November, 2021
Presented by Braden Burckhard, MD


Presented by Braden Burckhard, MD

A 23 year-old female reported a 2 week history of increased scleral pigmentation following routine primary vitrectomy for repair of retinal detachment.
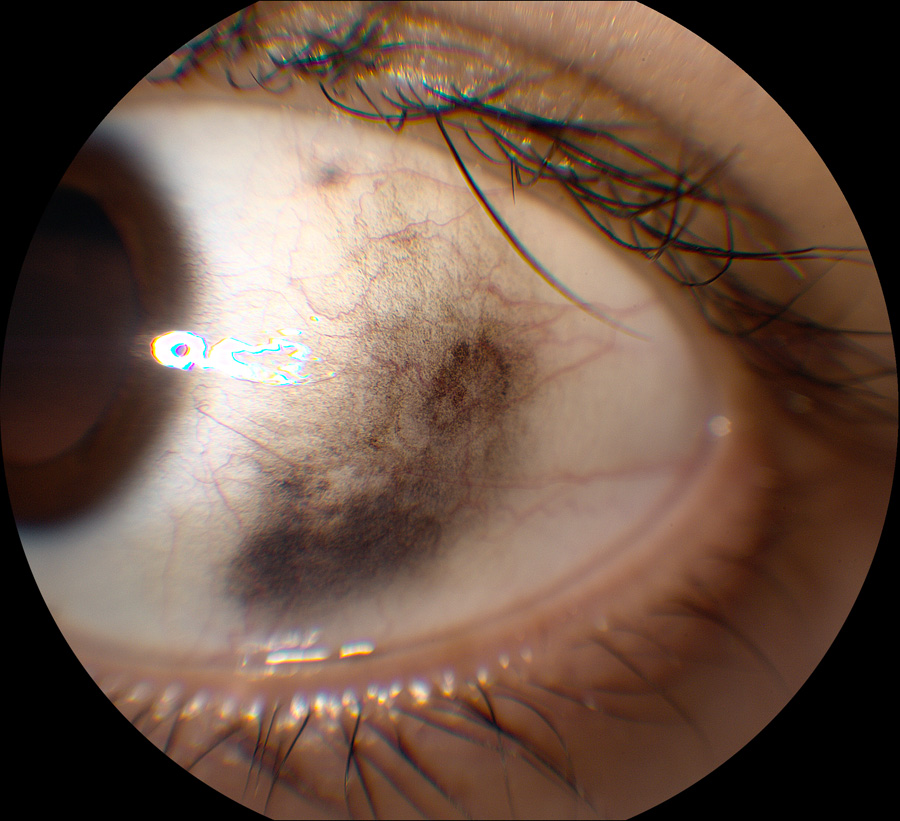
Figure 1: Anterior segment photo of the left eye. Note the area of conjunctival pigmentation
Two weeks earlier, the patient presented with an inferior visual field defect in the left eye that had worsened over a three day period, eventually involving her central visual field. Her past ocular history is significant for high myopia (>16 diopters), lattice degeneration, and previous laser photocoagulation of retinal tears in both eyes. She underwent bilateral medial rectus recessions for an existing esotropia one month prior to this presentation. She has been taking latanoprost and combigan drops in the left eye only, due to a history of steroid-induced ocular hypertension. She has a past medical history of depression, anxiety, and Marfan-like Syndrome. Her systemic medications include clonazepam, sertraline, and drospirenone/ethinyl estradiol tablets. Her review of systems was otherwise unremarkable.
Her Snellen visual acuity measured 20/20 in the right eye (OD) and 20/50 in the left eye (OS). Her intraocular pressure was 18 mmHg in both eyes (OU). Anterior segment examination showed remnants of vicryl suture in the conjunctiva of both eyes from her recent strabismus surgery but was otherwise unremarkable. She was phakic, without any evidence of cataract in each eye. The funduscopic examination of the right eye was significant for scattered areas of treated lattice degeneration. There was also a treated retinal tear located superonasally, just posterior to the scatter laser. The left eye showed a fovea involving, rhegmatogenous retinal detachment extending from 11:00 to 2:30, as well as peripheral lattice degeneration and scattered laser. Spectral domain optical coherence tomography (SD-OCT) confirmed a fovea-off retinal detachment.
The patient underwent 25-gauge pars plana vitrectomy (PPV) with endolaser and tamponade with 16% C3F8 one day later. A combined vitrectomy and scleral buckle procedure was initially recommended but she wanted to proceed without the scleral buckle, due to the recent success of her strabismus surgery. The surgery was completed uneventfully and the patient had a normal post-operative course until 2 weeks after her surgery, when she had noticed progressive increased pigmentation over the “white part of her left eye” (Figure 1). The pigmented lesion was found to be mobile on examination, without evidence of sentinel vessels. Upon further questioning, she denied having any abnormal pigmentation of her eye prior to her vitrectomy surgery. She also denied a history of melanoma, unusual pigmented lesions of her skin, or abnormal amounts of UV exposure. She did admit to having 15-20 skin tattoos and she states her race is half Latin and half Caucasian.
Differential Diagnosis
The patient was observed without further treatment for the increased pigmentation of her eye. She continued her routine post-operative follow up appointments until about 2.5 months after her surgery, when she presented for new vision loss in her operative eye. On examination she was found to have a recurrent rhegmatogenous retinal detachment involving the macula. The following day she underwent repeat 25-gauge PPV with endolaser and silicone oil placement. A peritomy was made prior to vitrectomy, with careful inspection of the pigmented region shown in the previously shown photo. Most of the pigment was confined to Tenon’s capsule with a small amount of pigment visible at the trochar site located within the sclera surrounding the incision. The other trochar sites had a similar appearance, but with no pigment in the overlying Tenon’s capsule. A majority of the inferotemporal pigmented Tenon’s was excised and sent for pathology. The histology of this specimen showed heavily pigmented epithelioid cells, likely representing melanin-laden macrophages (Figure 2). Immunohistochemical stain for melanocytes (S100 and Mart-1) were performed but no definite staining was seen to support the presence of melanocytes.

Figure 2:Histology of excised specimen demonstrating pigment-laden macrophages. Immunohistochemical slides no melanocytes.
Discussion
The occurrence of this pigmentation following surgery and the absence of melanocytes on histology is suggestive that our patient had PPV-associated prolapse of pigment through the sclerotomy sites. Similar pigmentation related to pars plana sclerotomies has been previously documented by Park et al.3 In their study, conjunctival pigmentation was seen after surgery within 7 days postoperatively in eight of 185 eyes undergoing 23-gauge PPV. Light microscopy of excised tissue in these eye showed infiltration of abundant dark-brownish colored melanophages with surrounding, finely granular, melanin pigments 3 (Figure 4 – Park external photo and histology photo). All of the sclerotomies from these study patients were closed with 8-0 nylon sutures in a hemi-bow tie fashion and patients were placed on topical ofloxacin and prednisolone acetate post-operatively for one and four weeks, respectively.3 All of the sutures were released at the slit-lamp one day after surgery 3. They noted that tamponade with C3F8 gas was significantly associated with conjunctival pigmentation (OR, 9.4; 95% CI, 1.9–44.5; P = 0.005) 3. Post-operative leakage or hypotony was not identified in any of the cases showing increased pigmentation 3. They hypothesized that intraocular melanin prolapsed through the sclerotomy sites and that the origin of the pigment was likely from RPE cells, because the three eyes with the most significant accumulation of pigment came from eyes that had retinal tears.3 No pigmentation accumulation was identified in eyes that had epiretinal membrane, macular hole, or non-diabetic vitreous hemorrhage surgery 3. They proposed that the lack of pigment in these patients resulted from vitreous plugging at the sclerotomy sites from a less thorough vitreous base dissection during surgery.3
Similar findings of post-operative pigmentation have been described by Smiddy et al, who also reported dark brown pigmentation at the episclera and conjunctiva following 20-gauge conventional vitrectomy and retinal re-attachment surgery.4 Light and electron microscopic studies demonstrated melanin granules extracellularly and within macrophages in the biopsied tissue4. Liu et al also described similar histology after 20-gauge standard vitrectomy.5
Our patient stated she was half-Caucasian and half-Latina. Currently, no racial association has been identified with the development of post-operative conjunctival or subconjunctival pigment. The patient also underwent recent strabismus surgery prior to her initial vitrectomy, however, only the medial recti muscles were involved in the procedure and the majority of the pigment seen in our patient was located inferotemporally, where there were no sutures or manipulation of the recti muscles.
In summary, our patient developed a large area of subconjunctival pigmentation in the inferotemporal quadrant after undergoing PPV where a retinal tear was involved and C3F8 was used. The etiology of this pigment is likely from intraocular melanin that prolapsed through the sclerotomy sites during or after vitrectomy. These findings are consistent with previous reported cases.3-5