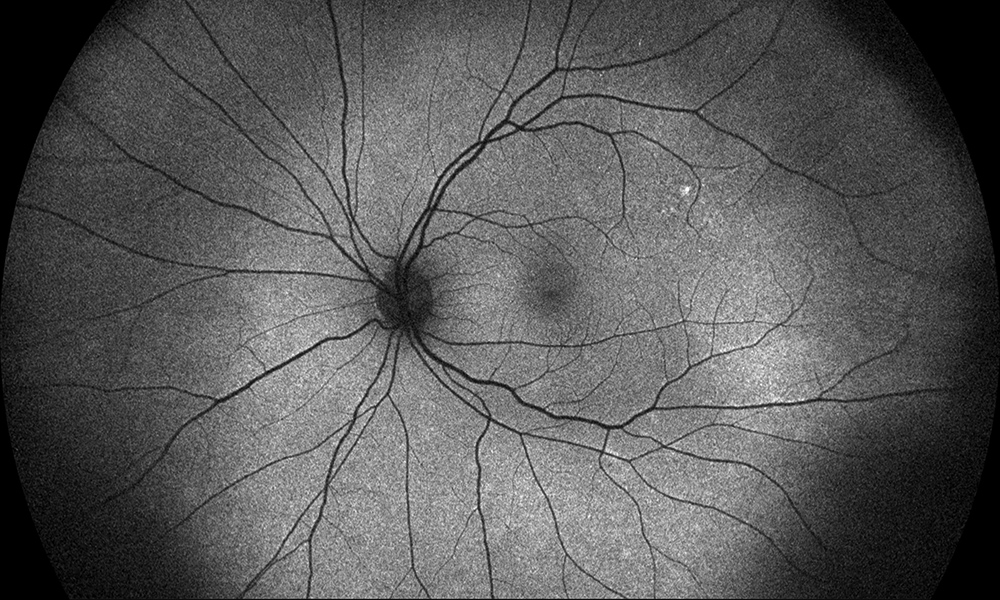
Figure 3B: Wide-field color fundus autofluorescence of the left eye. The temporal retina shows subtle increased autofluorescence.
Fluorescein angiography (FA) revealed hyperfluorescence at the disc in the right eye, with staining of the temporal macula (Figure 4A) and the left eye FA showed mild mottled fluorescence temporally (Figure 4B). Indocyanine green angiography (ICG-A) demonstrated diffuse multifocal hypofluorescent spots in both eyes (Figures 5A and B). Spectral domain optical coherence tomography (SD-OCT) of the right eye revealed a large choroidal mass involving the temporal macula, without evidence of intraretinal or subretinal fluid (Figure 6A). The left eye OCT was unremarkable (Figure 6B). B-scan ultrasonography was performed at the location of this lesion confirming the presence of a choroidal mass that measured 4.12 mm (Figure 7).
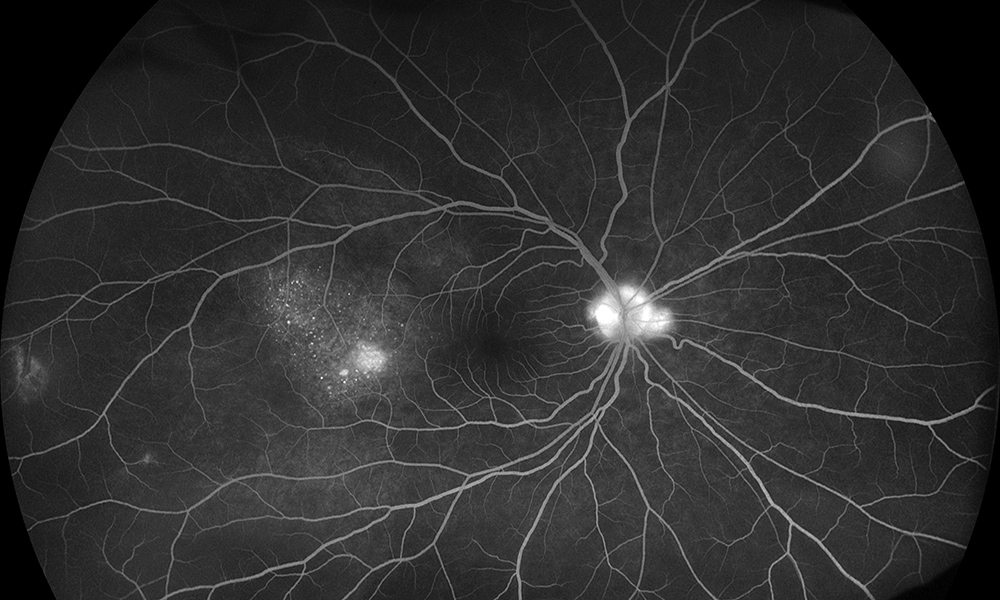
Figure 4A: Wide-field fluorescein angiogram of the right eye. Note the disc hyperfluorescence and the mottled areas of hyperfluorescence temporally in the area of elevation.

Figure 4B: Wide-field fluorescein angiogram of the left eye. Subtle hyperfluorescence is seen in the temporal retina.
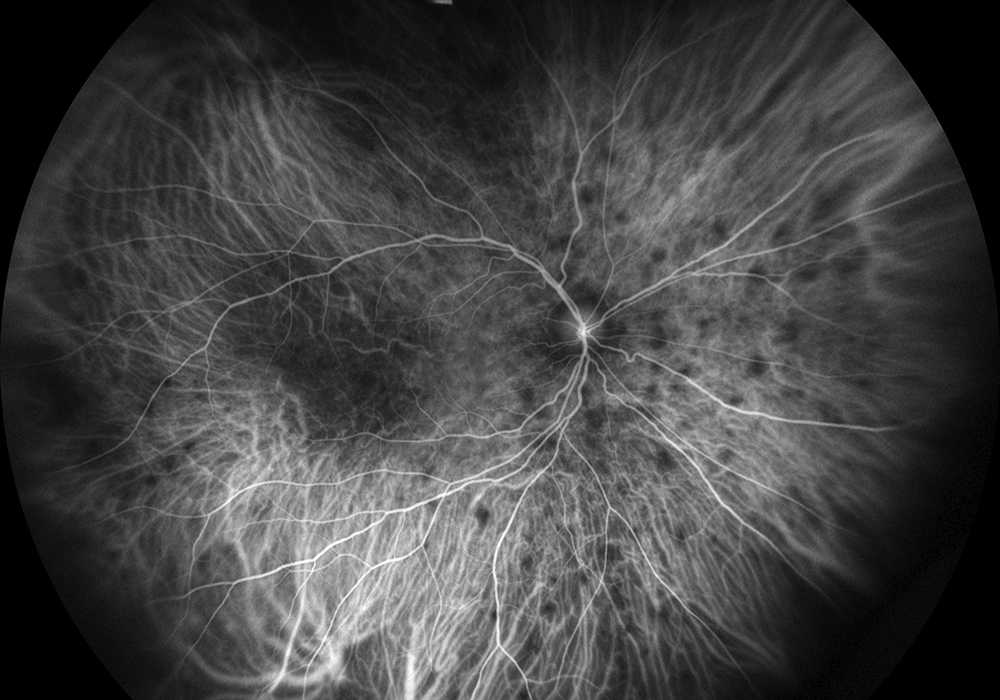
Figure 5A: Wide-field indocyanine angiogram of the right eye. Multiple areas of ~1/2 disc-diameter sized areas of hypoflurescence are seen.
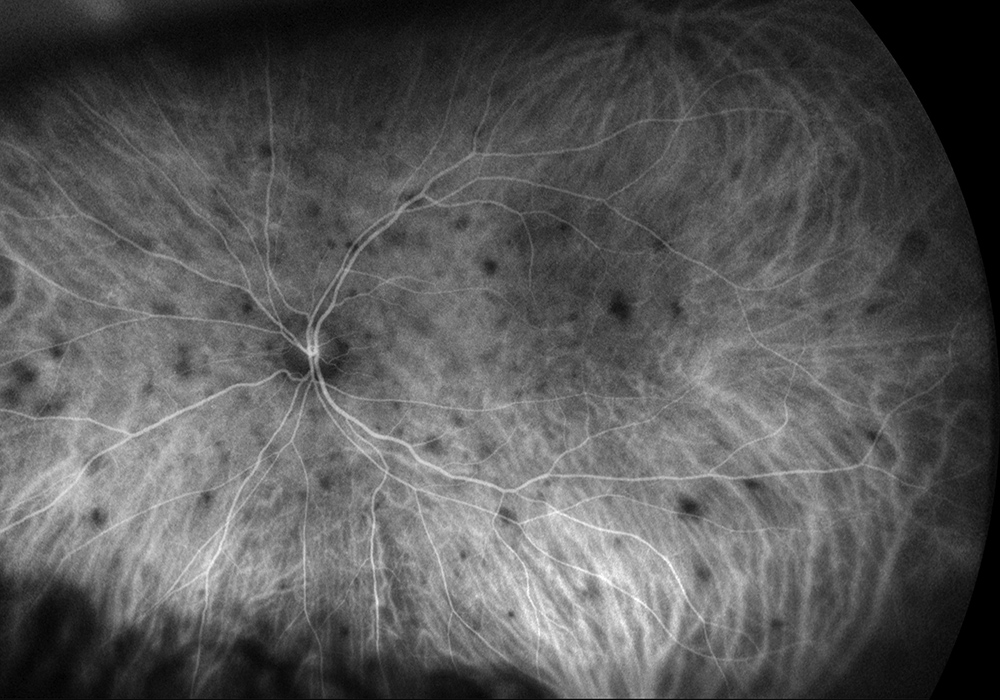
Figure 5B: Wide-field indocyanine angiogram of the left eye. Similar to the right eye, multiple areas of ~1/2 disc-diameter sized areas of hypoflurescence are seen.
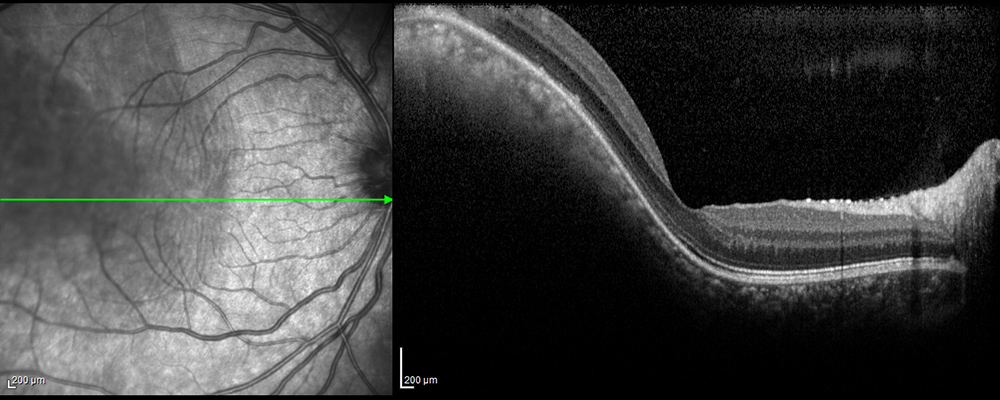
Figure 6A: Spectral domain OCT of the right macula. Note the elevated mass extending into the macula.
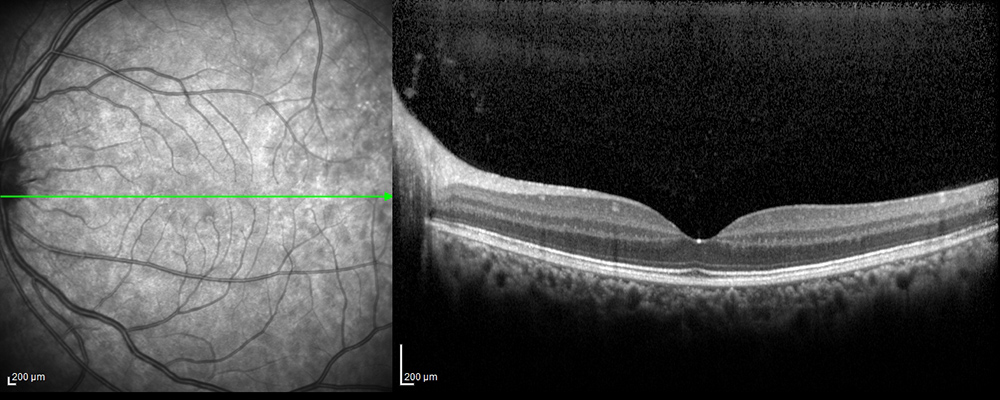
Figure 6B: Spectral domain OCT of the left macula is unremarkable.
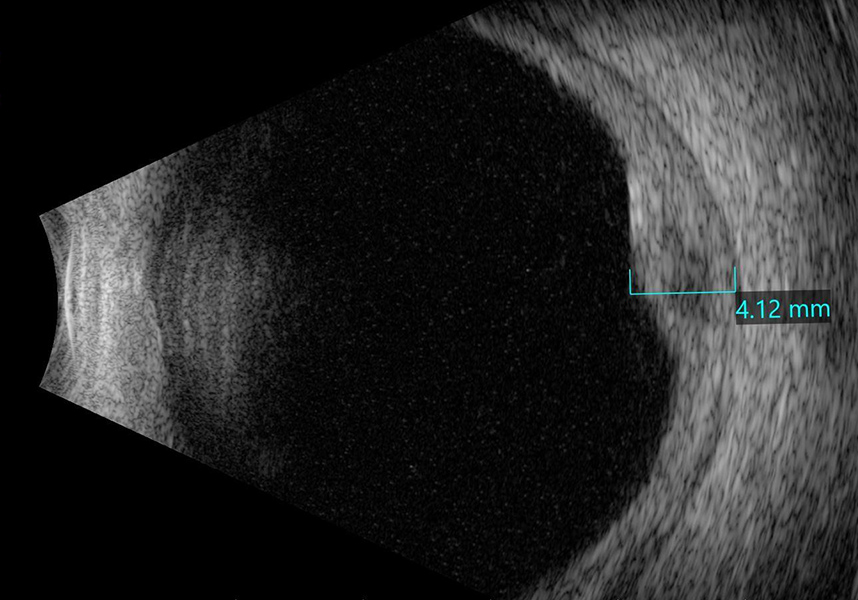
Figure 7: B-scan ultrasound of the right elevated area temporal to the macula shows a solid mass of moderate reflectivity.
Differential Diagnosis
Additional History and Course
The patient was seen by an outside ophthalmologist 11 days prior to his initial visit to our clinic and the following labs obtained: CBC, RPR, FTA-ABS, QuantiFERON-Gold, and a Lyme PCR. All of these labs were normal. The outside provider placed the patient on topical difluprednate four times a day and cyclopentolate three times a day in the right eye and referred him for further evaluation and treatment.
We continued the cyclopentolate and topical steroids in the right eye and added topical steroids to the left eye. The patient was also started on 60 mg of oral prednisone, with the plan to taper to 40 mg in one week. A chest X-ray (CXR) was ordered due to the concern for ocular sarcoidosis and later revealed bilateral hilar lymphadenopathy which further supported our working diagnosis. The patient returned two weeks later with complete resolution of his symptoms and his visual acuity in the right eye had improved to 20/20. The keratic precipitates had resolved and no cell was present on his anterior segment exam in both eyes. His funduscopic exam showed marked improvement in the elevated lesion at the temporal macula (Figures 8 and 9A and B).
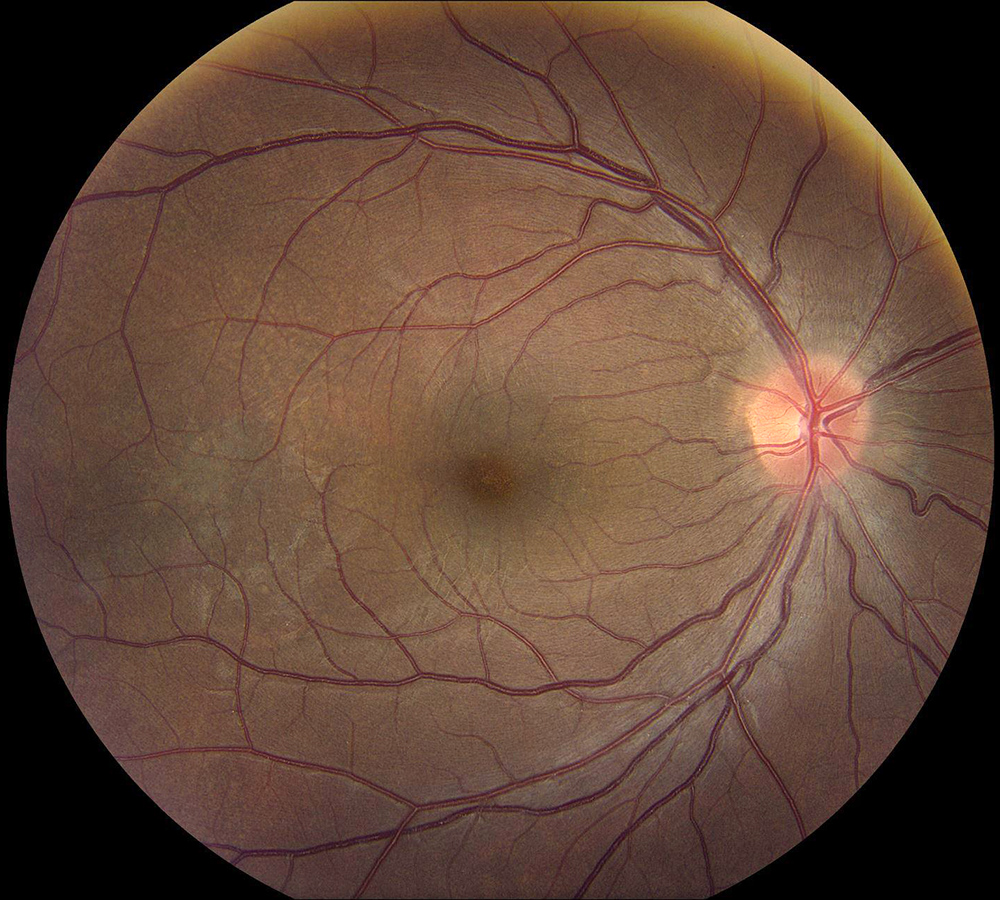
Figure 9: Color photo of the right eye. Note the marked improvement in disc hyperemia, resolution of the retinal folds, and reduction in the height of the temporal lesion.
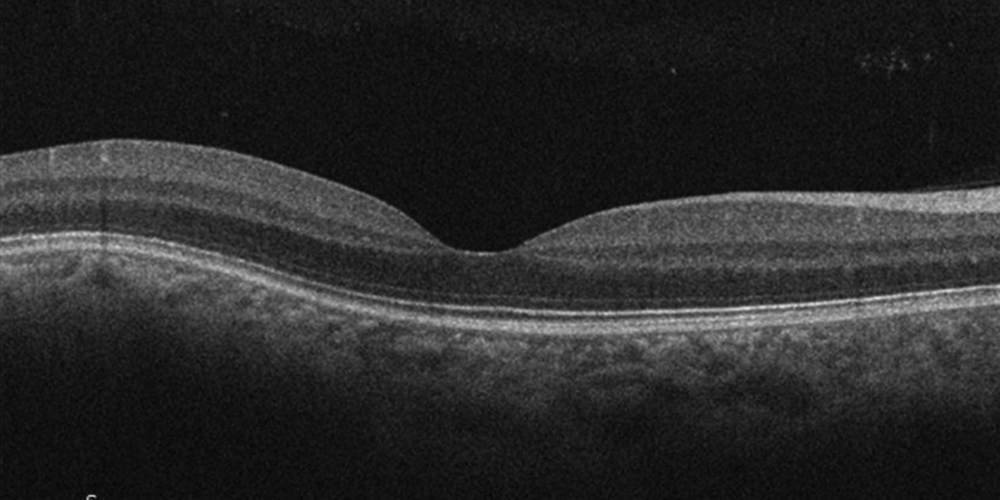
Figure 7: Spectral domain OCT of the right macula. Marked reduction in the elevated choroidal lesion is noted.
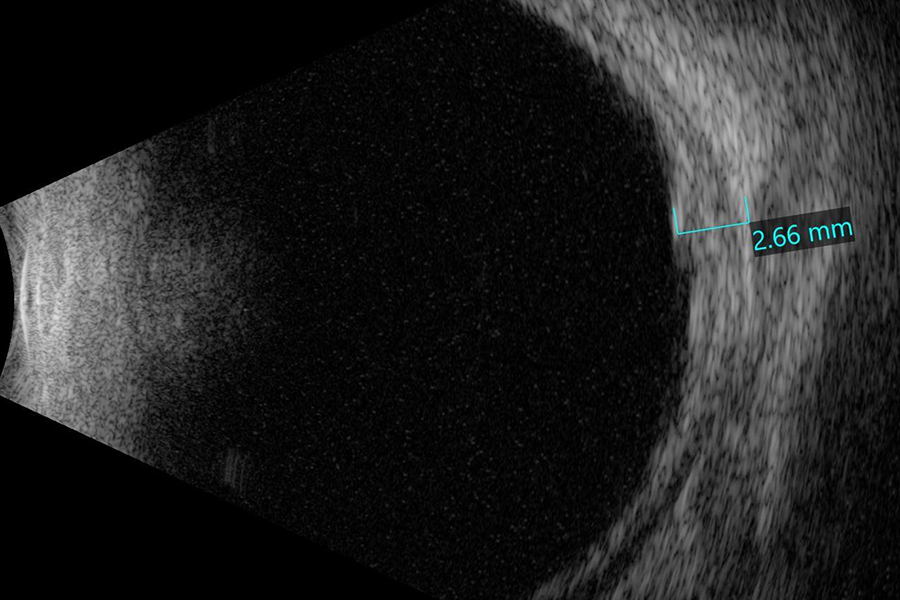
Figure 7: B-scan ultrasound of the right eye shows a significant reduction in the height of the inflammatory leison.
Discussion
Ocular sarcoidosis often presents with multiple ocular manifestations and can involve most structures in the eye and orbit. Uveitis has been reported in 30-70% of sarcoid cases, making it the most common ocular manifestation1. Of the patients with uveitis, bilateral anterior inflammation is most commonly seen, along with some degree of posterior involvement.1 Typical anterior examination findings include anterior chamber cell, granulomatous keratic precipitates, iris or angle nodules, and anterior or posterior synechiae.2 Patients with intermediate uveitis often demonstrate vitreous opacities, snowballs, or snowbanks on examination of the peripheral vitreous and retina.2 Common posterior uveitis findings include periphlebitis, “candle wax drippings,” and choroidal granulomas.3
The diagnosis of ocular sarcoidosis is based on a combination of clinical findings, laboratory testing, imaging, and confirmatory biopsy. Tissue biopsy is the gold standard for the diagnosis of “definite” ocular sarcoidosis when uveitis is present, but if not performed, a combination of other diagnostic criteria can be used to support the diagnosis. In 2017, the International Workshop on Ocular Sarcoidosis (IWOS) published criteria for diagnosing ocular sarcoidosis based on seven clinic signs, eight systemic investigation results, and three diagnostic criteria listed below:4
Revised International Workshop on Ocular Sarcoidosis (IWOS) criteria for the diagnosis of ocular sarcoidosis (OS):
Our patient's exam was significant for mutton-fat keratic precipitates, iris (Bussaca) and trabecular meshwork (Berlin) nodules (Figure 1), a solid choroidal nodule, bilateral anterior and posterior involvement, a positive CXR, and a negative TB test. Based on the criteria established above, the combination of these findings is consistent with the diagnosis of “presumed” ocular sarcoidosis. The main line of treatment in ocular sarcoidosis is corticosteroid therapy. Our patient responded promptly to oral prednisone with resolution of symptoms and significant improvement of his exam after just two weeks of treatment. Immunosuppressive or biological agents may be used for long-term management in patients that require prolonged use of systemic steroids to control their inflammation.